Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
GASTROENTEROLOGY / CLINICAL RESEARCH
Application of dietary training combined with acupuncture based on syndrome differentiation for treating dysphagia in stroke rehabilitation patients
1
Ankang Hospital of Traditional Chinese Medicine, Shanxi, China
Submission date: 2025-03-19
Final revision date: 2025-04-21
Acceptance date: 2025-04-25
Online publication date: 2025-06-08
KEYWORDS
TOPICS
ABSTRACT
Introduction:
Stroke-induced dysphagia significantly impacts patients’ nutritional status, quality of life, and rehabilitation outcomes. Conventional therapy primarily involves dietary training, while acupuncture and moxibustion have been used in complementary medicine. This study aims to evaluate the efficacy of combining dietary training with acupuncture and moxibustion based on syndrome differentiation in improving dysphagia outcomes in stroke rehabilitation patients.
Material and methods:
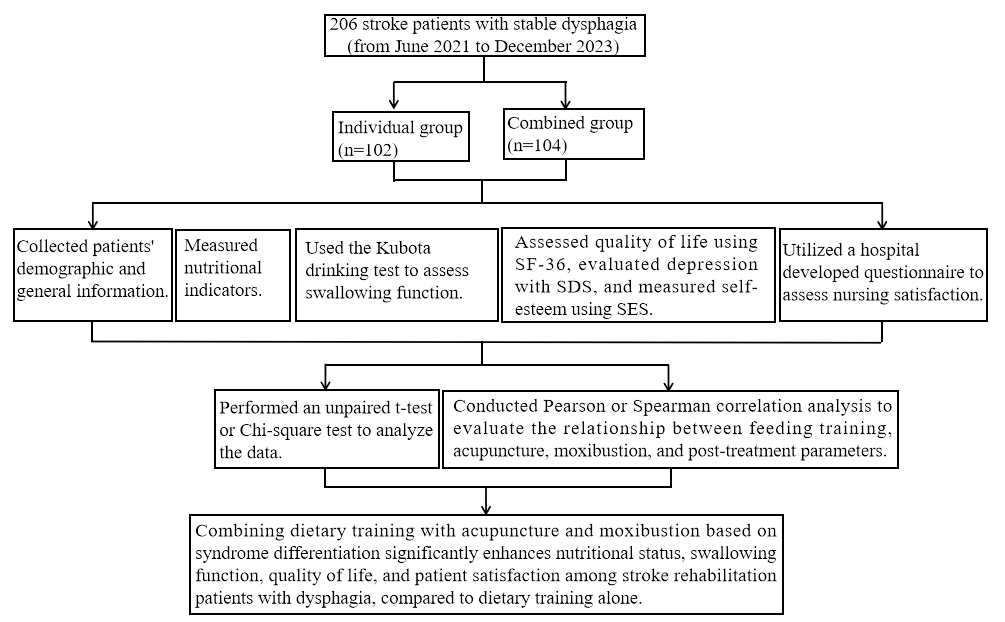
A retrospective cohort study, conducted from June 2021 to December 2023, included 206 stroke patients (aged 40 to 80 years) with stable dysphagia. Patients were divided into two groups: an individual treatment group (n = 102) receiving standard dietary training, and a combination treatment group (n = 104) receiving dietary training with acupuncture and moxibustion. The intervention lasted 6 weeks. Nutritional status, swallowing function (evaluated via Kubota drinking test and videofluoroscopic swallowing study – VFSS), quality of life, depression, self-esteem, and patient satisfaction were assessed before and after treatment.
Results:
Pre-treatment demographics and clinical characteristics showed no significant differences between groups. Post-treatment results indicated significant improvements in the combination group compared to the individual group across all parameters: nutritional status (triceps skin fold – TSF, middle arm muscle circumference on the healthy side – AMS, hemoglobin – Hb, serum albumin – ALB, serum prealbumin – PA), swallowing function (Kubota test, VFSS scores: higher in combined, p = 0.028), quality of life (SF-36 scores), depression (SDS scores: lower, p = 0.022), self-esteem (SES scores: higher, p = 0.005), and patient satisfaction (70.19% vs. 54.9%, p = 0.034). Correlation analysis confirmed the positive associations between combined treatment and outcomes (e.g., post-TSF r = 0.196, p = 0.005).
