Introduction
Malfunctions of the heart occur in the following manifestations: rhythm disturbances and conduction disturbances of the heart muscle [1, 2]. Every year in the United States, atrial fibrillation is detected in 2.3 million people, and about 90 thousand cases of ventricular tachycardia are also reported here annually [3]. Disturbances in the heart rhythm are detected in 25% of patients who are being examined for the first time and had no complaints of heart pain or palpitations. The development of ventricular arrhythmias in the United States alone causes sudden death annually in 180–450 thousand people [4, 5]. Among these patients, there is a high incidence of depressive and anxiety disorders, which, according to some reports, are observed in 40–60% of the entire sample [6].
Some studies report a pronounced negative effect of depression on the health of patients with diagnoses such as chronic cardiovascular failure and coronary heart disease [7].
It has been found that cardiovascular diseases more often develop with depression, identified during initial assessment. In addition, with the development of coronary heart disease (CHD), patients with depression are at a higher risk of developing cardiovascular disease and mortality. An increase in risk is characteristic of patients not only with major depression, but also with a moderate degree of depression. However, the risk of recurring myocardial infarction and cardiac death increases as depression intensifies [8]. Depression can precede vascular pathology for decades. However, it is not yet known to what extent such an early-onset depression determines the development of vascular pathology and to what extent such an association is a consequence of general predisposing factors. Depression can be a consequence of vascular changes in the brain.
Moreover, depressive and anxiety disorders can be predictors of cardiovascular events, in particular heart attacks and strokes leading to repeated hospitalizations [9]. It has been established that the risk of adverse cardiovascular events under the influence of anxiety-depressive disorders is not associated with the functional class of chronic heart failure. Depression in such patients can lead to inhibition of cognitive function [10]. In patients with a combined depressive disorder and diseases of the cardiovascular system, cerebrovascular pathological processes might develop, accompanied by numerous metabolic disorders in the brain tissue, a decrease in cognitive functions, as well as an imbalance in the autonomic nervous system [11].
According to the data obtained, in patients with coronary heart disease, the presence of anxiety-depressive disorders leads to a 1.5–2.0 times increase in the probability of cardiovascular catastrophes leading to death [12]. The data on chronic heart failure are also disappointing – in patients with depression, the frequency of hospitalization increases 2.0 times, the cost of treatment increases by a third, and there is a general decrease in the quality of life [13]. According to the MONICA study, in patients after acute myocardial infarction, depressive disorder within 0.5–3.0 years becomes the main prognostic factor for recurrent heart attack and death [14].
The frequent occurrence of depression in cardiological patients is associated with the general links of the pathogenesis of damage to the cardiovascular and central nervous system. From the standpoint of physiology, the effect of depression on the complications of cardiovascular diseases can be explained by two hypotheses:
the vascular hypothesis (generalized damage in the vascular system of the brain can further affect mood regulation processes);
other risk factors, in particular, arterial hypertension, dyslipidemia, diabetes mellitus – common for stroke and myocardial infarction – may be related to depression.
In addition, damage to the small vessels of the brain, hyperintensity of white matter according to magnetic resonance imaging, and “hidden” cerebral infarction can also affect the occurrence of depression. In addition, less specific mechanisms may be involved in the formation of depression: both myocardial infarction and ischemic stroke are strong stressors, leading to significant consequences in the physical and mental state of patients [15, 16]. In depression, a decrease in serotonergic neuromediation can be associated with an increase in the level of inflammatory markers and the corresponding effects on cardiovascular outcomes. In addition, elevated levels of inflammatory markers (e.g., interferon-γ) are associated with the activity of an enzyme that converts tryptophan (a serotonin precursor) to kynurenine in patients with cardiovascular diseases [17]. This leads to a decrease in serotonin levels and may be another link in the relationship between inflammation and depression in cardiac patients. The main risk factors for depression in patients with chronic heart failure, combined with atrial fibrillation, may be the following factors: female gender, low level of education, NYHA functional class 2 or more, aldosterone antagonists [18].
