Introduction
Neck pain is a prevalent musculoskeletal issue that profoundly affects individuals’ health and well-being [1]. From mild discomfort to severe disability, its symptoms can impair daily activities, academic performance, and overall quality of life [2, 3]. The burden of neck pain extends beyond individual suffering, presenting substantial challenges to healthcare systems and society [3]. Despite its global recognition as a significant health concern, research on the prevalence of neck pain among adolescents and young adults has been limited [4]. This study aims to fill this gap by examining temporal trends in neck pain prevalence among individuals aged 10–24 years from 1990 to 2019. Given the unique vulnerabilities and developmental stages of young adults, understanding the trajectory of neck pain in this demographic is crucial for targeted interventions and improved public health outcomes.
Recent research on neck pain has seen significant advancements across various domains, contributing to a better understanding of its etiology, prevalence, mechanisms, and management strategies [3, 5, 6]. Epidemiological studies have played a crucial role in mapping the prevalence and impact of neck pain across different populations and age groups, highlighting its pervasive nature and substantial burden on individuals and healthcare systems [6–8]. Moreover, research has identified a multitude of risk factors associated with neck pain, including biomechanical, psychosocial, and lifestyle factors [9, 10]. These findings underscore the complex interplay between physical and psychosocial factors in the onset and persistence of neck pain. Overall, recent research progress has enhanced our understanding of the complexity of neck pain and provided evidence-based strategies for its prevention, management, and rehabilitation [11, 12]. Continued efforts in research and clinical practice are essential to further advance our knowledge and improve outcomes for individuals affected by neck pain.
The Global Burden of Disease (GBD) project has reshaped our understanding of global health dynamics [13–15]. By collaborating with governments worldwide, it offers insights into various health conditions, including neck pain [13]. In our study, we analyzed GBD data to examine neck pain incidence and mortality rates among adolescents and young adults aged 10–24 across 204 countries from 1990 to 2019. Our findings aim to guide evidence-based interventions to reduce neck pain burden and improve health outcomes globally for this demographic.
Material and methods
Study design and data sources
In this study, we conducted an extensive analysis using data from the Global Health Data Exchange (GHDx), which offers a comprehensive compilation of cross-sectional data on the GBD 2019 [13, 16]. This dataset spans a wide range of health conditions, including 369 diseases and injuries, across 204 countries and territories from 1990 to 2019. To identify cases of neck pain, we employed standardized procedures and diagnostic codes developed by international health organizations [13, 17]. Neck pain was defined as any discomfort or pain localized in the cervical spine region, irrespective of its underlying cause [3].
Our data collection efforts encompassed individuals of both sexes, spanning three distinct age groups: 10–14 years, 15–19 years, and 20–24 years [13, 18]. Adolescence marks a pivotal transitional period characterized by significant biological maturation and profound shifts in social dynamics and behavior. As defined by the WHO, this developmental phase spans from 10 to 19 years of age [18]. In this study, a clear distinction was made between adolescents (aged 10–19) and young adults (aged 20–24). Further granularity was achieved through delineating subgroups (10–14, 15–19, 20–24), allowing for a nuanced exploration of growth patterns and facilitating a deeper understanding of this critical life stage [19]. Additionally, we examined data across 21 regional groupings of countries that share geographic proximity and epidemiological similarities, as defined by the GBD project [20]. To contextualize our findings, we also utilized the Socio-Demographic Index (SDI) as a measure of countries’ overall development [21–23]. The SDI takes into account various socio-economic factors, including educational attainment, average income per person, and total fertility rate [21]. This index ranges from 0 to 1, with lower values indicating lower educational attainment, lower income per capita, and higher fertility rates across all GBD regions [22].
Statistical analysis
To investigate the prevalence trends of neck pain among individuals aged 10–24 years, we employed a multifaceted approach incorporating various statistical measures and analytical techniques [24]. To understand the trajectory of neck pain prevalence over time, we utilized estimated annual percentage changes (EAPCs), accompanied by their respective 95% confidence intervals (CIs) [25]. These EAPCs offer valuable insights into the direction and magnitude of changes in prevalence rates over the specified period, with an upper bound above 0 indicating an increasing trend and a lower bound below 0 suggesting a decreasing trend [8]. To derive the EAPCs, we employed a log-linear regression model, with the natural logarithm of prevalence rates (y) as the dependent variable and the calendar year (x) as the independent variable, formulated as follows: y = α + βx + ε; EAPC = (eβ-1) × 100%.
