Introduction
Depression is a common mental illness, affecting more than 300 million people worldwide [1]. It is a leading cause of disability worldwide and is associated with significant morbidity, mortality, and economic burden [2]. Depression has been linked to various adverse health outcomes, including increased risk of cardiovascular disease (CVD) [3]. Proposed mechanisms for this association include behavioral factors such as physical inactivity, poor diet, and smoking, as well as direct biological effects such as inflammation, autonomic dysfunction, and metabolic changes.
In 2010, the American Heart Association (AHA) introduced Life’s Simple 7 (LS7) as a metric for cardiovascular health (CVH). This measure encompasses seven key components: a well-balanced diet, abstention from smoking, maintaining a healthy body mass index (BMI), engaging in adequate physical activity, and maintaining optimal levels of blood pressure, fasting blood glucose, and total cholesterol. The initiative was aimed at enhancing population health by promoting these core aspects of cardiovascular wellness [4]. Recently, the American Heart Association expanded upon its cardiovascular health assessment tools by introducing Life’s Essential 8 (LE8) [5]. This updated metric not only retains the core elements of the original LS7 but also incorporates sleep quality indicators and features refined scoring algorithms, thereby offering a more comprehensive evaluation of cardiovascular health [5]. The LE8 represents an advanced scoring system, distinguished by its heightened sensitivity to inter-individual variations. It uniquely emphasizes the role of social determinants in both mental and overall health, focusing on factors that maintain or enhance CVH.
Adherence to healthy lifestyle habits like these has been associated with lower risk of depression in longitudinal studies [6]. However, few studies have examined the relationship between LE8 (CVH) and depression, especially in a nationally representative sample.
In this study, we analyzed data from the National Health and Nutrition Examination Survey (NHANES) to examine the association between adherence to LE8 recommendations and current depression in American adults. Exploring this relationship may provide insight into lifestyle factors influencing depression risk and highlight potential opportunities for public health initiatives targeting depression prevention.
Material and methods
Study population
The NHANES received approval from the National Center for Health Statistics’ ethics review committee. In compliance with ethical standards, all participants provided written informed consent. Moreover, the methodologies employed in this study adhered strictly to the relevant guidelines and regulations as outlined by the Centers for Disease Control and Prevention CDC (https://www.cdc.gov/nchs/data_access/restrictions.htm). Since 1999, the National NHANES has been systematically gathering data through a complex, stratified, multi-stage probability sampling method, ensuring a nationally representative cross-section of the U.S. population [7]. Each survey wave involves distinct participants. The assessment protocol encompasses both a household interview and a physical examination conducted at a Mobile Examination Center [8]. For the purpose of our study, we utilized data from the 2005–2018 cycle. It is pertinent to note that in NHANES, the assessment of depressive symptoms was limited to individuals aged 18 years and above; consequently, our analysis only included data from participants within this age group [9].
Measurement of LE8
The LE8 scoring system encompasses eight core components, divided equally into four health behaviors – diet, physical activity, nicotine exposure, and sleep duration – and four health factors – body mass index (BMI), non-high-density lipoprotein cholesterol (non-HDL cholesterol), blood glucose, and blood pressure [10]. Dietary patterns were evaluated using the Healthy Eating Index (HEI) 2015, derived from 24-hour dietary recall interviews [11]. Information on physical activity, nicotine exposure, sleep patterns, diabetes history, and medication usage was obtained via self-reported questionnaires. Physical measurements included height and weight (to calculate BMI as weight in kilograms divided by height in meters squared) and blood pressure. Laboratory analyses were conducted to measure non-HDL cholesterol, plasma glucose, and hemoglobin A1c levels from blood samples. The LE8 score calculation algorithm, previously published (Supplementary Table SI), assigns each of the eight CVH indicators a score from 0 to 100, with the total LE8 score being an unweighted average of these indicators. For categorization, high CVH corresponds to LE8 scores between 80 and 100, moderate CVH to scores between 50 and 79, and low CVH to scores between 0 and 49 [12]. Additionally, our study utilized the same thresholds to categorize health behavior and health factor scores, facilitating a focused examination of the relationships between LE8 sub-scores and biological aging.
