Introduction
The human coronavirus disease 2019 (COVID-19) led to a global lockdown and increased public anxiety and fears [1, 2]. As estimated, at least 4 billion people were forced to quarantine themselves. Observational studies indicate that such isolation has caused psychological distress, anxiety, insomnia, and depressive symptoms [3, 4]. Moreover, numerous investigations have reported adverse changes to the diet in a relatively high number of isolated individuals [5, 6]. According to some studies, the quarantine reinforced pre-existing alterations in body weight and adversely affected physical activity [5, 7]. The obligatory use of face masks also induces higher perioral humidity, temperature and breathing difficulties, which could be another limiting factor for athletes [8]. The potential infection among athletes could also influence the team training habits and the change in disinfection and protection protocols. Especially indoor athletes should be aware of air contamination with viral particles and use air disinfection similarly to the dental clinics [9]. An increase in alcohol consumption, particularly in individuals experiencing higher stress, was reported [5, 10,11]. These findings highlight that the COVID-19 pandemic has directly affected lifestyle behaviors, raising concerns from both an individual and public health perspective.
However, the above-mentioned effects of the pandemic may not necessarily apply to those practicing sports on a regular basis. To help them cope with the epidemiological situation, some strategies encompassing personalized conditioning training have been developed [12]. At the same time, data on how the pandemic has affected the physical activities of groups practicing particular sports are scarce [13]. Cycling athletes may be particularly affected as outdoor activities have been temporarily sanctioned due to lockdowns.
In athletes under one session of heavy training, both innate and acquired immunity are decreased transiently during the recovery period after prolonged heavy exertion (≥ 90 min), typically by 15–70% [14, 15]. Empirical evidence, albeit in a small number of athletes, indicates that international athletes suffer fewer, not greater, upper respiratory infection episodes compared to national-level athletes [16, 17]. The manipulation of training volume and/or intensity includes: gradually increasing volume and intensity by 5–10% per week; increasing the frequency of shorter, spike training sessions rather than enduring fewer but longer sessions, recoveries after intensive sessions and easier weeks after 3-week blocks [18]. Psychological stress has a well-known and marked influence on immunity; thus, it plays a role in the decrease in immunity with prolonged heavy exercise and heavy training [14]. Athletes may experience psychological stress associated with competition (or lack of competition), injury, travel, and sleep disruption; in addition, they may also experience psychological stress in their personal life related to relationship difficulties, financial hardship and bereavement. Unfortunately, psychological stress has rarely been reported in such studies; therefore, it is difficult to assess the strength of such a relationship. Some supporting evidence is, however, emerging, as more recent research shows that the level of anxiety and perceived stress (life stress in the last month) reported before exercise can significantly modify the immune response to subsequent exercise [18]. Sports practice in elite athletes should protect against psychological disorders, as stated by the International Olympic Committee (IOC), and its antidepressant effect probably disappears after ceasing to exercise [19].
Infectious diseases are usually successfully managed among athletes, but COVID-19 brought new and unprecedented challenges to the sports community, including cyclists [14, 20]. How did the epidemiological COVID-19 situation and risk of severe infection affect the training pattern, volume, and intensity? Was it influenced by psychological factors, including an athlete’s becoming infected with SARS-CoV-2 or the infection of related individuals? We hypothesized that athletes could change their training patterns and the pandemic negatively influences their quality of life with the resolution of SARS-CoV-2 infection. So far, these aspects have not been subjected to any reported research.
This study aimed to provide the first answers to the above questions by assessing the training activities and patterns (frequency, volume, intensity), quality of life factors, and the epidemiological situation among professional and advanced amateur cycling athletes during the COVID-19 pandemic in Poland.
Material and methods
To explore the effect of the COVID-19 pandemic on the training activities of professional and advanced cyclists in Poland, an anonymous online survey was performed. We based our study on adult males and females from the Polish Cycling Association elite and amateur license list (n = 1241). Given the size of the target population, it was calculated using Cochran’s formula [21] that 134 eligible individuals should be surveyed to reach the margin level of 8% at the confidence interval of 95%. Such a research approach has been recommended to swiftly reach a specific group of individuals, ensuring their safety under pandemic conditions [22]. The study was performed between 16 and 30 November 2020 and approved by the Bioethics Committee of Poznan University of Medical Sciences (KB – 170/21). Strict legal regulations limited the cycling season of 2020 under the pandemic in Poland. The first case of COVID-19 in Poland was identified on 4 March 2020; from 24 March, a nationwide lockdown was imposed; on 20 April, the ban on the recreational use of forests and parks was lifted; on 4 May, hotels and shopping centers were permitted to reopen. No cycling activities were possible between 24 March and 20 April, since cycling was only possible with the face covered. Nevertheless, all the cycling events, including professional and amateur competitions, were canceled until 31 July.
