Gallstones represent one of the most prevalent digestive disorders worldwide, affecting approximately 10–20% of adults, with the incidence steadily increasing in recent decades due to changes in diet and lifestyle patterns [1]. The pathogenesis of gallstones primarily involves disturbances in bile composition – such as cholesterol supersaturation, reduced bile salt levels, and excessive mucin secretion – which promote bile crystallization and stone formation [2].
Obesity, particularly abdominal obesity, is a well-established risk factor for gallstone formation [3]. Prior studies have shown that weight gain contributes to gallstone development through multiple mechanisms, including altered cholesterol metabolism, impaired gallbladder motility [4], and enhanced intestinal cholesterol absorption mediated by Niemann-Pick C1-Like 1 protein. Moreover, obesity-induced chronic inflammation and oxidative stress elevate levels of proinflammatory cytokines such as TNF-α and IL-6 and increase reactive oxygen species, thereby aggravating metabolic disturbances and promoting gallstone formation [5].
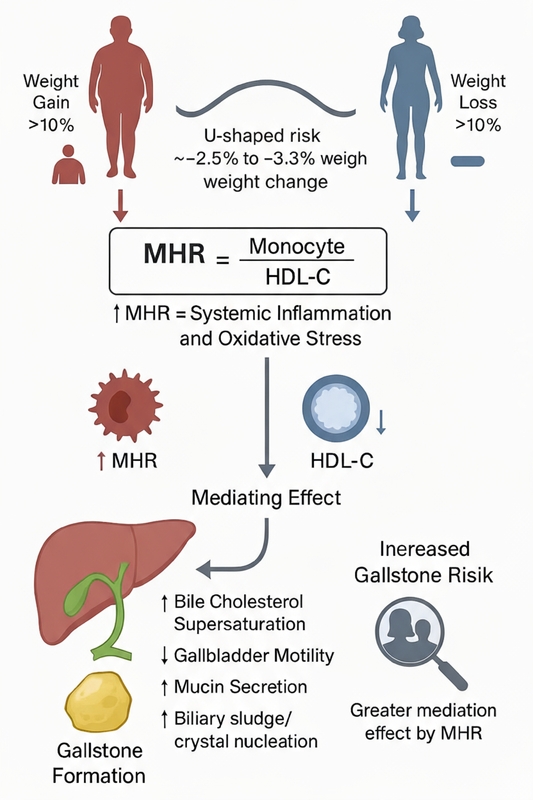
Inflammation plays a central role in gallstone pathophysiology. Oxidative stress and inflammatory cytokines impair gallbladder epithelial function and disturb bile metabolism, accelerating stone formation [6]. Given that weight gain is closely associated with systemic inflammation, the chronic inflammatory milieu may be a key mechanism linking weight change to gallstone risk. The monocyte-to-high-density lipoprotein cholesterol ratio (MHR), a novel biomarker reflecting the balance between proinflammatory monocytes and anti-inflammatory HDL cholesterol, has recently emerged as an indicator of systemic inflammation and metabolic dysregulation [7]. Elevated MHR levels have been linked to metabolic syndrome and cardiovascular disease, suggesting that MHR may also mediate the relationship between weight gain and gallstone risk through inflammation and oxidative stress pathways.
Although obesity has long been recognized as a major determinant of gallstone disease, evidence regarding how weight change influences gallstone risk remains limited. Therefore, this study aimed to investigate the association between weight gain and gallstone risk, with particular attention to the potential mediating role of MHR. Using data from the National Health and Nutrition Examination Survey (NHANES), this study provides new insights into the inflammatory mechanisms underlying gallstone development and supports more individualized strategies for early prediction and prevention.
Methods
Study population
This study used data from the 2017–2020 cycles of the National Health and Nutrition Examination Survey (NHANES), a publicly available, nationally representative dataset collected via multistage probability sampling. Participants aged < 20 years or with missing data on key variables were excluded, resulting in a final analytic sample of 7,398 individuals. Details on inclusion criteria and exclusions are illustrated in Supplementary Figure S1 and further elaborated in the Supplementary Materials.
Gallstone prevalence
Gallstone prevalence was assessed using self-reported physician diagnosis via the NHANES questionnaire item MCQ550.