Measurement of depression
The assessment of depressive symptoms in our study was conducted using the Patient Health Questionnaire (PHQ-9), a widely recognized and validated 9-item depression screening tool [13]. This questionnaire probes the frequency and intensity of depressive symptoms experienced over the preceding 2 weeks [14]. Respondents rate each item on a scale from 0 to 3, yielding a cumulative score ranging from 0 to 27. For the purposes of our analysis, the presence of depressive symptoms was defined as a PHQ-9 score of 5 or higher [15].
Covariates
In our analysis, a comprehensive range of socio-demographic characteristics were considered. These included age, gender, and racial categories (White, Black, and Other). Additionally, drinking status was categorized as never, former, light, moderate, and heavy drinkers [16]. In our categorization of alcohol consumption, participants were classified based on their drinking patterns. ‘Never drinkers’ were identified as those who reported consuming fewer than 12 alcoholic drinks in their lifetime. ‘Ever drinkers’ were defined as individuals who had consumed more than 12 alcoholic drinks in their lifetime, but none in the year preceding the survey. Among current drinkers, further distinctions were made: ‘heavy current drinkers’ were defined as women consuming an average of three alcoholic drinks per day and men consuming four, with both groups having five or more binge drinking episodes per month. ‘Moderate drinkers’ were identified as women consuming two drinks per day and men consuming three, with up to two binge drinking episodes per month. Participants who consumed alcohol but did not meet the criteria for moderate or heavy drinking were categorized as ‘light drinkers [17].
Statistical analysis
We first calculated descriptive statistics for all variables. Continuous variables were presented as means with standard deviations (SD), while categorical variables were expressed as frequencies and percentages. To compare characteristics between participants with and without depression, we used t-tests for continuous variables and χ2 tests for categorical variables. To examine the association between LE8 scores and depression, we performed multivariate logistic regression analyses. We constructed three models with progressive adjustment: Model 1: unadjusted model;
Model 2: adjusted for age, gender, race and alcohol use; Model 3: further adjusted for education level, marital status, alcohol consumption, and history of chronic diseases. We calculated odds ratios (ORs) with 95% confidence intervals (CIs) for each model. The LE8 score was analyzed both as a continuous variable and as a categorical variable (low, moderate, and high cardiovascular health). For the mortality analysis, we used Cox proportional hazards models to estimate hazard ratios and 95% CIs for all-cause and cardiovascular mortality associated with LE8 scores among participants with depression. The proportional hazards assumption was tested using Schoenfeld residuals. The statistical analyses for this study were conducted using R software, version 4.2.1 (R Foundation for Statistical Computing, Vienna, Austria; http://www.r-project.org). Statistical significance was determined based on a two-sided p-value threshold of less than 0.05. The analyses were confined to participants with complete data records, ensuring robustness and validity of the findings.
Results
Population characteristics
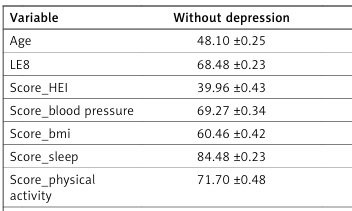
Table I presents the descriptive characteristics of the study cohort. Following meticulous screenings, a total of 29 100 participants were selected from the National Health and NHANES database (2005–2018). Among these, 2561 individuals (8.8%) were diagnosed with depression, while 26 539 participants (91.2%) were not. The mean age was 48.10 years in the group without depression and 47.17 years in those with depression (p = 0.04). Participants with depression had a significantly lower mean LE8 score compared to those without depression (58.54 vs. 68.48; p < 0.0001). Individuals with depression also had markedly lower mean scores for all components of the LE8, including diet quality score (31.40 vs. 39.96; p < 0.0001), blood pressure score (66.83 vs. 69.27; p = 0.01), body mass index score (52.09 vs. 60.46; p < 0.0001), sleep score (68.96 vs. 84.48; p < 0.0001), physical activity score (58.09 vs. 71.70; p < 0.0001), blood lipids score (60.91 vs. 64.29; p < 0.0001), smoking status score (51.82 vs. 73.09; p < 0.0001), and plasma glucose score (80.96 vs. 86.05; p < 0.0001). The proportion of participants with low cardiovascular health was substantially higher in those with depression compared to those without (27.39% vs. 10.26%; p < 0.0001). Depression was significantly more prevalent among females than males (63.91% vs. 36.09%; p < 0.0001). There were also marked disparities in the distribution of race (p < 0.0001) and alcohol drinking status (p < 0.0001) based on depression diagnosis.