The online questionnaire (Google Forms) employed in this study was advertised and linked among Facebook professional and amateur cycling groups. A total of 40 target groups were searched on Facebook social media and were listed in two advertising posts distributed by our scientific and sports cooperators.
The inclusion criteria included: active cyclists who perform structured or unstructured training programs monitored by heart rate monitors. When available, additional data were requested: VO2 max expressed as mL of oxygen uptake per kg of body weight per minute (minimum difference: 1.0) and Training Stress Score estimated by appropriate software (iE TrainingPeaks, Golden Cheetah and others, minimum difference: 1.0). Cyclists were recruited from advanced amateurs who do not compete, amateurs who attend races and professional cyclists. Because of different training measuring devices and software as well as different training conceptions and planning, the study focused on heart rate monitors and average derivative information.
The employed questionnaire aimed to assess:
Training load during the COVID-19 pandemic in comparison to the pre-pandemic period (2019 season): weekly frequency and volume of sessions, weekly time spent in high-intensity intervals (expressed in minutes above 90% of HRmax, all times minimum difference 1 min), time spent in intensive intervals (expressed in minutes between 80 and 90 of HRmax), Training Stress Score (a composite number that takes into account the duration and intensity of a workout [23]) and VO2max expressed as ml of oxygen uptake per kg of body weight per min (when available for 2020, n = 51).
SARS-CoV-2 infection history in the studied cycling athletes, death of relative due to COVID-19, and the potential effect of these circumstances on training parameters.
Quality of life using the WHOQOL-BREF questionnaire in the following domains: physical health, psychological, environmental, and social relationships in association with training patterns and epidemiological situations of cycling athletes.
The demographic data on each surveyed individual included gender, age, body mass index (BMI; calculated from reported weight and height), years of training (weight, height, years minimum difference 1 kg, 1 cm, 1 year), type of cycling (road, mountain bike, triathlon, etc.).
The respondents completed the WHOQOL-BREF 26-item questionnaire in the valid Polish version [24–26], an abbreviated version of WHOQOL-100 developed by the quality of life researchers at the World Health Organization. It enables an assessment of the quality of life profile in the physical health, psychological, social relationships and environment domains. The domain scores were transformed into a linear scale between 0 and 100 following the scoring guidelines [27]. A higher score indicated a better QOL. The psychometric properties of the original version are considered as very good (Cronbach’s α = 0.89).
Data from Google Forms were exported to a spreadsheet file. The training characteristics data were analyzed simultaneously for the 2019 and 2020 seasons. Changes in training frequency, volume, intensity and Training Stress Score (TSS) were calculated by subtracting the 2020 value from the 2019 value. The TSS was calculated according to the following formula: TSS = (t × NP × IF)/(FTP × 3600) × 100, where t is the duration of the exercise bout, NP is its normalized power, FTP is the individual’s functional threshold power, IF is the intensity factor (the ratio between the NP. and the individual’s FTP) [24].
Statistical analysis
The statistical analysis was performed with SigmaPlot 11.0.0.77 (Systat Soft, USA). All data are presented as means ± SD and median values or percentages. Since the variables expressed on the interval scale did not meet the assumption of a Gaussian distribution, non-parametric statistical tests were applied. The differences in studied parameters between subgroups were analyzed with the Mann-Whitey U test. Correlations were assessed with Spearman’s correlation coefficient (Rs). A value of p < 0.05 was considered statistically significant.
Results
The online questionnaires were filled in by 131 respondents. One form was missing basic training data and was withdrawn from further analysis. The demographic breakdown of the studied groups is given in Table I.
