Multiple endocrine neoplasia type 1 (MEN1) syndrome, also known as Wermer’s syndrome, is a rare, autosomal dominant inherited syndrome caused by mutations in the MEN-1 tumor suppressor gene [1, 2]. The estimated prevalence of MEN1 syndrome is 1 : 30,000 in the general population [1]. This low frequency is the main reason for the rarity of controlled clinical trials. Patients can be diagnosed with MEN1 when 2 or more primary endocrine tumors, including pituitary tumors, pancreatic tumors, and parathyroid adenomas, are present. Among them, the most common pathological type is parathyroid adenoma with primary hyperparathyroidism (HPT).
MEN1 with HPT is characterized by asynchronous and asymmetrical growth of the parathyroid glands. Ectopic parathyroid adenomas can also be observed in MEN1 patients, which can be easily misdiagnosed. In the present case, we report a man with persistent HPT, who was diagnosed with MEN1 based on the results of a genetic study. He was found to have an ectopic parathyroid adenoma in the retroesophageal region, which was the main gland to affect HPT.
We present a case of a 66-year-old man, with a history of renal lithiasis for 42 years. Forty-two years ago, the patient was diagnosed with renal lithiasis due to the symptoms of renal colic and hematuresis. From then on, renal colic and hematuresis recurrently attacked for many years. But the only treatment strategy the patient received was the use of drugs to relieve the pain.
In November 2018, at 63 years of age, the patient was admitted to our hospital due to recurrent renal colic. The laboratory evaluation showed that the serum calcium concentration was 3.14 mmol/l (reference range: 2.2–2.7 mmol/l), the serum phosphorus concentration was 0.30 mmol/l (reference range; 0.8–1.6 mmol/l), and the intact parathyroid hormone (PTH) level was 376 pg/ml (reference range: 18.5–88.0 pg/ml). Methoxyisobutyl isonitrile (MIBI) showed that the region below the left thyroid gland had an abnormal increase of radioactivity, consistent with the features of HPT. Abdominal computed tomography (CT) and abdominal ultrasound revealed that many calculi were located in the gallbladder and both kidneys. Pituitary magnetic resonance imaging (MRI) did not find any abnormality. Aforementioned medical data posed a high clinical suspicion of primary HPT. Thus, parathyroid surgery was suggested to the patient, but he refused the surgical treatment after consulting his family.
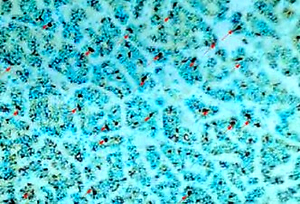
In July 2020, the patient felt pain of the ankles and heels. He was admitted to a local hospital. The laboratory evaluation showed a serum calcium concentration of 2.93 mmol/l (reference range: 2.11–2.52 mmol/l), a serum phosphorus concentration of 0.6 mmol/l (reference range: 0.84–1.54 mmol/l), and a PTH level of 243 pg/ml (reference range: 18.5–88.0 pg/ml). The blood gastrin level was within the normal range. A calcimimetic (25 mg, once a day for 21 days) was used to treat the hypercalcemia caused by HPT. But this treatment did not have a good effect. After 1 month of calcimimetic treatment, the serum levels of calcium and PTH did not decrease significantly. On 18 January 2021, a cervical ultrasound scan revealed a hypoechoic nodule below the left thyroid gland. Parathyroid hyperplasia was suggested. Thus, the patient received parathyroid surgery on 20 January 2021 and the left inferior parathyroid gland was removed. The postoperative pathology showed that the removed tissues were nodular hyperplasia (Figure 1). Aforementioned medical data suggested that the HPT of the patient was caused by parathyroid adenoma. But the surgery did not improve the patient’s condition well. The serum calcium was 2.62 mmol/l, and the PTH level increased to 762.2 pg/ml after surgery.