It is known that psychosocial factors make a significant contribution to the development of cardiovascular diseases [10]. It is this group of factors that causes the development of arrhythmia in individuals who do not have organic changes in the heart tissue. Psychosocial factors include the processes of globalization and urbanization, an increasing number of stressful events, an increase in average life expectancy, and an increase in migration processes among the world’s population [19]. In developed countries (EU, USA, Japan, Canada, etc.), favorable aspects of living in megacities (the result of a set of active measures to combat risk factors) prevail over negative ones (unfavorable environmental situation), which contributes to lower mortality from cardiovascular diseases [20]. In developing countries (Brazil, Russia, Mexico, countries of Africa), however, urbanization is associated with a greater risk of adverse outcomes of cardiovascular diseases [21, 22]. For developing countries, the example of Russia shows a greater likelihood of depression and anxiety disorder of city residents, compared with rural residents [23].
Pathological diseases of the cardiovascular system and anxiety-depressive disorders should not be considered as independently proceeding processes; numerous data indicate an inextricable link between them. In turn, the relationship determines the influence of these processes on each other, in most cases positive – the more one process develops, the more the other manifests itself. Depression and cardiac diseases have a bi-directional relationship in which inflammatory processes, endothelial dysfunction, increased platelet activity, neurohumoral and autonomic nervous system dysfunctions related to depression, and depressive behavior mutually potentiate each other [24]. All this leads to an ever-increasing risk of complications and even an increase in the number of deaths [25].
Among cardiac arrhythmias, the so-called extrasystolic arrhythmia prevails in the frequency of cases [26]. Extrasystolic arrhythmias are divided into two main classes. Functional arrhythmias do not significantly affect a person’s quality of life, and are not detected by general blood tests. As a rule, functional arrhythmias are of psychosomatic origin. Another type of extrasystolic arrhythmias, organic, is associated with processes of inflammation in the heart tissue, excessive myocardial development (in individuals with increased physical activity), as well as diseases such as ischemia and heart defects [27].
In some patients prone to neurotic reactions, extrasystole can be very painful. Excessive sensitivity to changes in heart rhythm causes a chain reaction – the appearance of anxiety-depressive disorders [28]. In turn, these disorders cause the appearance of more dangerous diseases of the cardiovascular system – ischemia, heart failure and others. Yet, for patients undergoing inpatient treatment, the frequency of anxiety-depressive disorders is lower than in patients with heart attacks and other heart pathologies and ranges from 5 to 14% according to various sources [29]. Nevertheless, extrasystole and other forms of arrhythmia are the first step before the development of more serious consequences of diseases of the cardiovascular system.
Among the methods used to correct anxiety and depressive disorders, drug therapy predominates [30]. Among other methods, psychotherapy and therapy with music are used. An important point is support from friends and relatives. In particular, anxiolytics (tranquilizers) are used, i.e., drugs that are used systematically and can cause addiction. Addiction is observed both at the physical (habituation of the organism) and mental levels, with the development of the so-called withdrawal syndrome [31]. In this regard, the use of tranquilizers occurs only under the supervision of a psychiatrist. The above reasons reduce the massive use of this group of drugs.
There is an urgent need for research on the timely diagnosis of anxiety and depressive disorders in patients with cardiac arrhythmias and diseases of the cardiovascular system. In case of early detection of depression symptoms and adequate therapy, it is possible to reduce the risk of adverse cardiovascular events and catastrophes by 1.5–2.0 times. This study focuses on monitoring depressive disorder in patients with extrasystolic arrhythmia. Accordingly, the purpose of this study is to perform a comparative analysis of the degree of development of anxiety-depressive disorder in patients with different types of extrasystolic arrhythmia by means of different assessment scales.
Material and methods
Research design and sample
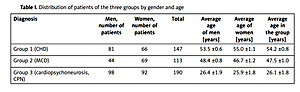
The study was conducted in 2018–2019 based on the cardiology department of polyclinic No. 4 of Moscow (Russian Federation). The study involved 450 patients with extrasystolic arrhythmia. The gender and age distribution of patients are presented in Table I. Patients were divided into three groups depending on the diagnosis of the cause of the observed arrhythmia. The first group included patients with CHD, the second – myocardiodystrophy (MCD), and the third – cardiopsychoneurosis (CPN). CHD develops with a disruption of the myocardial blood supply, with a progressive lesion of the coronary arteries. CHD occurs in about 90% of patients with diseases of the cardiovascular system. MCD is characterized by metabolic disorders in the heart muscle under the influence of factors not related to the heart. MCD is often detected in children and adolescents and can cause the development of diseases such as heart failure. It occurs in 20–25% of patients with cardiovascular disease. CPN is characterized by disorders of neuroendocrine regulation with multiple and varied clinical symptoms that occur or are aggravated by stressful effects. This disease represents 32–50% of general cardiovascular diseases, which are based on autonomic disorders. Thus, all three diseases are quite common. Thus, patients with these diagnoses have been included in this study. Out of these three diseases, CHD is the most severe.