Table I
Demographic breakdown of the studied group of cycling athletes in Poland (n = 130)
Training patterns
During the 2020 cycling season, 16.9% (n = 22) of athletes were confirmed to be SARS-CoV-2 positive, whereas 63.8% (n = 83) stated that they knew someone who had died due to COVID-19. The characteristics of training patterns in 2019 and 2020 are presented in Table II. Compared to the pre-pandemic season, no changes in weight, BMI, frequency of training, and exercise volume were reported. The time spent on high-intensity interval training (HIIT, > 90% of HRmax) was reduced from 37.0 to 31.6 min/week. Furthermore, although not significant, a decrease was observed in other intensive training between 80% and 90% of HRmax. For 47 athletes, the Training Stress Score was available. The weekly mean of TSS did not differ between pre-pandemic and pandemic seasons, but the maximum weekly TSS was reduced in the latter (660.6 vs. 767.0, p < 0.05). This represents the reduction of higher intervals and maximum weekly TSS while retaining overall training load.
Table II
Comparison between the pre-pandemic year 2019 and pandemic 2020 season regarding training patterns in the studied group of cycling athletes in Poland (n = 130)
| Parameter | 2019 season (prior to COVID-19) | 2020 season (during COVID-19) | P-value | |
|---|---|---|---|---|
| VO2max [ml/kg/min]* | Mean | – | 58.9 ±10.6 | – |
| Years of training [years] | Mean | – | 7.4 ±8.6 | – |
| Weight [kg] | Mean | 74.4 ±13.0 | 74.5 ±13.2 | 0.37 |
| Median | 74 | 74 | ||
| BMI [kg/m2] | Mean | 23.2 ±3.7 | 23.2 ±3.8 | 0.32 |
| Median | 23.1 | 23.2 | ||
| Frequency of training [/week] | Mean | 4.4 ±1.6 | 4.3 ±1.9 | 0.73 |
| Median | 4 | 4 | ||
| Training volume [h/week] | Mean | 8.1 ±3. | 8.0 ±4.3 | 0.68 |
| Median | 8 | 8 | ||
| Time spent in > 90% of HRmax [min/week] | Mean | 37.0 ±38.3 | 31.6 ±41.7 | 0.04 |
| Median | 27.5 | 20.0 | ||
| Time spent in 80–90% of HRmax [min/week] | Mean | 93.3 ±96.9 | 84.6 ±91.7 | 0.20 |
| Median | 60.0 | 60.0 | ||
| TSS [average/week]* | Mean | 396.8 ±216.8 | 391.0 ±207.8 | 0.15 |
| Median | 400.0 | 400.0 | ||
| TSS [maximum/week]* | Mean | 767.0 ±439.6 | 660.6 ±319.2 | 0.001 |
| Median | 715.0 | 660.0 | ||
We analyzed the potential influence of a positive COVID-19 test on the training patterns and quality of life measured by WHOQOL-BREF. Subjectively, a few respondents reported a decrease in training capacity, which in eight individuals did not recover (Table I). All the SARS-CoV-2-infected athletes were asymptomatic or had mild symptoms of COVID-19. Their training patterns after the infection period did not change. A tendency to reduce training volume and intensive sessions was observed, but the data variation was likely influenced by the smaller sample size bias. Interestingly, cyclists infected with SARS-CoV-2 had better physical health, social relations domain, and environmental domain scoring, but not in the psychological domain (Table III). Athletes infected with SARS-CoV-2 seemed slightly less experienced (4.8 years vs. 7.9) and had a lower VO2max (54.6 vs. 60.1) than those who did not acquire the infection, but the difference was not significant. Infected cyclists reported the resolution of symptoms without severe complications.