Figure 1
The removed left inferior parathyroid gland was nodular hyperplasia (hematoxylin-eosin staining, 100× magnification). The red arrow indicated the tumor tissue, and the black arrow indicated normal healthy tissue
In February 2021, the patient felt that the pain of the ankles and heels was aggravated. He was admitted to our hospital for further treatment. The laboratory evaluation showed a serum calcium concentration of 2.66 mmol/l, a serum phosphorus concentration of 0.40 mmol/l, and a PTH level of 459 pg/ml. The blood gastrin level was 10.32 pg/ml, within the normal range. Bone densitometry showed osteoporosis (T score: –1.8 in the lumbar spine, –1.8 in the femoral neck). The chest CT in another hospital showed that a soft tissue mass was located on the left rear side of the esophagus with a size of 2.5 × 1.6 cm. The properties of the mass were undefined.
The two sons of the patient were diagnosed with parathyroid adenoma with HPT earlier, and received surgery to remove all four parathyroid glands. In addition, the younger son of the patient was also diagnosed with gastrinoma and prolactinoma. Other close relatives of the patient were generally healthy without apparent health issues such as endocrinopathies or tumor. Based on the clinical symptoms and family history, the diagnosis of MEN1 syndrome was highly suspected. Then, a genetic study was carried out. The patient and his two sons were confirmed to be carriers of a novel mutation variant of the MEN1 gene. Analysis of the MEN1 gene coding region revealed a heterozygous mutation (variant c.200_201insAGCCC:p.D70Pfs) in exon 2. Thus, the diagnosis of MEN1 syndrome was finally made. The mass on the neck was highly suspected as an ectopic parathyroid adenoma. Thus, surgery of cervical exploration was suggested to the patient. But considering the patient had undergone cervical surgery not long ago, cervical exploration was not performed immediately.
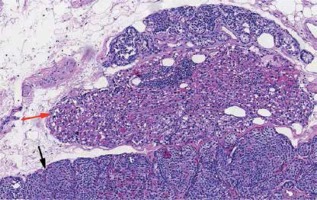
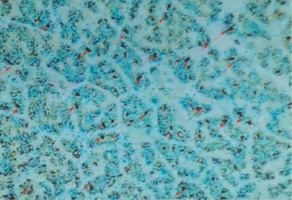
In May 2021, the patient underwent surgery of cervical exploration. During the procedure, a 4 × 2 × 1.3 cm hardened mass was found in the left rear side of the esophagus (Figure 2). The surgeon removed the mass with surrounding fatty tissue. The pathology study showed that the removed tissues were hypercellular parathyroid tissue, compatible with parathyroid adenoma. The cells had no atypia with positivity for PTH (Figure 3), CK19, CgA and Ki-67 3%. Based on these findings a diagnosis of MEN1 syndrome with ectopic parathyroid adenoma was made. After the surgery, serum calcium concentration of the patient was 2.45 mmol/l (reference range: 2.2–2.7 mmol/l), and the PTH level was 80.0 pg/ml (reference range: 18.5–88.0 pg/ml).
Figure 3
The pathology study showed that the mass in the left rear side of the esophagus was hypercellular parathyroid tissue, compatible with parathyroid adenoma (immunohistochemical staining for PTH, 100× magnification). The cells had no atypia with positivity for PTH (red arrows). PTH immunoreactivity was assessed using standard immunohistochemistry methodology. In short, formalin-fixed, paraffin-embedded tissue was cut into 4 μm sections. Then sections were incubated with anti-PTH at 1 : 200 dilution (NCL-PTH-488, Leica Biosystems; Wetzlar, Germany) at 4°C overnight, followed by a secondary antibody at 1 : 200 dilution (B-200, Vector Laboratories, Burlingame, CA, USA) for 45 min at room temperature. Immunoreactivity was visualized by the avidin-biotin-peroxidase complex method
Clinically, MEN1 is usually diagnosed when a patient presents with two or more MEN1-associated tumors (such as parathyroid adenomas, entero-pancreatic tumors, and pituitary adenomas) [3]. But diagnosis can also be made when a patient has a MEN1-associated tumor and a first degree relative with MEN1 or when a person has a MEN1 mutation [4, 5]. In the present case, the patient only presented a MEN1-associated tumor (parathyroid adenoma). But his sons were clinically diagnosed with MEN1, and the genetic study revealed a novel mutation variant of the MEN1 gene. Analysis of the MEN1 gene coding region showed a heterozygous mutation (variant c.200_201insAGCCC:p.D70Pfs) in exon 2. Thus, the diagnosis of MEN1 of the patient was made on the basis of clinical, familial, and/or genetic criteria [4, 6].