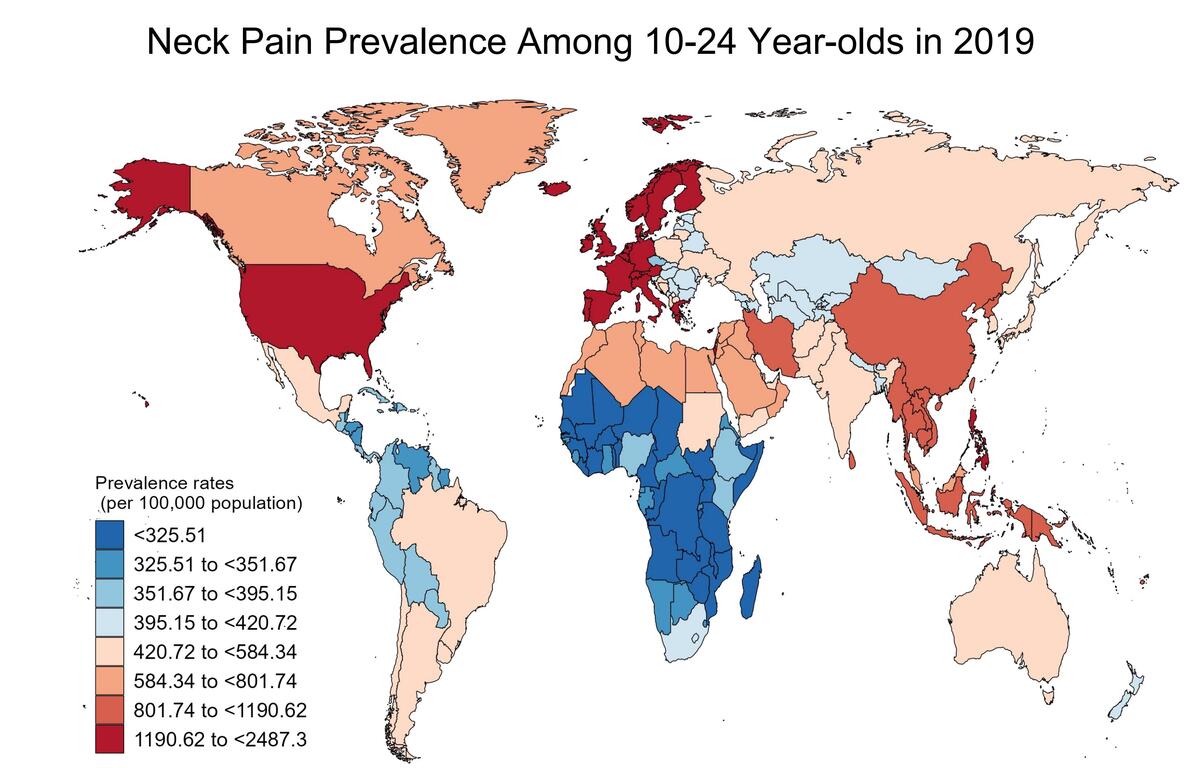
Furthermore, we conducted Pearson correlation analyses to explore the relationships between the EAPC and neck pain prevalence rates in 1990, as well as between the EAPC and the SDI in 2019. Additionally, we assessed the correlation between neck pain prevalence and SDI for all countries. The resulting correlation coefficients (ρ) and associated p-values were used to evaluate the strength and significance of these relationships. Moreover, we utilized geographic visualization techniques to illustrate the prevalence rates of neck pain among individuals aged 10–24 in each country in 2019. Furthermore, we depicted the EAPC trends from 1990 to 2019 using global maps. These visualizations provide a comprehensive overview of the geographical distribution and temporal trends of neck pain burden among adolescents and young adults across different regions.
All statistical analyses and visualizations were conducted using R software (v3.5.2) (http://www.r-project.org/) and GraphPad Prism (v8.02) (https://www.graphpad-prism.cn/), ensuring the robustness and accuracy of our research findings.
Results
Global estimates of neck pain prevalence among adolescents and young adults
Globally, the prevalence and trends in the occurrence of neck pain among adolescents and young adults from 1990 to 2019 are illustrated in Figure 1. The number of cases increased from 11,594,119 in 1990 to 12,880,134 in 2019, as depicted in Figure 1 A. Notably, the number of cases among females slightly exceeded that of males, with 5,934,098 cases in males and 6,946,036 cases in females in 2019 (Table I). Despite the rising number of cases, the prevalence rates of neck pain among adolescents and young adults, both male and female, remained relatively stable over the 30-year period (EAPC = –0.28), decreasing from 74,850.57 per 100,000 individuals in 1990 to 69,178.4 per 100,000 individuals in 2019 (Figure 1 B, Table I).