Table III
Changes in training and health domains among SARS-CoV-2-positive and SARS-CoV-2-negative cycling athletes in Poland (n = 130)
| Parameter | Infected cyclists (n = 22) | Non-infected cyclists (n = 108) | P-value | |
|---|---|---|---|---|
| Training experience [years] | 4.8 ±4.0 | 7.9 ±9.2 | 0.320 | |
| BMI | 23.5 ±2.5 | 23.1 ±3.9 | 0.659 | |
| VO2max [ml/kg/min]* | 54.6 ±6.9 | 60.1 ±11.2 | 0.28 | |
| Age [years] | 35.0 ±9.7 | 34.3 ±12.1 | 0.675 | |
| Change in frequency of training [/week] | Mean | –0.18 ±1.39 | 0.03 ±1.73 | |
| Median | 0 | 0 | 0.789 | |
| Change in training volume [h/week] | Mean | –0.29 ±3.78 | 0.0 ±3.81 | |
| Median | 0 | 0 | 0.564 | |
| Change in time spent in > 90% of HRmax [min] | Mean | –13.9 ±32.5 | –3.5 ±39.8 | |
| Median | –1.5 | 0 | 0.406 | |
| Change in time spent in 80–90% of HRmax [min] | Mean | –18.0 ±76.2 | –6.5 ±68.5 | |
| Median | 0 | 0 | 0.604 | |
| Change in TSS [average/week]* | Mean | –34.2 ±178.9 | 5.1 ±202.1 | |
| Median | –36 | 0 | 0.120 | |
| Change in TSS [maximum/week]* | Mean | –24.8 ±390.4 | –102.6 ±406.9 | |
| Median | –125 | –10 | 0.540 | |
| WHOQOL-BREF somatic domain (transformed) | Mean | 56.1 ±12.4 | 50.6 ±10.7 | |
| Median | 56 | 53 | 0.024 | |
| WHOQOL-BREF psychological domain (transformed) | Mean | 66.0 ±13.0 | 66.3 ±12.1 | |
| Median | 69 | 69 | 0.836 | |
| WHOQOL-BREF social domain (transformed) | Mean | 74.1 ±15.1 | 63.6 ±21.2 | |
| Median | 75 | 69 | 0.032 | |
| WHOQOL-BREF environmental domain (transformed) | Mean | 72.5 ±11.2 | 65.9 ±12.8 | |
| Median | 75 | 69 | 0.018 | |
Influence on quality of life
We hypothesized that infection with SARS-CoV-2 or death among family and friends due to COVID-19 could affect the training patterns. As observed, the routine training plan and the training frequency, volume, and intensity did not change statistically significantly in cyclists who experienced the death of their relatives/friends due to COVID-19 (Table IV). At the same time, such individuals revealed lower psychological health domain scoring (statistically significant) and social relation domain scoring (nearly significant) measured by WHOQOL-BREF.
Table IV
Changes in training patterns in the studied group of Polish cyclists (n = 130) in relation to whether they experienced death of family members or friends due to COVID-19
| Parameter | Cyclists who knew somebody who died (n = 83) | Cyclists who did not know somebody who died (n = 47) | P-value | |
|---|---|---|---|---|
| Change in frequency of training [/week] | Mean | 0.08 ±1.8 | –0.14 ±1.30 | |
| Median | 0 | 0 | 0.57 | |
| Change in training volume [h/week] | Mean | 0.00 ±4.1 | –0.15 ±3.21 | |
| Median | 0 | 0 | 0.88 | |
| Change in time spent in > 90% of HRmax [min] | Mean | –3.0 ±39.9 | –9.4 ±37.2 | |
| Median | 0 | 0 | 0.97 | |
| Change in time spent in 80–90% of HRmax [min] | Mean | –7.9 ±77.3 | –9.5 ±55.4 | |
| Median | 0 | 0 | 0.90 | |
| Change in TSS [average/week]* | Mean | –6.2 ±200.1 | 6.1 ±192.1 | |
| Median | 0 | –20 | 0.67 | |
| Change in TSS [maximum/week]* | Mean | –112.1 ±425.4 | –9.2 ±318.0 | |
| Median | –32.5 | 0 | 0.22 | |
| WHOQOL-BREF somatic domain (transformed) | Mean | 52.1 ±11.1 | 50.0 ±11.3 | |
| Median | 56 | 50 | 0.28 | |
| WHOQOL-BREF psychological domain (transformed) | Mean | 64.5 ±12.6 | 69.2 ±11.0 | |
| Median | 69 | 69 | 0.02 | |
| WHOQOL-BREF social domain (transformed) | Mean | 63.6 ±20.7 | 68.6 ±20.6 | |
| Median | 69 | 75 | 0.11 | |
| WHOQOL-BREF environmental domain (transformed) | Mean | 67.2 ±12.8 | 66.5 ±12.8 | |
| Median | 69 | 69 | 0.62 | |
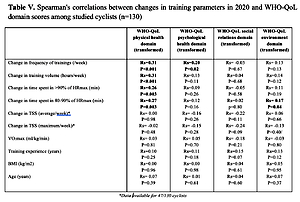
Physical health correlated positively with the change of training frequency, volume and intensity. At the same time, psychological health positively affected only the frequency of training but not its volume and intensity. Age, training experience, BMI and VO2max had no influence on the whole health report (Table V).