Currently, more than 1300 mutations have been detected in the MEN1 gene region. These mutations could result in a loss of a functional tumor-suppressor protein called menin, leading to unregulated cell division and tumor growth in susceptible tissues [7]. Parathyroid adenoma is the most common type of MEN1, and HPT is the most common and first manifestation [8]. In this case, the patient presented persistent HPT for a long time. The hypercalcemia caused by HPT made the patient develop symptoms such as renal lithiasis and bone pain. After the first surgery to remove the left inferior parathyroid gland, the patient’s condition did not improve. The serum calcium and the PTH level were not decreased after surgery. This result indicated that other factors might exist to affect HPT. Fortunately, 1 month after the surgery, a mass was found on the left rear side of the esophagus by CT. An ectopic parathyroid adenoma was highly suspected. The patient underwent the second surgery, and the pathology study confirmed the diagnosis of ectopic parathyroid adenoma.
HPT due to ectopic parathyroid adenoma is extremely rare, with a few published case reports [9, 10]. It has been reported that the most common ectopic parathyroid site is the thymus, followed by retroesophageal and intrathyroidal regions [11]. A few previous studies have reported MEN1 patients with ectopic parathyroid glands. Tonelli et al. reported a 16-year-old male patient diagnosed with MEN1 affected by severe hypercalcemia [8]. An ectopic parathyroid gland was found very deeply near the tracheal bifurcation [8]. Park et al. reported a 51-year-old woman who had HPT with ectopic parathyroid adenoma in the mediastinal para-aortic region [12]. In this case, the ectopic parathyroid adenoma of the MEN1 patient was found in the retroesophageal region. Parathyroid glands originate from the third and fourth branchial pouches and usually are located posterior to the thyroid. But the abnormal embryological migration of parathyroid glands are also found in 1–3% of the overall population [13]. MEN1 syndrome or HPT could give a proliferative stimulus to the ectopic parathyroid gland, making the cells in the ectopic gland proliferate and enlarge [8]. When the stimulus is strong enough, the cells will proliferate in a tumorous manner. Thus, we could observe an ectopic parathyroid adenoma in this patient, which made the patient present persistent HPT.
Surgery is the main treatment choice for parathyroid adenoma in patients diagnosed with MEN1 [4]. The recommended surgical approach is subtotal parathyroidectomy with removal of 3.5 parathyroid glands. Total parathyroidectomy is also an option for patients who have extensive disease either at initial or repeat surgery [14]. In the present case, the patient received parathyroid surgery to remove the diseased parathyroid gland before he was diagnosed with MEN1. However, after the diagnosis was made, we did not choose subtotal parathyroidectomy or total parathyroidectomy either, since we thought that the ectopic parathyroid adenoma was the dominant gland to affect HPT. It has been reported that some MEN1 patients with HPT who present only one enlarged gland could benefit from excision of the enlarged parathyroid [8, 15, 16]. In our case, after surgery of the ectopic parathyroid adenoma excision, the patient’s PTH and serum calcium levels were restored to normal. But long-term efficacy should be observed.
In conclusion, we reported a MEN1 patient who presented with persistent HPT with an ectopic parathyroid adenoma near the rear side of the esophagus. Thus, when we meet MEN1 patients with persistent HPT, we should note the possibility that an ectopic parathyroid adenoma may exist.