Introduction
Detection of incidental prostate cancer by transurethral resection of the prostate (TURP) has decreased with the introduction of prostate-specific antigen (PSA) screening [1]. Although there is a controversy regarding which treatment is appropriate in cases of incidental detection of prostate cancer, radical prostatectomy (RP) remains a commonly performed treatment [2, 3].
It is generally recommended that RP be performed at 12 weeks after TURP, presumably to allow for resolution of inflammatory adhesions so that the anatomy between the prostate and the surrounding structures returns to a nearly normal state before surgery. However, there was no convincing data to support this recommendation. During the past decades, laparoscopic radical prostatectomy (LRP) has become a more commonly performed procedure for the treatment of localized prostate cancer [4]. Laparoscopic radical prostatectomy has the advantages of clearer fields of vision, better preservation of anatomical structures, a shorter period of convalescence and less blood loss compared with open RP [5]. To our knowledge, there is a lack of published data whether LRP performed within 12 weeks after TURP was associated with surgical difficulty or outcomes. The present study aims to bridge this gap in the existing literature.
Material and methods
After obtaining Institutional Review Board approval, we retrospectively reviewed the records of prostate cancer, and included the patients diagnosed at TURP who had undergone LRP between July 2009 and December 2017. We excluded prostate cancer patients detected with prostate biopsy for PSA rising during the post-TURP follow-up, and men who had adjuvant neoadjuvant endocrine therapy were also excluded. The clinical, pathologic and follow-up data were collected to determine whether the interval from TURP to LRP affected the surgical difficulty or outcomes.
We stratified the patients into two groups according to the interval between TURP and LRP: patients with intervals ≤ 12 weeks and those with intervals > 12 weeks. The age, body mass index (BMI), PSA level before TURP, Gleason score at TURP, operative duration, estimated blood loss (EBL), postoperative length of stay, pathologic Gleason score, complications, Gleason score upgrading, margin status, major complications, postoperative urinary incontinence and PSA recurrence were compared between the 2 groups. Laparoscopic radical prostatectomy was performed by 1 of 2 senior urologists. We used post-operative drop in hemoglobin (preoperative hemoglobin minus post-operative hemoglobin 1 day after surgery) instead of surgeon-reported estimated blood loss. Patients were considered as having continence if they occasionally leaked a few drops with abdominal straining and if they needed to use only one protective pad a day at 6 months after LRP. Prostate-specific antigen recurrence was defined as follow-up PSA level > 0.2 ng/ml.
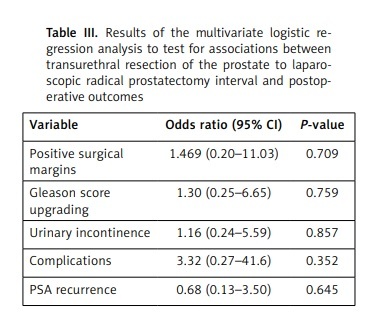
The independent t-test, χ2 and Fisher’s exact test were used to compare the clinical and pathologic variables of patients undergoing LRP across the TURP-to-LRP interval. The multivariate linear regression model was used to examine the effect of the interval between TURP and RP on EBL, operative duration and length of postoperative stay. In addition, we carried out multivariable logistic regression analyses to determine whether the interval from TURP to LRP independently affected the positive surgical margins, Gleason score upgrading, complications, urinary continence and PSA recurrence. We adjusted for potential confounding factors of patient age, BMI, pre-TURP PSA level, and pathologic Gleason score in the analysis.
Results
Overall, a total of 56 incidental prostate cancer patients detected by TURP who underwent LRP in our institute were included in this study. The mean age and pre-TURP PSA level were 67.6 ±5.7 and 5.7 ±3.6 ng/ml, respectively. Three patients had no residual tumor identifiable in the prostate. Grade of disease ranged from Gleason 3 + 3 = 6 to Gleason 5 + 4 = 9. The positive surgical margin was found in 7 patients. Eight patients developed complications, including pelvic hematoma in one, urine leakage in two, lymphocele formation in three, deep vein thrombosis in one and urethrorectal fistula in one. Forty-five patients were continent at 6 months after RP. Ten patients developed a PSA recurrence, and no patients died during the follow-up.
In all, 38 patients had LRP at > 12 weeks (17.3 ±5.6 weeks) after TURP, and 18 at ≤ 12 weeks (8.4 ±2.5 weeks). There was no significant difference in patients’ age, BMI, pre-TURP PSA level, Gleason score at TURP, operative duration, EBL, pathologic Gleason score, length of postoperative stay, rate of Gleason score upgrading, positive margin, complications, urinary incontinence at 6 months after surgery, or PSA recurrence between the ≤ 12 and > 12 weeks subgroups (Table I). The TURP to LRP interval was not an independent predictor of EBL, operative duration, length of postoperative stay, positive surgical margins, Gleason score upgrading, complications, urinary incontinence, or PSA recurrence in multivariate linear or logistic regression analysis (Tables II and III). No correlation was found between the TURP to LRP interval and surgical outcomes during or after LRP.