Table I
Global prevalence rates and their change trends of neck pain in individuals aged 10–24 from 1990 to 2019
Figure 1
Trends in neck pain prevalence in adolescents and young adults aged 10–24 years, 1990 to 2019. A – Prevalent cases of neck pain by sex. B – Prevalence rates of neck pain by sex. C – Prevalent cases of neck pain by age group. D – Prevalence rates of neck pain by age group
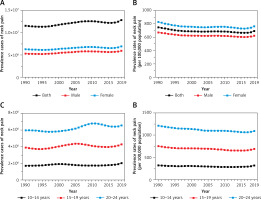
We conducted a detailed analysis among adolescents and young adults across different age groups. From 1990 to 2019, the prevalence of neck pain among individuals aged 20–24 years was significantly higher than among those aged 10-14 years and 15-19 years (Figures 1 C, D). In 2019, the prevalence of neck pain among individuals aged 20–24 years was nearly three times higher than that among those aged 10–14 years. Specifically, the prevalence rates of neck pain among adolescents and young adults aged 10–14 years, 15–19 years, and 20–24 years were 31,624.66 per 100,000, 69,189.45 per 100,000, and 109,351.52 per 100,000, respectively (Table I). The noticeable decrease in neck pain prevalence among adolescents and young adults aged 20–24 years, with an EAPC of –0.4, indicates recent advancements in neck pain prevention and treatment measures. This highlights the effectiveness of interventions specifically targeted at this age group, contributing to the overall decline in neck pain burden.
Regional differences of neck pain among adolescents and young adults
Globally, significant disparities exist in the absolute number and prevalence of cases of neck pain among adolescents and young adults, influenced by varying levels of socioeconomic development and geographic location [8, 21]. Overall, there has been a notable increase in the burden of neck pain in low SDI regions, with the number of cases rising from 633,107 in 1990 to 1,449,669 in 2019, representing a growth rate of 1.29 (Figure 2 A, Table I). However, it is worth noting that the prevalence of neck pain among adolescents and young adults is higher in regions with higher SDI, while lower SDI regions exhibit lower prevalence rates (Figure 2 B). The prevalence in high SDI regions has experienced rapid growth in recent years, reaching 152,027.17 per 100,000 individuals in 2019, possibly due to the intense workload and immense pressure faced by young individuals in today’s society [26].
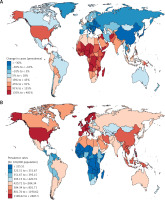
Figure 2
Regional differences in neck pain prevalence in adolescents and young adults aged 10–24 years. A – Prevalent cases of neck pain by SDI regions. B – Prevalence rates of neck pain by SDI regions. C – Prevalence rates of neck pain in 2019 in low to high SDI and 21 GBD regions
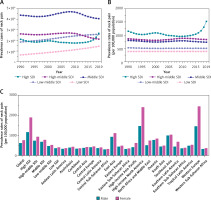
The prevalence rates of neck pain among adolescents and young adults vary significantly across different regions. In 2019, the highest prevalence rates of neck pain were observed in Western Europe (1938.57 per 100,000 individuals), high-income North America (1930.2 per 100,000 individuals), and Southeast Asia (1021.37 per 100,000 individuals), with male prevalence rates of 1458.48, 1471.36, and 1001.14 per 100,000 individuals, respectively, and female prevalence rates of 2448.27, 2409.54, and 1042.37 per 100,000 individuals, respectively (Figure 2 C). It is noteworthy that the regions experiencing continued growth in the burden of neck pain from 1990 to 2019 were Tropical Latin America, Central Asia, and Eastern Europe, with an EAPC of 0.31 (0.28 to 0.35), 0.3 (0.22 to 0.39), and 0.3 (0.12 to 0.49), respectively (Table I). Based on our analysis, we found that the prevalence of neck pain in Western Sub-Saharan Africa, Eastern Sub-Saharan Africa, and Central Sub-Saharan Africa is relatively low, with rates of 351.95, 346.18, and 319.93 per 100,000 individuals, respectively (Table I). Specifically, the prevalence rates among males are 333.05, 332.67, and 308.35 per 100,000 individuals, respectively, while among females, the rates are 369.97, 359.64, and 331.51 per 100,000 individuals, respectively (Table I). Interestingly, among these 21 geographical regions, high-income North America exhibits the most significant decline in the burden of neck pain, with an EAPC of –0.29.