Table V
Spearman’s correlations between changes in training parameters in 2020 and WHOQOL domain scores among studied cyclists (n = 130)
| Parameter | WHOQOL physical health domain (transformed) | WHOQOL psychological health domain (transformed) | WHOQOL social relations domain (transformed) | WHOQOL environment domain (transformed) |
|---|---|---|---|---|
| Change in frequency of training [/week] | Rs = 0.31 | Rs = 0.20 | Rs = –0.03 | Rs = 0.13 |
| P < 0.001 | P = 0.02 | P = 0.67 | P = 0.13 | |
| Change in training volume [h/week] | Rs = 0.31 | Rs = 0.13 | Rs = 0.04 | Rs = 0.14 |
| P < 0.001 | P = 0.11 | P = 0.68 | P = 0.12 | |
| Change in time spent in > 90% of HRmax [min] | Rs = 0.26 | Rs = 0.09 | Rs = –0.05 | Rs = 0.11 |
| P = 0.003 | P = 0.26 | P = 0.58 | P = 0.19 | |
| Change in time spent in 80–90% of HRmax [min] | Rs = 0.27 | Rs = 0.12 | Rs = 0.02 | Rs = 0.17 |
| P = 0.003 | P = 0.16 | P = 0.80 | P = 0.04 | |
| Change in TSS [average/week]* | Rs = 0.00 | Rs = –0.16 | Rs = –0.22 | Rs = 0.06 |
| P = 0.98 | P = 0.26 | P = 0.11 | P = 0.66 | |
| Change in TSS [maximum/week]* | Rs = –0.02 | Rs = –0.15 | Rs = –0.24 | Rs = –0.13 |
| P = 0.48 | P = 0.28 | P = 0.09 | P = 0.40/ | |
| VO2max [ml/kg/min] | Rs = 0.03 | Rs = 0.05 | Rs = –0.18 | Rs = –0.03 |
| P = 0.81 | P = 0.70 | P = 0.21 | P = 0.80 | |
| Training experience [years] | Rs = 0.10 | Rs = 0.11 | Rs = 0.15 | Rs = 0.13 |
| P = 0.25 | P = 0.18 | P = 0.07 | P = 0.12 | |
| BMI [kg/m2] | Rs = 0.00 | Rs = 0.00 | Rs = 0.04 | Rs = 0.05 |
| P = 0.96 | P = 0.98 | P = 0.61 | P = 0.95 | |
| Age [years] | Rs = 0.07 | Rs = 0.01 | Rs = 0.04 | Rs = 0.07 |
| P = 0.39 | P = 0.61 | P = 0.60 | P = 0.37 |
Discussion
To the best of our knowledge, this is the first study to report on the effects of the COVID-19 pandemic on the training patterns of cycling athletes. The epidemiological situation has caused global disruptions to the world of sports with cancellations of major and smaller-scale sporting events, including cycling competitions. By itself, this could affect the training volume and intensity of amateur and professional cyclists.
In general, there are different strategies to achieve optimal results in cycling. Planning the whole year season is crucial for achieving the best results for priority racings (A) independent of cycling types: road, cross country, or triathlon. Several measurement parameters and devices have been developed in sport science for proper coaching or self-coaching. They are based on the conception of training frequency, volume (duration), and intensity, whereby intensity could be considered as full session intensity and one session intensity, measured at least by heart rate monitors or a power meter. However, diet, recovery, and micro/macrocycle planning are needed to achieve the highest possible efficiency. This includes low-intensity basic training mixed with an interval session, periodization or inverted periodization, polarization, high altitude training/living, and a racing calendar.
The efficacy of day-to-day high-intensity interval training (HIIT) monitored by power on a cycloergometer, initially at a minimum of 91% HRmax, was effective. Although the increase in VO2max in all three types of training was similar to that reported in the literature, no differences or additional advantages of any of the intensive regimes were observed [28]. As demonstrated, this regime in designed percentages and intensities spent in certain zones has a significant training effect on power output and VO2max [29]. Both sprint interval training (SIT 30-s all-out bouts, together 6 min in sprint power range weekly) and high-intensity interval training (HIIT > 90% of HRmax, together 48 min/week) three times weekly are other ways to improve cycling performance. Participants improved their VO2max by 4.5 and 4.4, respectively, and the SIT group benefited additionally from a higher sum of skinfold reduction (36.3 vs. 20.5 mm) [30].