Table I
Distribution of patients of the three groups by gender and age
As can be seen from the data in Table I, there are no significant differences between the numbers of men and women within each group (except for group 2, where there are 1.5 times more women, at p ≤ 0.05). The average age of patients in groups 1 and 2 does not differ, but patients from group 3 (both men and women) are 1.5 times younger.
Patients from group 3 are younger, since long-term psycho-emotional stress caused by significant acute and chronic stressful situations in young people (employment, as well as bad habits – smoking and alcohol) has a greater influence in this group compared to the other two. Such stress is the main reason for the development of CPN in young people.
Conditions for inclusion in the study protocol
The presence of extrasystolic arrhythmia in the diagnosis, the absence of pathological changes, with their prevalence over arrhythmia and the need for intensive emergency therapy, the absence of mental illness in patients and their relatives. An agreement was concluded with each of the patients on non-disclosure of information and anonymity of the study, as well as on voluntary consent to participate in the study. This study was conducted in accordance with international standards of confidentiality, ethics and morality [32].
Intervention
All patients from the three groups underwent 12-lead electrocardiographic examination. In parallel, an echocardiographic study was performed on an Aloka H 40A apparatus. Qualitative and quantitative characteristics of the electrocardiogram were obtained by daily monitoring according to the Holter method using the Holter-DMS apparatus, KSNR 2 ECG DMS model, Cardiotechnics, Russian Federation. In this case, two unipolar leads were used, with the modification V2, V5.
The following parameters were evaluated: a) heart rate per day (heart rate); b) the number of extrasystoles of ventricular and supraventricular origin during the day; c) parameters of ectopic activity of the ventricles, according to the generally accepted classification of Laun-Wolf.
When identifying the type of extrasystole, a bicycle ergometer test was performed for each patient.
To assess the mental indicators of patients, in particular quality of life, a questionnaire was used, developed at the Orenburg Medical Academy [33]. The severity of the development of anxiety-depressive disorder was assessed using the Montgomery and Asberg scale, as well as the Zung scale. Covi and Zung scales were used to assess anxiety disorder. The Montgomery-Asberg scale is characterized by its brevity and ease of use, reliability of assessing a depressed state and sufficient sensitivity, and accuracy with respect to assessing the dynamics of a state. It was designed for quick and accurate assessment of the severity of depression and changes in the severity of the condition as a result of therapy. The Covi scale was designed to determine the intensity of anxiety, which is determined by 3 parameters: patient complaints, his/her behavior and somatic manifestations. The Zung scale was designed to assess the severity of depression. Depression is detected based on the patient’s self-esteem.
Statistical analysis
The data were processed using the program Statistica 6.0 (StatSoft Inc., USA). Parametric methods of statistical analysis were used – a two-sample t-test for independent samples. Data differ significantly at p ≤ 0.05. For each of the parameters, the arithmetic mean was calculated and the error of the mean. Data are presented as the average number of points for each of the applied scales for assessing depression and anxiety.
Results
According to the obtained data, no significant differences by gender were found (Table II). Thus, this pattern can be traced for all three scales.
Table II
Average indicators of depression and anxiety on various scales depending on the gender factor (in points)
It was found that, regardless of gender, there were no significant differences for depression and anxiety disorders. From this it follows that for all patients of the examined sample, both men and women, anxiety and depressive disorders appear with the same frequency.
For three groups of patients, differing in type of cardiac arrhythmias, significant differences were obtained (Table III). Thus, for group 1, the depression indicators on the Zung scale significantly differ from the indicators of group 2. At the same time, between groups 2 and 3 on the same scale the differences are also significant. For the scales of depressive disorders according to Montgomery-Asberg, no such differences were found, as well as for anxiety on the Zung scale. Other significant differences were obtained on the Covi scale, for indicators of anxiety disorders, between all three groups (except for groups 1 and 3). It follows that depressive and anxiety disorders are mostly manifested in all cases in patients from the second group (MCD), then in patients with CHD and minimally in patients with CPN. The latter may also be associated with a younger age of patients, in whom depression is usually not as severe as in older age.