Table I
Characteristics of the overall target population according to depression
Association between LE8/CVH and depression
To elucidate the association between LE8/CVH and depression, both weighted univariate and multivariate logistic regression analyses were conducted. Table II presents three distinct models: In the unadjusted model, every 1-point increment in LE8 score was associated with a 4% reduction in the odds for depression (odds ratio (OR): 0.96; 95% CI: 0.95–0.96; p < 0.0001). Compared to participants with high cardiovascular health, those with low cardiovascular health had 7.47 times higher odds (95% CI: 5.98–9.33; p < 0.0001) and those with moderate cardiovascular health had 2.70 times higher odds (95% CI: 2.17–3.36; p < 0.0001) of depression. After adjusting for age in model 1, the results were similar, with each 1-point increase in LE8 score conferring 5% decreased odds of depression (OR = 0.95; 95% CI: 0.95–0.96; p < 0.0001). In model 1, low and moderate cardiovascular health were associated with over 9 times (p < 0.0001) and over 3 times (p < 0.0001) higher odds of depression relative to high cardiovascular health. In model 2, which additionally adjusted for sex, race, and alcohol use, a robust inverse association between LE8 score and depression persisted, with every 1-point rise in LE8 linked to 5% lower odds of depression (OR = 0.95; 95% CI: 0.95–0.96; p < 0.0001). Both low and moderate cardiovascular health retained significantly elevated odds for depression of over 8 times (p < 0.0001) and nearly 3 times (p < 0.0001) compared to high cardiovascular health in the fully adjusted model. Moreover, we examined the association between the individual components constituting the LE8 score and depression. Table III presents the relationship between each LE8 subdomain and depression after adjustment for other covariates. Higher HEI score was significantly associated with lower odds of depression, with every 1-point increment corresponding to a 3% reduction (OR = 0.97; 95% CI: 0.96–0.98; p = 0.004). Blood pressure score was not significantly linked to depression (p = 0.14). In contrast, higher body mass index score conferred prominently decreased odds of depression, with every 1-point increase associated with a 28% reduction (OR = 0.72; 95% CI: 0.57–0.90; p < 0.0001). Each 1-point rise in sleep score was related to 2% diminished odds (OR = 0.98; 95% CI: 0.98–0.99; p < 0.0001). Likewise, every 1-point increment in physical activity score was accompanied by 22% lowered odds (OR = 0.78; 95% CI: 0.65–0.94; p < 0.0001). Non-high-density lipoprotein cholesterol score demonstrated a similar inverse association, with every 1-point elevation associated with a 43% reduction (OR = 0.57; 95% CI: 0.32–0.87; p = 0.03). Every 1-point increase in smoking status score was linked to 11% decreased odds (OR = 0.89; 95% CI: 0.91–0.92; p < 0.0001). Finally, higher plasma glucose score was related to substantially lower likelihood of depression, with each 1-point rise corresponding to a 24% decline in odds (OR = 0.76; 95% CI: 0.74–0.78; p < 0.001).