These findings show that neck pain rates vary globally by location and gender. Higher rates are seen in Western Europe and high-income North America, while lower rates are observed in sub-Saharan Africa and low-income regions. In some areas, such as high-income North America, neck pain burden has decreased over time, possibly due to effective interventions. These insights are important for guiding neck pain management strategies globally.
National differences of neck pain among adolescents and young adults
Due to regional disparities, the prevalence of neck pain among adolescents and young adults varies significantly between different countries, reflecting the influence of various factors. At the national level, among the 204 countries analyzed, China, India, and the United States of America had the highest absolute numbers of cases, with 2,333,303, 1,932,061, and 1,319,629 cases, respectively, in 2019 (Figure 3 A, Supplementary Table SI). This may be attributed to the large population bases of these countries. When considering prevalence rates per 100,000 population, we found that some developed countries such as the United Kingdom, Denmark, and Finland had the highest rates, reaching 2,487.30, 2,442.03, and 2,336.94 cases per 100,000 individuals, respectively (Figure 3 B, Supplementary Table SI). Upon the same analysis, the prevalence of neck pain in Chad, South Sudan, and Niger is remarkably low, with rates of only 312.30, 312.38, and 312.82 cases per 100,000 individuals, respectively. It is noteworthy that over the past 30 years, New Zealand, the Northern Mariana Islands, and Spain have effectively managed neck pain burden, showing the most significant declines. Their EAPC was –0.56 (–0.63 to –0.5), –0.51 (–0.82 to –0.21), and –0.39 (–0.79 to 0.01), respectively (Supplementary Table SI). This positive trend emphasizes the effectiveness of interventions aimed at reducing the incidence rates of neck pain among adolescents and young adults, providing hope for further enhancements in adolescent neck pain-related health outcomes.
Correlations between EAPC, prevalence rates, and SDI in neck pain among adolescents and young adults
Based on previous epidemiological surveys, we observed a correlation between the prevalence of neck pain among adolescents and young adults and the level of SDI in different regions. This suggests an association between socioeconomic factors and the incidence of this condition. This correlation underscores the intricate interplay between socioeconomic factors and neck pain among adolescents and young adults. Subsequently, we conducted a correlation analysis of the trend in neck pain prevalence among adolescents and young adults. As shown in Figure 4 A, the trend represented by EAPC values is weakly negatively correlated with the overall incidence rate in 1990 (ρ = –0.151, p = 0.031), but not correlated with higher SDI levels (ρ = 0.02, p = 0.78) (Figure 4 B). By examining the SDI levels in different regions, we observed that regions with higher SDI levels tend to have relatively higher prevalence rates (ρ = 0.466, p < 0.001) (Figure 4 C). Similarly, at the national level, this correlation appears to be more pronounced (ρ = 0.497, p < 0.001) (Figure 4 D), which may be attributed to the diverse socioeconomic landscapes within individual countries, indicating a complex interplay of various factors influencing the prevalence of neck pain among adolescents and young adults.
Figure 4
Correlation of EAPC, prevalence, and SDI of neck pain among adolescents and young adults. A – The correlation between EAPC and prevalence rates in 1990. B – The correlation between EAPC and SDI in 2019. C – Correlation of prevalence and SDI at the regional level. D – Correlation of prevalence and SDI at the national level

Discussion
In this study, we examined the prevalence and trends of neck pain among adolescents and young adults from various perspectives. Initially, we highlighted the global trends in neck pain prevalence, taking into account both the absolute numbers and prevalence rates over the years. Despite an increase in the number of cases, we observed that the prevalence rates remained relatively stable. This suggests the need for further investigation into the factors influencing these trends. Next we investigated the age-specific prevalence of neck pain, revealing significant differences between age groups. Notably, adolescents and young adults aged 20–24 exhibited higher prevalence rates compared to younger age groups. This underscores the importance of implementing targeted interventions tailored to different age cohorts. Moreover, we examined the disparities in neck pain prevalence across different regions and countries. Our analysis revealed that factors such as socioeconomic development and geographic location play a significant role in shaping these disparities. Certain regions exhibited higher burden rates of neck pain than others, highlighting the need for tailored strategies to address this variation and ensure equitable access to care.