Table I
Comparison of preoperative clinical variables, pathologic and follow-up outcomes according to interval between transurethral resection of the prostate (TURP) to laparoscopic radical prostatectomy (LRP)
Table II
Results of the linear regression analysis to test the association between transurethral resection of the prostate to laparoscopic radical prostatectomy interval and outcomes during and after surgery
| Variable | Point estimate (95% CI) | P-value |
|---|---|---|
| EBL [g/l] | −0.15 (−7.80, 7.50) | 0.968 |
| Length of postoperative stay [days] | −0.97 (−4.06, 2.12) | 0.530 |
| Operative duration [min] | −13.07 (−47.72, 21.60) | 0.453 |
Table III
Results of the multivariate logistic regression analysis to test for associations between transurethral resection of the prostate to laparoscopic radical prostatectomy interval and postoperative outcomes
Discussion
With the introduction of PSA screening, incidental prostate cancer was diagnosed in less than 5% of patients who undergo benign prostatic hyperplasia-related surgery [6, 7]. The most appropriate management of incidental prostate cancers diagnosed at TURP has been debated [8]. European Association of Urology guidelines recommend active surveillance for stage T1a and radical prostatectomy for stage T1b patients with a life expectancy of more than 10 years [9]. In our study, the mean PSA was higher; hence there was a greater possibility that these incidental prostate cancers would be locally advanced prostate cancer rather than “true” incidental prostate cancer. As the concept of active surveillance is not widely accepted in China, most patients with incidental prostate cancer after TURP will undergo RP.
Many studies have described the procedure as being more difficult after TURP [10]. Perforation of the prostatic capsule during TURP with extravasation of blood and irrigation fluid can lead to periprostatic fibrosis and distortion of the surgical planes. Bladder neck sparing can seldom be performed, and neurovascular bundle (NVB) preservation is technically more difficult, ultimately compromising postoperative continence and erectile function [11]. In the era of open RP, the TURP to LRP interval has been recommended as at least 12 weeks to allow adequate time for complete resolution of inflammation [12]. However, the reason for this recommendation is not yet clear. It may originate from clinical experience of urologists with challenging cases after a short interval to TURP. In the last decades, LRP has become a common option for the treatment of prostate cancer and represents a new experience for urologists. However, tissue adhesion is also considered to be one of the factors that make the laparoscopic surgery more difficult [13]. In actual clinical practice, urologists often encounter patients who choose RP and request surgery as soon as possible. For such patients, our results showed that LRP performed within 12 weeks did not affect surgical difficulty, such as operative duration, EBL and major complications, suggesting that patients could safely proceed to LRP shortly after TURP. Although insignificant, we noted that the complications rate in patients with an interval below 12 weeks was obviously higher than in those with an interval above 12 weeks (18.4% vs. 5.6%). It could be speculated that this difference might become significant if more patients were enrolled.
Because such tumors are often perceived to be of low volume and clinically insignificant, and several therapeutic options are available, some patients would need a long time to finalize their decision when choosing a primary treatment for incidental prostate cancer. Our results indicated no significant differences in rate of positive margin, Gleason score upgrading, urinary incontinence or PSA recurrence in patients with TURP to RP intervals above and below 12 weeks, suggesting that patients choosing delayed treatment were not at risk of disease progression and the surgical efficacy was not affected by a longer TURP to LRP interval.
To the best of our knowledge, this is the first study comparing incidental prostate cancer patients of TURP-to-LRP interval ≤ 12 weeks with those > 12 weeks. Although all patients had LRP in this analysis, these findings may be applicable to open RP or robotic-assisted LRP. As with TURP, it is a widely accepted practice to wait at least 6 weeks after prostate biopsy before RP to allow for resolution of inflammation and bleeding caused by biopsy [14]. However, consistent with the present study, previous work also showed no significant association between biopsy-to-surgery interval and perioperative outcomes [15, 16].
There are several limitations to our study that warrant discussion. First, our study had a relatively small sample size, especially for the patients with an interval below 12 weeks. More patients need to be included to improve the statistical power. Second, it is retrospective in nature, so there may be confounding variables that are unaccounted for. A prospective analysis with different intervals can allow for a better definition of a minimum and an optimum TURP to LRP interval. Third, our data are from a single institution. Some of our findings might be specific to surgical techniques or patient selection, and therefore may have less applicability elsewhere. Last, the post-operative erectile function was not analyzed, as we did not preserve the NVBs intraoperatively, and that would require a longer follow-up and standardized instruments, which were not used to assess erectile function in these patients.
In conclusion, our study showed that TURP-to-LRP interval did not affect surgical difficulty or outcomes. This may provide reassurance for either the urologists or patients contemplating LRP soon after TURP. However, our results need to be further confirmed in large prospective studies.