As evaluated in the present study, all intensive or high-intensity cycling regimes, irrespective of the exact interval design and session plan, could be a cause of apprehension during the COVID-19 pandemic. Based on the observations of the present study, the professional and amateur cyclists did not significantly reduce the frequency and volume of training sessions. A decrease in HIIT was noted and a weak tendency to reduce intensive training volume (80–90% HRmax). But the overall weekly TSS did not change, suggesting that intensity was substituted partially by an increase in low- to middle-intensity volume training. This is rational because of infection avoidance and risks described in the literature after intensive sessions [14, 15]. Roche et al. even reported an increase in the duration of training in 31% of athletes, with a mean increase from 92 to 103 min per day during the pandemic. But the mean heart rate remained unchanged. This partially corresponds to our results, but the results can be highly location-specific. Additionally, the cited study was performed on a very inhomogeneous group of 131 runners, cyclists and triathletes [31]. In another study conducted among 65 runners, the training pattern during the pandemic changed towards an increase in volume but the intensity did not change [32]. Muriel et al. reported a decrease in weekly training volumes by 25.8–52.2% in zones Z1 to Z6 except for the aerobic Z2. This caused the reduction of 5 and 20 min performances among 18 professional cyclists [33]. In contrast, elite athletes in Italy reduced their energy expenditure (MET) and hours of training. However, the studied athletes were very heterogenous; individual elite athletes completed a greater number of training sessions during COVID-19 compared to team athletes [19]. Both aerobic and resistance interval training is adequate for improving stable coronary heart disease [30]. Although maintaining at least low to middle intensive training could not be beneficial for cycling efficiency progress, it may better stimulate the immune system against infectious respiratory diseases. During a pandemic, reasonable training in accordance with better life hygiene (diet, sleep) should be recommended [16, 17].
Previous viral diseases, including the Middle East respiratory syndrome (MERS), have been associated with myocardial injury and myocarditis with troponin elevation, thought to be due to increased cardiac physiologic stress, hypoxia, or direct myocardial injury [34, 35]. Athletes should be aware of additionally generating hypoxia because acute heart failure can be the primary presenting manifestation of COVID-19 infection. One study found that COVID-19-induced cardiomyopathy occurs in 33% of patients with the infection [36]. Another study found that heart failure was present in 24% of patients and was associated with an increased risk of mortality, even when nearly half had no known history of hypertension or cardiovascular disease [37]. Up to 20–30% of patients hospitalized with COVID-19 have evidence of myocardial involvement, but this percentage in subclinical or mild symptoms of disease remains unknown [38]. Athletes are a special subgroup of patients, and given the rapidly evolving knowledge base about the virus and changing governmental and public health recommendations, it is difficult to provide precise answers to this highly relevant question. For athletes suffering from flu-like symptoms, myocarditis has always been a potential complication of viral syndromes. While serum biomarkers of myocardial damage are commonly elevated in the acute stages, it is important to note that raised troponins do not equate to a diagnosis of myocarditis and may be secondary to intensive physical training. For those that have fully recovered without ongoing cardiovascular symptoms (symptom-free at least for 7 days and no sooner than day 10 from the onset of symptoms), it is recommended to carry out cardiac testing, including 12-lead ECG and echocardiography, and, if the results are abnormal or the symptoms are persistent or prolonged, additional MRI. Measuring serum cardiac troponin should be confined to athletes with ongoing symptoms compatible with myocarditis and those with imaging studies that reveal impaired myocardial function [39]. However, in rare cases, patients returning to high-level sport following confirmed myocarditis require a 3–6-month period of complete rest [40]. As shown in our study, the COVID-19-positive cyclists decreased their training intensity temporarily. To clarify, their return to training due to lack of information was not supervised as part of this research and could include cardiologic examination, troponins, MRI, and ECG, but we cannot exclude independent decisions to return to physical activity. Many athletes with confirmed COVID-19 on PCR testing are minimally symptomatic or asymptomatic. Return to outdoor exercise 7 days or later after two negative SARS-CoV-2 tests carries a very low risk of infecting others. According to guidelines, including omicron variants, routine medical investigation for athletes, including cardiac screening, is not recommended in those returning to exercise following COVID-19. The protocol for return to exercise for recreational and elite athletes assumes a stepwise (50%/75%/100%) increase of training intensity every 3 days [41].