Table III
Average indicators of depression and anxiety in patients with extrasystolic arrhythmia on various scales depending on the disease
| Disease and patient group | Zung depression scale [points] | Montgomery-Asberg depression scale [points] | Zung anxiety scale [points] | Covi anxiety scale [points] |
|---|---|---|---|---|
| CHD (group 1) | 40.9 ±0.7* | 15.1 ±0.7 | 38.1 ±0.9 | 3.2 ±0.1* |
| MCD (group 2) | 43.0 ±0.9** | 14.3 ±0.8 | 40.6 ±0.8 | 3.6 ±0.2** |
| CPN (group 3) | 37.1 ±0.8 | 13.1 ±1.1 | 36.6 ±1.1 | 2.8 ±0.1 |
However, in the analysis of forms of extrasystole, other patterns are revealed. It was found that with supraventricular extrasystole, the maximum number of depression points on the Zung scale is also in patients from group 2 (MCD), slightly lower in patients from group 1 (CHD), and the minimum in patients from group 3 (p ≤ 0.05) (Table IV). On the other hand, indicators of anxiety according to the Zung scale, according to the Covi scale, and depression indicators according to the Montgomery-Asberg scale significantly differ in patients from groups 2 and 3 (p ≤ 0.05). At the same time, patients from group 2 scored the maximum number of points in terms of anxiety on the Zung and Covi scales.
Table IV
Average rates of depression and anxiety in patients with supraventricular extrasystole, depending on the disease
The same patterns are also manifested in the analysis of scores on various scales of depression and anxiety among patients with ventricular extrasystole (Table V). The maximum number of points was recorded for patients from group 2, the minimum for patients from group 3 (p ≤ 0.05). Significant differences were recorded only for indicators of depression on the Zung scale, while on the other scales they were absent.
Table V
Average rates of depression and anxiety in patients with ventricular extrasystole, depending on the disease
It follows that the differences in depression and anxiety rates are most pronounced in patients diagnosed with supraventricular extrasystole (on all scales for depression and anxiety), to a lesser extent for patients diagnosed with ventricular extrasystole (only for depressive disorders, on the Zung scale). This may be due to the fact that with supraventricular extrasystole, the patient feels symptoms that can form a high level of anxiety and depression – a heartbeat on the chest, heart failure, a sinking heart, lack of air, decreased performance and fatigue. The second type of extrasystole can occur with a less pronounced clinical picture, and, accordingly, cause a lower level of anxiety or depression. There were no significant differences between the patients with supraventricular and ventricular extrasystoles in the level of manifestation of depression and anxiety. Thus, depressive and anxiety disorders are equally dangerous for both men and women with extrasystole.
Among the three scales used to determine the level of depression and anxiety, the Zung scale turned out to be the most sensitive, since its use revealed significant differences in both the level of depression and the level of anxiety in patients with various diseases. Therefore, this scale can be recommended as the most sensitive scale in detecting levels of depression and anxiety in patients with diseases of the cardiovascular system.
Discussion
The emergence and development of cardiovascular diseases can be promoted by a number of factors – diabetes, bad habits, congenital malformations, inflammatory processes and obesity [34]. The functional form of extrasystolic arrhythmia is known to include various disorders, such as tachycardia (sinus, paroxysmal and supraventricular), and attacks of various origins, in particular, atrial flutter [35]. When a patient experiences such attacks, an increase in general stress and an increase in excitement, as well as anxiety, are noted [36]. In the case of extrasystoles, patients experience the most intense heart tremors, subsequent to a compensatory pause. These tremors are also referred to as heart “tripping”. Usually, the reasons for such attacks are domestic quarrels, conflicts, etc. [37, 38]. According to some reports, a quarter of patients have a consistent relationship between the onset of an attack and the onset of a situation associated with conflict or other forms of stress [39]. A conscious behavioral reaction develops among some patients – suppressing their feelings in order not to show them in relation to others, and avoiding a stressful situation to reduce the likelihood of an attack [40]. Most often, the ventricular form of extrasystoles is observed during sleep, but there may be an increase in extrasystoles with emotional stress, which, ultimately, leads to hypochondria, as well as to an increase in suspiciousness [41]. Fear of sudden death is most evident in various heart rhythm disturbances, which ultimately increases the state of depression and anxiety [42]. The present study shows that patients with heart tissue disorders, for example, with MCD, are most susceptible to anxiety-depressive states. At the same time, according to patients, any disturbance of the rhythm of the heart caused them an anxiety state. At the same time, the fear of death from a myocardial rupture dominates among the sensations. The aggravation occurs when the fear of death does not stop tachycardia, but only enhances its manifestations and increases the duration of the attack. It is interesting to note that according to some observations, fear has a connection with the presence of a physician in the hospital and intensifies on weekends and holidays [17].