Table II
Association between LE8/CVH and depression
Table III
Relationship between LE8 components and depression
Association of LE8 with all-cause, heart-specific mortality
In the unadjusted model, every 1-point increment in LE8 score conferred 1.3% decreased hazard of all-cause mortality (hazard ratio [HR] = 0.987; 95% CI: 0.981–0.993; p < 0.0001, Table IV). Relative to high cardiovascular health, low cardiovascular health was associated with 6.479 times elevated hazard (95% CI: 5.334–7.870; p < 0.0001, Table IV) and moderate cardiovascular health was linked to 2.799 times higher hazard (95% CI: 2.326–3.368; p < 0.0001, Table IV) for all-cause mortality. After adjusting for age in model 1, the results were similar, with each 1-point rise in LE8 score associated with 2.3% lower hazard of all-cause death (HR = 0.977; 95% CI: 0.970–0.984; p < 0.0001, Table IV). In the age-adjusted model, low and moderate cardiovascular health were related to 3.452 times (p < 0.0001) and 1.773 times (p < 0.0001) increased hazard relative to high cardiovascular health. In model 2, which additionally controlled for sex, race/ethnicity, and alcohol use, every 1-point increment in LE8 score retained a significant 2.5% inverse association with all-cause mortality (HR = 0.975; 95% CI: 0.972–0.978; p < 0.0001, Table IV). Low and moderate cardiovascular health continued to demonstrate approximately 2.751 times (p < 0.0001, Table IV) and 1.575 times (p < 0.0001) higher hazard compared to high cardiovascular health. For heart-specific mortality, higher LE8 scores were linked to lower hazard in unadjusted and adjusted models, though cardiovascular health categories were not significantly associated.
Table IV
Association of LE8/CVH with all-cause and heart-specific mortality among depression patients
Discussion
In this nationally representative study of 29 100 U.S. adults, we detected a robust inverse association between overall cardiovascular health, assessed using the AHA’s Life’s Essential 8 metric, and presence of depressive symptoms. Individuals with depression (8.8% of participants) had markedly worse LE8 profiles across all health behavior and factor components compared to the non-depressed group. Each 1-point increment in total LE8 score was associated with 4-5% lower adjusted odds of depression in a dose-dependent manner. Categorically, the likelihood of depression was 3 times higher for moderate and over 8 times higher for low cardiovascular health relative to high cardiovascular health, even after controlling for potential confounders such as sociodemographics and alcohol use.
All eight individual LE8 components were predictive of lower depression odds, indicating the relevance of the overall cardiovascular risk factor burden in mood disorders. The strongest associations were observed for physical activity, BMI, sleep adequacy, smoking, and glucose status. With prior evidence indicating more favorable LE8 metrics among middle-aged and older versus younger adults over the past decade in the U.S. [18] and globally, our analysis highlights the necessity to improve cardiovascular health early in the life course to mitigate later risk of depressive pathophysiology.
Our findings highlight a particularly strong inverse association between BMI score and depression, with each 1-point increase in BMI score corresponding to a 28% reduction in the odds of depression. This relationship underscores the complex interplay between obesity and mental health. Obesity, a global pandemic with substantial public health implications, has been consistently linked to an increased risk of depression in epidemiological studies [19]. The bidirectional nature of this relationship is noteworthy; obesity can lead to depression through various mechanisms including social stigma, reduced physical activity, and inflammatory processes, while depression can contribute to weight gain through altered eating behaviors and decreased motivation for physical activity [20]. Adipose tissue, once considered merely an energy storage depot, is now recognized as an active endocrine organ that secretes various hormones and cytokines, potentially influencing mood regulation [21]. Moreover, obesity and depression share common pathophysiological pathways, including dysregulation of the hypothalamic-pituitary-adrenal axis and alterations in neurotransmitter systems [22]. The strong association observed in our study between improved BMI scores and lower depression risk emphasizes the potential mental health benefits of addressing obesity through lifestyle interventions. This finding aligns with emerging evidence suggesting that weight loss interventions may have positive effects on depressive symptoms [23]. Given the global obesity epidemic and rising prevalence of depression, our results underscore the importance of integrated approaches to tackle these interlinked public health challenges.
Among the 2561 participants with depression, higher LE8 scores were related to substantially reduced hazard of all-cause mortality in adjusted models. Relative to high cardiovascular health, the nearly 2750 individuals with low or moderate cardiovascular health experienced a 2 to 3 times higher mortality risk over follow-up. These observations underscore the prognostic value of evaluating cardiovascular health both quantitatively through the LE8 score and qualitatively via stratified risk categories in this high-risk subgroup with mood disorders. Targeting poor health behaviors and risk factor control encompassed in the LE8 framework could confer significant morbidity and mortality benefits.