Conclusions:
Combining dietary training with acupuncture and moxibustion based on syndrome differentiation significantly enhances nutritional status, swallowing function, quality of life, and patient satisfaction among stroke rehabilitation patients with dysphagia, compared to dietary training alone. This integrative approach presents a promising adjunctive therapy for post-stroke dysphagia, warranting further investigation in larger, randomized controlled trials.
Stroke-induced dysphagia significantly impacts patients’ nutritional status, quality of life, and rehabilitation outcomes. Conventional therapy primarily involves dietary training, while acupuncture and moxibustion have been used in complementary medicine. This study aims to evaluate the efficacy of combining dietary training with acupuncture and moxibustion based on syndrome differentiation in improving dysphagia outcomes in stroke rehabilitation patients.
Material and methods:
A retrospective cohort study, conducted from June 2021 to December 2023, included 206 stroke patients (aged 40 to 80 years) with stable dysphagia. Patients were divided into two groups: an individual treatment group (n = 102) receiving standard dietary training, and a combination treatment group (n = 104) receiving dietary training with acupuncture and moxibustion. The intervention lasted 6 weeks. Nutritional status, swallowing function (evaluated via Kubota drinking test and videofluoroscopic swallowing study – VFSS), quality of life, depression, self-esteem, and patient satisfaction were assessed before and after treatment.
Results:
Pre-treatment demographics and clinical characteristics showed no significant differences between groups. Post-treatment results indicated significant improvements in the combination group compared to the individual group across all parameters: nutritional status (triceps skin fold – TSF, middle arm muscle circumference on the healthy side – AMS, hemoglobin – Hb, serum albumin – ALB, serum prealbumin – PA), swallowing function (Kubota test, VFSS scores: higher in combined, p = 0.028), quality of life (SF-36 scores), depression (SDS scores: lower, p = 0.022), self-esteem (SES scores: higher, p = 0.005), and patient satisfaction (70.19% vs. 54.9%, p = 0.034). Correlation analysis confirmed the positive associations between combined treatment and outcomes (e.g., post-TSF r = 0.196, p = 0.005).
Conclusions:
Combining dietary training with acupuncture and moxibustion based on syndrome differentiation significantly enhances nutritional status, swallowing function, quality of life, and patient satisfaction among stroke rehabilitation patients with dysphagia, compared to dietary training alone. This integrative approach presents a promising adjunctive therapy for post-stroke dysphagia, warranting further investigation in larger, randomized controlled trials.
REFERENCES (45)
1.
Watkins DA. Policy priorities for preventing stroke-related mortality and disability worldwide. Lancet Neurol 2023; 22: 1096-98.
2.
Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke 2005; 36: 2756-63.
3.
Cecconi E, Di Piero V. Dysphagia--pathophysiology, diagnosis and treatment. Front Neurol Neurosci 2012; 30: 86-9.
4.
Eltringham SA, Kilner K, Gee M, et al. Factors associated with risk of stroke-associated pneumonia in patients with dysphagia: a systematic review. Dysphagia 2020; 35: 735-44.
5.
Wilkinson JM, Codipilly DC, Wilfahrt RP. Dysphagia: evaluation and collaborative management. Am Fam Physician 2021; 103: 97-106.
6.
Vose A, Nonnenmacher J, Singer ML, González-Fernández M. Dysphagia management in acute and sub-acute stroke. Curr Phys Med Rehabil Rep 2014; 2: 197-206.
7.
Reddy KM, Lee P, Gor PJ, et al. Timing of percutaneous endoscopic gastrostomy tube placement in post-stroke patients does not impact mortality, complications, or outcomes. World J Gastrointest Pharmacol Ther 2022; 13: 77-87.
8.
Bath PM, Lee HS, Everton LF. Swallowing therapy for dysphagia in acute and subacute stroke. Cochrane Database Syst Rev 2018; 10: CD000323.