Almost half of the patients (up to 45%, according to some sources) did not show any changes in the ECG, or in the pulse. Violations of the rhythm of the heart are associated, as already established, with changes in the hypothalamus. Ventricular and atrioventricular extrasystoles, as a rule, arise at the onset of depression and stop when this condition is over [19]. According to the data obtained in the present study, patients from groups 1 and 2, with a diagnosis of CHD and MCD, had the highest rates on three scales for anxiety-depressive conditions. These data are consistent with others, according to which the prevalence of depression in patients with diabetes and CHD is estimated to be 12–18% and 15–23%, respectively [43, 44]. Depression after myocardial infarction occurs in 25% of patients [45].
Moreover, as the present study showed, in contrast, patients with the supraventricular form of extrasystole had more pronounced mental disorders and a depressed state. It is interesting to note that with an increase in depression, heart rhythm disturbances (revealed during ECG analysis) disappear with an increase in depressive disorder.
Depressive syndrome, according to some reports, may cause the patient to refuse treatment of cardiovascular diseases, such as paroxysmal atrial fibrillation [46].
Anxiety is a state of adaptation of the human body to abruptly changing conditions, which include disturbances in the rhythm of the heart. The presence of anxiety as a constant psychogenic factor can aggravate heart rhythm disturbances, while not taking into account anxiety as a personality trait. In such a case, anxiety of endogenous genesis is considered, developing as a response to internal factors [47]. The data in the present study show that anxiety can be no less important than a depressive state, and is equally widespread among patients in all three groups. The greatest anxiety was noted among patients with CHD and MCD.
It is the underestimation of factors of psychogenic origin that causes the development of cardiac rhythm disturbances, and concomitant inadequate drug therapy. The present study shows that, at least for supraventricular extrasystoles, such factors determine the general condition of the patient.
In conclusion, it was found that the maximum rates of anxiety-depressive disorder are typical for patients over the age of 45 years, without gender dependence. From this it follows that for all patients in the surveyed sample, both men and women, anxiety and depressive disorders occur equally often. Most often, depression and anxiety occurred in patients from the second group (MCD), less often in patients with CHD, and minimally in patients with CPN. Patients of group 3 belong to a younger age, when depression is not as pronounced as in older age. The most susceptible to depression and anxiety are patients with extrasystolic arrhythmia with a diagnosis of CHD, as well as MCD. At the same time, indicators of depression and anxiety on all three scales significantly differed in patients with ventricular extrasystole (over 40 points on the Zung scale, over 14 points on the Montgomery-Asberg scale for depression; more than 38 points on the Zung scale and more than 3 points on the Covi scale for anxiety). The Zung scale turned out to be the most sensitive to identifying significant differences in the level of depression; thus, it can be recommended in the diagnosis of depression and anxiety in patients with cardiovascular diseases. The same cannot be said about patients with supraventricular extrasystole, for whom a significant difference was obtained between groups 1 and 2 only in terms of depression on the Zung scale. Thus, depressive syndrome is most pronounced in patients with a ventricular form of extrasystole and with CHD. These patients may be recognized as the highest risk group. Accordingly, in patients with CHD and ventricular extrasystole, depressive disorders can be a cause of aggravation of health (cardiovascular catastrophes). Differences in the level of depression and anxiety occur in patients with a diagnosis of supraventricular extrasystole (on all scales for depression and anxiety), and to a lesser extent for patients with ventricular extrasystole (depressive disorders, Zung scale). It follows from this that depressive and anxiety disorders are equally dangerous for both men and women with supraventricular extrasystole. At the same time, an assessment of the negative impact of government restrictive measures due to the spread of COVID-19 and subsequent economic consequences in 2020 for patients may be the focus of future studies of anxiety-depressive disorder.