There are a number of studies reporting on the effect of the COVID-19 pandemic on mental health and quality of life in the general population [42]. It was reported that 37% experience post-traumatic stress symptoms, 17% depression, 21% anxiety, 7% insomnia, while 22% suffer an increased stress level [43]. One of the present study’s unexpected observations was the higher physical, social relation, and environmental domain results in WHOQOL scoring among cyclists with a history of SARS-CoV-2 infection, but not in the psychological domain. The psychological domain was the only one that did not increase. We hypothesize that cyclists are highly individual athletes with good self-motivation, thus retaining a good psychological state with the experience of mild symptoms of COVID-19, producing the subjective evaluation of other domains: “I’m strong, nothing bad happened to me”. A similar tendency was observed when cyclists were asked whether they knew a person who had died from COVID-19 or not. In this case, the psychological domain was also less favorable, with a lower score in athletes who had experienced bereavement, while other domains did not change. General norms for the WHOQOL-BREF domains were found to be higher than in our study: in non-pandemic conditions, 73.5 (SD = 18.1) for the physical health domain, 70.6 (14.0) for psychological well-being, 71.5 (18.2) for social relationships, and 75.1 (13.0) for the environmental domain [44]. We could speculate that higher scores in the somatic, social and environmental Quality of Life questionnaire in those cyclists that were infected by SARS-CoV-2 as compared to those that were not infected could represent a reduction in pandemic fear. This is opposite to the lower quality of life described in the literature after mild and severe disease courses. Among US professional endurance athletes, more than 60% reported the negative influence of the pandemic on training motivation, and 28% felt depressed. However, the authors did not analyze the impact of past SARS-CoV-2 infection on the eventual resolution of these symptoms [31]. In Italian elite athletes, self-determined motivation during COVID-19 was higher in individual than team athletes, elite vs. non-elite, and females vs. males. A significant positive relationship was observed between distress and mental health and intolerance of uncertainty and physical health [19]. The results obtained among cyclists who recovered from SARS-CoV-2 infection suggest that it is an important factor contributing to the quality of life of athletes under stressful and uncertain situations.
During lockdown in Austria, the psychological domain was observed to be similar and correlated positively with higher-income work activity [45]. The WHOQOL-BREF psychological domain was strongly dependent on physical activity; the authors observed mean scores of 62.8, 64.1, 69.1, 70.3, and 73.2 in cases with 0, 1, 2, 3 and 4 days of physical activity, respectively [45]. Our study’s overall mean psychological domain score was 66.2 ±12.2 and was also positively correlated with training frequency (Rs = 0.20, p = 0.02). Interestingly though, we observed a stronger positive correlation between training frequency, volume, and intensity with the physical domain than with psychological status. The association between physical activity and mental health, as found in our study, is well established. Increased duration and greater intensity of physical activity were both associated with a further reduction in the prevalence of depression in men [46].
In a study of physically active pregnant women in the second trimester, the WHOQOL psychological, social, and environmental domains did not correlate with the intensity of physical activity and volume. In the physical domain, a weak (Rs = 0.16) correlation between WHOQOL and highest intensity activity was observed [47]. It could also be speculated that a lower social domain score among cyclists resulted from isolation from general society to concentrate on healthy living and maintaining year-to-year goals in training. In this situation, the dominant role of training patterns should be emphasized in the physical domain, which by the way kept them also relatively psychologically healthy.
The study limitations should also be stressed. Firstly, the research encompassed a group of cyclists in Poland, and caution needs to be taken in extrapolating the findings to groups of such athletes in other countries, as the epidemiological situation, imposed restrictions, and available resources may differ. Secondly, the study employed an anonymous online questionnaire, which was an appropriate approach during the pandemic and enabled a relatively high number of participants to be reached. Additional limitations are the incomplete availability of the TSS score and VO2max and the online sampling method.
In conclusion, cyclists maintained their volume and frequency of training during the pandemic compared to 2019. Still, they reduced the intensity of training by lowering the time spent on high-intensity intervals. Also, changes in the pattern were more likely to have been affected by their physical status rather than by their psychogenic condition. Moreover, the training pattern of cyclists who experienced death of family members or friends due to COVID-19 remained unaffected; however, they obtained lower psychological domain scores in WHOQOL.