9.
Lu Y, Chen Y, Huang D, Li J. Efficacy of acupuncture for dysphagia after stroke: a systematic review and meta-analysis. Ann Palliat Med 2021; 10: 3410-22.
10.
Xiong F, Song K, Huang A, Zhang H. Treatment of dysphagia after stroke with acupuncture and related therapies: a protocol for systematic review and network meta-analysis. Medicine (Baltimore) 2020; 99: e21657.
11.
Zhong L, Wang J, Li F, Bao X, Liu H, Wang P. The effectiveness of acupuncture for dysphagia after stroke: a systematic review and meta-analysis. Evid Based Complement Alternat Med 2021; 2021: 8837625.
12.
Chan YT, Zhang HW, Sun WZ, et al. Acupuncture for poststroke dysphagia: a pilot, nonrandomized, self-controlled trial. Evid Based Complement Alternat Med 2020; 2020: 4689296.
13.
Xia W, Zheng C, Zhu S, Tang Z. Does the addition of specific acupuncture to standard swallowing training improve outcomes in patients with dysphagia after stroke? A randomized controlled trial. Clin Rehabil 2016; 30: 237-46.
14.
Li L, Xu F, Yang S, et al. Tongue acupuncture for the treatment of post-stroke dysphagia: a meta-analysis of randomized controlled trials. Front Neurosci 2023; 17: 1124064.
15.
Qin S, Zhang Z, Zhao Y, et al. The impact of acupuncture on neuroplasticity after ischemic stroke: a literature review and perspectives. Front Cell Neurosci 2022; 16: 817732.
16.
Tseng CY, Hsu PS, Lee CT, et al. Acupuncture and traditional Chinese herbal medicine integrated with conventional rehabilitation for post-stroke functional recovery: a retrospective cohort study. Front Neurosci 2022; 16: 851333.
17.
Xie Y, Pan J, Chen J, Zhang D, Jin S. Acupuncture combined with repeated transcranial magnetic stimulation for upper limb motor function after stroke: a systematic review and meta-analysis. NeuroRehabilitation 2023; 53: 423-38.
18.
Xue C, Jiang C, Zhu Y, et al. Effectiveness and safety of acupuncture for post-stroke spasticity: a systematic review and meta-analysis. Front Neurol 2022; 13: 942597.
19.
Hung CYF, Wu XY, Chung VCH, Tang ECH, Wu JCY, Lau AYL. Overview of systematic reviews with meta-analyses on acupuncture in post-stroke cognitive impairment and depression management. Integr Med Res 2019; 8: 145-59.
20.
Liu J, Wang LN. Neurogenic dysphagia in traditional Chinese medicine. Brain Behav 2020; 10: e01812.
21.
Jiang H, Zhang Q, Zhao Q, et al. Manual acupuncture or combination of rehabilitation therapy to treat poststroke dysphagia: a systematic review and meta-analysis of randomized controlled trials. Evid Based Complement Alternat Med 2022; 2022: 8803507.
22.
Savcı C, Acaroğlu R. Effects of swallowing training and follow-up on the problems associated with dysphagia in patients with stroke. Florence Nightingale J Nurs 2021; 29: 137-49.
23.
Gao M, Wang Y, Xu L, et al. Safety and performance of oropharyngeal muscle strength training in the treatment of post-stroke dysphagia during oral feeding: protocol for a systematic review and meta-analysis. BMJ Open 2022; 12: e061893.
24.
Li LX, Deng K. Acupuncture combined with swallowing training for poststroke dysphagia: a meta-analysis of randomised controlled trials. Acupunct Med 2019; 37: 81-90.
25.
Wiśniewski A, Filipska K, Puchowska M, Piec K, Jaskólski F, Ślusarz R. Validation of a Polish version of the National Institutes of Health Stroke Scale: do moderate psychometric properties affect its clinical utility? PLoS One 2021; 16: e0249211.
26.