Weight gain percentage
Weight gain percentage was calculated as: [(current weight – weight 1 year ago)/weight 1 year ago] × 100. Participants were grouped as follows: –10 to –5.1%, –5 to 5% (reference), 5.1 to 10%, and > 10%.
Monocyte-to-HDL-C ratio (MHR)
MHR was defined as the ratio of monocyte count to HDL cholesterol level. Laboratory methods for both measurements are described in the Supplementary Materials.
Covariates
Potential confounders were selected based on prior literature and > 10% effect size change, including sociodemographics, lifestyle behaviors, comorbidities, and medication use. Definitions of all covariates are provided in Supplementary Materials.
Statistical analysis
All statistical analyses were performed using R (v4.2.1) and Free Statistics (v2.0). Continuous variables are expressed as means ± SD or medians (IQR), and categorical variables as frequencies (%). Comparisons used appropriate parametric or nonparametric tests. MHR was log2-transformed and categorized into quartiles. Multivariable logistic and linear regression models examined associations between weight gain, gallstone risk, and MHR, with adjustments for confounders. Nonlinear trends were explored using segmented regression. Mediation analysis with bootstrapping was used to evaluate the indirect role of MHR. Sensitivity analyses included E-value computation, subgroup analysis, multiple imputation, and expanded covariate models. All tests were two-sided, with p < 0.05 considered statistically significant.
Results
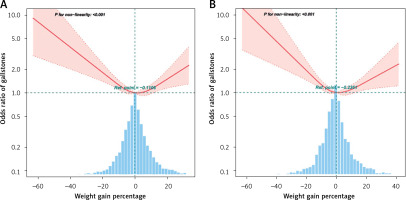
Restricted cubic spline analysis revealed a U-shaped relationship between percentage weight change and gallstone risk (nonlinearity p < 0.001; Figure 1). The lowest risk occurred near the inflection point (pre-PSM: –2.45%; post-PSM: –3.31%). Below this threshold, gallstone risk decreased with increasing weight gain (pre-PSM: OR = 0.954, 95% CI = 0.921–0.987, p = 0.0075; post-PSM: OR = 0.971, 95% CI = 0.957–0.986, p < 0.001), whereas above it, risk rose significantly (pre-PSM: OR = 1.029, 95% CI = 1.011–1.047, p = 0.0012; post-PSM: OR = 1.055, 95% CI = 1.02–1.091, p = 0.0019) (Supplementary Tables SI, SII). Fully adjusted analyses confirmed that both excessive weight loss (< –10%) and marked gain (> 5%) were independently associated with greater gallstone risk compared with stable weight (–5% to 5%), and this pattern persisted after PSM (Supplementary Table SIII).
Figure 1
Restricted cubic spline plot of the association between weight gain percentage and gallstone risk. Solid and dashed lines represent the predicted value and 95% confidence intervals. The models were adjusted for age, sex, race, educational level, marital status, family poverty-income ratio, smoking and drinking status, sleep duration, weight loss attempts in the past year, diabetes, hypertension, coronary heart disease, cancer, and asthma. A – Before propensity score matching, B – After propensity score matching
After adjustment for confounders, each one-unit increase in log2-transformed MHR was linked to higher gallstone risk (pre-PSM: OR = 1.29, 95% CI = 1.14–1.46, p < 0.001; post-PSM: OR = 1.25, 95% CI = 1.11–1.40, p < 0.001) (Supplementary Table SIV, Model 2). When divided into quartiles, participants in Q2–Q4 showed significantly greater risks than those in Q1, and the results remained robust after PSM. Multivariable linear regression further indicated that every 5% increase in weight gain corresponded to a significant rise in MHR (pre-PSM: β = 2.62, 95% CI = 1.9–3.33, p < 0.001; post-PSM: β = 1.93, 95% CI = 0.92–2.95, p < 0.001). Likewise, compared with participants maintaining weight (–5% to 5%), those gaining 5–10% had a significantly higher gallstone risk, consistent across PSM analyses (Supplementary Table SV).