Several mechanisms may underlie the inverse link between cardiovascular health and depression observed here. Cardiovascular wellness entails avoidance of pro-inflammatory factors such as smoking, obesity, and dyslipidemia, which can trigger systemic inflammation – a proposed pathophysiological process in depression [24]. Healthy diets and regular physical activity may also confer antioxidant and anti-inflammatory effects [25]. Maintaining ideal blood pressure and blood glucose reduces the likelihood of cerebrovascular damage, which predisposes to late-life depression [26]. Neuroendocrine pathways have been implicated as well, as favorable lifestyle habits can optimize functioning of the hypothalamic-pituitary-adrenal axis and autonomic nervous system [27]. Population studies have revealed a potential role for brain-derived neurotrophic factor, which promotes neurogenesis [28]. Higher brain-derived neurotrophic factor levels are associated with regular exercise, healthier diets, and abstention from smoking – relationships that may mediate reduced depression susceptibility [29]. Ultimately, the mechanisms underpinning the observed inverse association between cardiovascular wellness and depression risk are likely multifactorial.
Our analysis carries important public health and clinical implications. As a modifiable indicator, Life’s Essential 8 provides a useful framework for enhancing cardiovascular and mental health at the population level through lifestyle optimization. Our study indicated that even moderately improving LE8 and its constituent components may considerably reduce the likelihood of depression. Consequently, public health initiatives promoting smoking cessation, healthy dietary patterns, routine physical activity, and ideal biometric levels could meaningfully lower the depression burden. In clinical settings as well, our findings highlight lifestyle optimization as an impactful approach for mitigating depression risk among patients, including those with established cardiovascular disease. Lifestyle modification programs may effectively complement conventional pharmacotherapy for improving mental health outcomes. The composite LE8 metric can serve as an invaluable tool for systematically tracking patient progress. While lifestyle optimization represents a promising depression prevention strategy, we acknowledge that the efficiency of interventions targeting diet, activity, sleep and other behaviors is variable. Simply providing education or basic recommendations often fails to produce lasting behavior change or measurable mental health benefits. However, evidence suggests that certain modalities can yield meaningful impacts. Approaches utilizing motivation-enhancing techniques, social support integration, mobile health technologies and complementary therapies appear relatively potent for supporting adherence and achieving reductions in depression susceptibility across diverse populations [30, 31]. However, it is important to acknowledge a potential limitation in our study design regarding the overlap between some components of the LE8 score and common symptoms of depression. Specifically, sleep disturbances, changes in eating habits, and fluctuations in body weight are not only components of the LE8 score but also frequently observed symptoms of depression. This overlap may introduce a potential bias, possibly leading to an overestimation of the association between higher LE8 scores and lower depression risk. Severe depression cases might be inadvertently excluded from the high LE8 score category due to these symptom-related factors. Furthermore, it is important to acknowledge that lifestyle quality, as reflected in the LE8 score, is intrinsically linked to socioeconomic factors such as income and various social determinants of health. These factors are often deeply entrenched and difficult to change, yet they significantly impact both cardiovascular health and depression risk. Our study, while controlling for some sociodemographic variables, may not fully capture the complex interplay between socioeconomic status, lifestyle behaviors, and mental health outcomes. To address this limitation, future studies could consider conducting sensitivity analyses that exclude these overlapping components from the LE8 score. Additionally, longitudinal studies would be valuable in elucidating the temporal relationship between changes in LE8 components and the onset or progression of depression, helping to disentangle the complex interplay between cardiovascular health factors and depressive symptoms. Despite this limitation, our findings still provide valuable insights into the relationship between overall cardiovascular health and depression risk, emphasizing the need for integrated approaches in mental and cardiovascular health care. Lifestyle modification programs may effectively complement conventional pharmacotherapy for improving mental health outcomes. The composite LE8 metric can serve as an invaluable tool for systematically tracking patient progress.
In conclusion, this nationally representative study of U.S. adults reveals a robust inverse association between cardiovascular health measured by the AHA’s Life’s Essential 8 metrics and depression burden. Superior cardiovascular health correlates markedly with lower odds of depression, independent of confounding factors. These discoveries highlight that promoting healthy lifestyles and biometric targets through public health initiatives could effectively mitigate depression susceptibility in populations.