Recent research on neck pain has led to significant advancements in understanding its multifactorial etiology, refining assessment techniques, and developing more effective management strategies [27, 28]. Etiological studies have underscored the complex interplay between biomechanical, structural, and psychosocial factors in the development and progression of neck pain [29]. Biomechanical stressors, including poor posture and repetitive movements, have been identified as predisposing factors, while genetic predispositions and biomarkers associated with degenerative changes have provided insights into the underlying mechanisms of cervical spine dysfunction [30]. Moreover, the impact of psychosocial factors such as stress, anxiety, and depression on neck pain onset and severity has garnered increased attention, emphasizing the need for comprehensive biopsychosocial assessments [31]. Furthermore, the emphasis on preventive measures, including ergonomic modifications, lifestyle interventions, and early intervention strategies, holds great promise in reducing the incidence and burden of neck pain in the long term [32]. Overall, recent research endeavors have significantly advanced our understanding and management of neck pain, offering new avenues for improving patient care and quality of life.
Previous research reports indicate a significant increase in the number of neck pain patients and the years of life lost due to neck pain in China over the past three decades [7, 22]. Despite a slight increase in the national prevalence of neck pain, the burden of neck pain remains substantial [7]. The study also found that the prevalence of neck pain is higher in females compared to males, and the burden of neck pain in China exceeds the global average [7]. Furthermore, the study highlights a positive correlation between the burden of neck pain and the SDI, indicating a heavier burden of neck pain in economically developed regions [7]. In our study, China emerged as one of the countries with the highest number of young people with neck pain, underscoring the serious public health issue of neck pain in China and emphasizing the importance of implementing effective prevention and treatment strategies to alleviate the burden of neck diseases in the future. Another report analyzed adults aged 70 and above in Iran [33]. The point prevalence of neck pain in 2019 was 8710.6, while the incidence rate was 1334.7 per 100,000 population [33]. The prevalence, incidence, and years lived with disability (YLD) peaked in the 70–74 age group and decreased with increasing age [33]. Overall, the burden of neck pain in Iran has slightly decreased over the past three decades but remains quite serious, surpassing other regions in the area. Our study focuses on analyzing the burden of neck pain in the 10–24 age group, emphasizing the need to initiate prevention programs at a young age to reduce attributable burdens later in life.
Numerous physiological and psychosocial factors may contribute to chronic neck pain, yet there remains limited understanding of the anatomical, psychological, social, and occupational factors associated with chronic pain [34]. Consequently, researchers have begun to explore various interventions to prevent the onset of neck pain and halt its progression to chronic pain and disability [32]. The use of medication and other interventions to prevent the occurrence of neck pain in asymptomatic high-risk individuals has been found to incur greater costs than benefits; thus these methods are not indicated [35, 36]. A meta-analysis revealed that health education does not prevent the onset of neck and back pain [37]. Another review, which included multiple controlled studies, found that exercise is effective in preventing neck and lower back pain, although there is no evidence either supporting or refuting the effectiveness of ergonomics or modifying risk factors [38]. For acute whiplash injury patients, a large randomized controlled study involving 405 emergency room patients found that adding a health education video to routine treatment resulted in a 7.9% decrease in the proportion of patients still experiencing pain at week 24 compared to those receiving routine treatment alone (95% confidence interval –2.0 to 17.8) [39].
While our study illuminates neck pain trends among adolescents and young adults aged 10–24 across 204 countries from 1990 to 2019, it has limitations. Data accuracy depends on quality and availability, and variations in reporting practices may introduce bias [13, 40]. Underreporting or misdiagnosis, particularly in regions with limited healthcare access, could lead to underestimated rates [20]. Additionally, our analysis may not fully address local variations in risk factors or healthcare practices. Nonetheless, our study lays the groundwork for further research and intervention efforts, with future studies aiming to enhance data quality and consider broader age ranges and geographical nuances for more targeted interventions.
Our analysis of neck pain prevalence and trends among adolescents and young adults aged 10 to 24 globally from 1990 to 2019 provided significant insights. Despite the profound impact of neck pain on individuals’ health and well-being, its prevalence has remained relatively stable over the past 30 years. Significant differences were observed among different age groups, with individuals aged 20 to 24 exhibiting notably higher neck pain prevalence compared to those aged 10 to 14 and 15 to 19. Furthermore, we observed disparities in neck pain prevalence both globally and regionally, influenced by socioeconomic development levels and geographic location. These findings provide valuable insights into the epidemiological characteristics of neck pain globally and can inform the development of preventive and intervention strategies to reduce its burden and improve health outcomes.