Mediation analysis showed that MHR partially mediated the relationship between weight gain percentage and gallstone risk (Supplementary Figure S2). Before PSM, the indirect effect was β1 × β2 = 0.0001 (95% CI = 0.0001–0.0002, p = 0.0002), accounting for –50% of the total effect. After PSM, the indirect effect was 0.0002 (95% CI = 0.0001–0.0004, p = 0.0137), with a mediation proportion of –15.3%. Collectively, these findings indicate that systemic inflammation, reflected by MHR, plays a significant mediating role in the association between weight change and gallstone formation.
Discussion
To our knowledge, this study is the first to examine the association between weight change and gallstone risk using nationally representative NHANES data, with a particular focus on the mediating role of the monocyte-to-high-density lipoprotein cholesterol ratio (MHR). We identified a significant U-shaped relationship between weight change and gallstone risk, with the lowest risk occurring around a 2–3% weight loss. Both excessive weight gain and loss were independently associated with higher gallstone risk, and this pattern remained robust after multiple sensitivity analyses. Moreover, MHR was positively correlated with gallstone risk, and mediation analysis confirmed its significant indirect effect, particularly among younger and female participants. These findings underscore the complex interplay among weight fluctuations, inflammation, and gallstone formation.
Our results align with prior research showing that both weight gain and loss can elevate gallstone risk. A study of Korean adults reported that weight changes exceeding 5% increased gallstone incidence by 2–32%, while a large cohort study of 112,109 middle-aged participants found that weight changes over 5 kg were associated with greater gallstone risk in both sexes [8, 9]. The increased risk associated with rapid weight loss may arise from metabolic changes that elevate bile cholesterol saturation and reduce gallbladder motility, thereby promoting biliary sludge formation [10]. Conversely, short-term weight gain may increase gallstone risk by enhancing bile cholesterol supersaturation, reducing gallbladder motility, and triggering insulin resistance and chronic inflammation [11].
The MHR, a biomarker integrating proinflammatory monocytes and anti-inflammatory HDL cholesterol, was significantly associated with gallstones in this study, consistent with previous evidence linking inflammation and oxidative stress to gallstone pathogenesis. Mechanistically, weight gain elevates monocyte counts and reduces HDL levels, amplifying systemic inflammation and impairing reverse cholesterol transport, which may accelerate cholesterol deposition in bile [12]. Similarly, rapid weight loss can activate inflammatory pathways, with elevated MHR levels capturing these systemic alterations [13]. The mediation analysis confirmed that MHR plays an important intermediary role between weight change and gallstone risk, indicating that systemic inflammation represents a key biological bridge between metabolic fluctuation and biliary pathology.
This mediating effect was more pronounced among younger and female individuals. Hormonal factors, particularly estrogen, may contribute by modulating lipid metabolism and promoting bile supersaturation and gallbladder dysfunction [11]. Younger individuals may also exhibit stronger inflammatory responses due to higher metabolic activity, increasing susceptibility to gallstone formation [14]. Emerging molecular and epidemiologic evidence suggests that young adults may show greater metabolic liability and a more reactive inflammatory/metabolic phenotype in response to acute perturbations such as rapid weight gain, compared with older adults who show features of immunosenescence and chronic low-grade inflammation (inflammaging) [15]. Taken together, these subgroup findings suggest that inflammation and hormonal-metabolic factors jointly shape gallstone risk in susceptible populations.
This study has several strengths. The NHANES dataset provides high-quality, nationally representative data, enabling generalizable conclusions. Rigorous statistical methods, including PSM, enhanced result robustness. Most notably, this is the first study to identify MHR as a mediator linking weight change to gallstone risk, revealing an inflammatory mechanism underlying weight fluctuation and gallstone formation. Nonetheless, several limitations should be noted. The cross-sectional design precludes causal inference; thus, associations among weight change, age, sex, and gallstone prevalence should be interpreted as noncausal. Our findings specifically concern gallstone prevalence and related inflammatory–metabolic factors and should not be extrapolated to cholecystitis or other complications, as NHANES lacks validated outcome data for these conditions. Furthermore, unmeasured confounding cannot be fully excluded despite statistical adjustments. Future longitudinal studies incorporating dynamic biomarker measurements are warranted to validate these causal pathways.
In conclusion, this study highlights that both excessive weight gain and loss increase gallstone risk and that systemic inflammation, reflected by elevated MHR, mediates this association. These findings provide novel insight into the inflammatory and metabolic mechanisms of gallstone formation and may inform early prediction and personalized prevention strategies.