Zarkada A, Regan J. Inter-rater reliability of the Dysphagia Outcome and Severity Scale (DOSS): effects of clinical experience, audio-recording and training. Dysphagia 2018; 33: 329-36.
27.
Lee JW, Randall DR, Evangelista LM, Kuhn MA, Belafsky PC. Subjective assessment of videofluoroscopic swallow studies. Otolaryngol Head Neck Surg 2017; 156: 901-5.
28.
Wu Q, Chen Y, Zhou Y, Zhang X, Huang Y, Liu R. Reliability, validity, and sensitivity of short-form 36 health survey (SF-36) in patients with sick sinus syndrome. Medicine (Baltimore) 2023; 102: e33979.
29.
Deluca P, Foley M, Dunne J, Kimergård A. The Severity of Dependence Scale (SDS) for codeine: preliminary investigation of the psychometric properties of the sds in an online sample of codeine users from the UK. Front Psychiatry 2021; 12: 595706.
30.
Dacakis G, Erasmus J, Nygren U, Oates J, Quinn S, Södersten M. Development and initial psychometric evaluation of the self-efficacy scale for voice modification in trans women. J Voice 2024; 38: 1251.e21-e31.
31.
Bai L, Cheng H, Hu P, et al. Effect of acupuncture on post-stroke dysphagia: a randomized controlled trial. Front Neurol 2024; 15: 1391226.
32.
Fu TC, Wang GR, Li YX, et al. Mobilizing endogenous neuroprotection: the mechanism of the protective effect of acupuncture on the brain after stroke. Front Neurosci 2024; 18: 1181670.
33.
Fu X, Li H, Yang W, et al. Electroacupuncture at HT5 + GB20 promotes brain remodeling and significantly improves swallowing function in patients with stroke. Front Neurosci 2023; 17: 1274419.
34.
Lan L, Zeng F, Liu GJ, et al. Acupuncture for functional dyspepsia. Cochrane Database Syst Rev 2014; 2014: CD008487.
35.
Lv Q, Xu G, Pan Y, et al. Effect of acupuncture on neuroplasticity of stroke patients with motor dysfunction: a meta-analysis of fMRI studies. Neural Plast 2021; 2021: 8841720.
36.
Cao BQ, Tan F, Zhan J, Lai PH. Mechanism underlying treatment of ischemic stroke using acupuncture: transmission and regulation. Neural Regen Res 2021; 16: 944-54.
37.
Li M, Wang Y, Li K, Xu X, Zhuang L. The efficacy and safety of Jin’s three-needle therapy vs. placebo acupuncture on anxiety symptoms in patients with post-stroke anxiety: a study protocol for a randomized controlled trial. Front Psychiatry 2022; 13: 941566.
38.
Yan XL, Liu Z, Sun Y, et al. Individualized nutritional support for hospitalized patients with oropharyngeal dysphagia after stroke: a randomized controlled trial. Front Nutr 2022; 9: 843945.
39.
Chang MC, Choo YJ, Seo KC, Yang S. The relationship between dysphagia and pneumonia in acute stroke patients: a systematic review and meta-analysis. Front Neurol 2022; 13: 834240.
40.
Li P, Huang W, Yan YN, et al. Acupuncture can play an antidepressant role by regulating the intestinal microbes and neurotransmitters in a rat model of depression. Med Sci Monit 2021; 27: e929027.
41.
Smith CA, Hay PP, Macpherson H. Acupuncture for depression. Cochrane Database Syst Rev 2010; 1: CD004046.
42.
Lee YC, Chiu EC. Nutritional status as a predictor of comprehensive activities of daily living function and quality of life in patients with stroke. NeuroRehabilitation 2021; 48: 337-43.
43.
Yao L, Liang W, Du X, Chen Y, Huang X. Effect of acupuncture on long-term outcomes in patients with post-stroke dysphagia. NeuroRehabilitation 2022; 51: 433-41.
44.
Zhang X, Zhao J, Zheng L, Li X, Hao Y. Implementation strategies to improve evidence-based practice for post-stroke dysphagia identification and management: a before-and-after study. Int J Nurs Sci 2022; 9: 295-302.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.