Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
GASTROENTEROLOGY / CLINICAL RESEARCH
Bidirectional associations of depression, anxiety, sleep disorders, and constipation: insights from Mendelian randomization
1
Department of Psychiatry, Xiamen Xianyue Hospital, Xianyue Hospital Affiliated with Xiamen Medical College, Fujian Psychiatric Center, Fujian Clinical Research Center for Mental Disorders, Xiamen, Fujian, China
2
Xiamen Cardiovascular Hospital of Xiamen University, Xiamen University, Xiamen, Fujian, China
3
School of Clinical Medicine, Fujian Medical University, Fuzhou, Fujian, China
Submission date: 2025-03-23
Final revision date: 2025-06-15
Acceptance date: 2025-06-27
Online publication date: 2025-07-02
Corresponding author
Xinchao Chen
School of Clinical Medicine, Fujian Medical University, Fuzhou, Fujian 350122; Department of Psychiatry, Xiamen Xianyue Hospital, Xianyue Hospital Affiliated with Xiamen, Medical College, Fujian Psychiatric Center, Fujian Clinical Research Center for Mental Disorders Xiamen, Fujian 361003, China
School of Clinical Medicine, Fujian Medical University, Fuzhou, Fujian 350122; Department of Psychiatry, Xiamen Xianyue Hospital, Xianyue Hospital Affiliated with Xiamen, Medical College, Fujian Psychiatric Center, Fujian Clinical Research Center for Mental Disorders Xiamen, Fujian 361003, China
KEYWORDS
TOPICS
ABSTRACT
Introduction:
Mental health disorders and constipation are increasingly prevalent health problems worldwide. Previous studies have reported bidirectional associations between depression, anxiety, sleep disorders, and constipation. However, observational studies have yielded inconsistent results.
Material and methods:
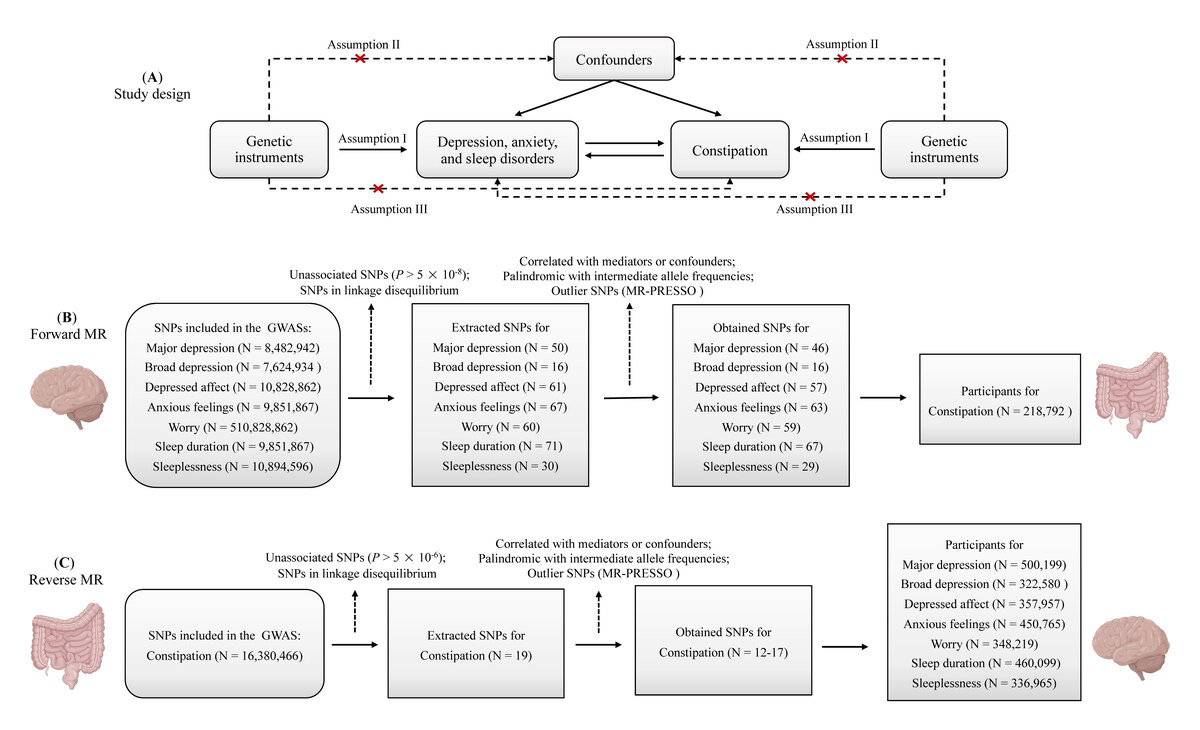
The associations were examined through a two-sample, bidirectional, univariable, and multivariable Mendelian randomization (MR) study. Summary-level data were obtained from the UK Biobank, large consortia, and the FinnGen consortium. The inverse-variance weighted method was applied as the principal analytical approach, and other additional MR methods (maximum likelihood, MR-RAPS, and MR-PRESSO) were used for sensitivity analyses. Multivariable MR analysis was performed to assess the independent effects of selected exposures.
Results:
The univariable MR analyses indicated that major depression (MD) (OR = 1.28; 95% CI: 1.12–1.46), broad depression (BD) (OR = 3.72; 95% CI: 1.55–8.97), depressed affect (OR = 1.41; 95% CI: 1.13–1.76), and worry (OR = 1.42; 95% CI: 1.13–1.77) were associated with an increased risk of constipation. There was no evidence supporting the causal effects of anxious feelings, sleep duration, and sleeplessness on constipation. The reverse MR analyses found no reverse causal association of constipation with depression, anxiety, and sleep disorders. In multivariable MR, only MD still had a robust causal association with constipation, while the effect of worry was attenuated to null, and the effects of BD and depressed affect were completely reversed.
Conclusions:
MD is causally associated with constipation, and worry might also increase the risk of constipation. Future studies are needed to confirm the causality and elucidate the underlying mechanisms.
Mental health disorders and constipation are increasingly prevalent health problems worldwide. Previous studies have reported bidirectional associations between depression, anxiety, sleep disorders, and constipation. However, observational studies have yielded inconsistent results.
Material and methods:
The associations were examined through a two-sample, bidirectional, univariable, and multivariable Mendelian randomization (MR) study. Summary-level data were obtained from the UK Biobank, large consortia, and the FinnGen consortium. The inverse-variance weighted method was applied as the principal analytical approach, and other additional MR methods (maximum likelihood, MR-RAPS, and MR-PRESSO) were used for sensitivity analyses. Multivariable MR analysis was performed to assess the independent effects of selected exposures.
Results:
The univariable MR analyses indicated that major depression (MD) (OR = 1.28; 95% CI: 1.12–1.46), broad depression (BD) (OR = 3.72; 95% CI: 1.55–8.97), depressed affect (OR = 1.41; 95% CI: 1.13–1.76), and worry (OR = 1.42; 95% CI: 1.13–1.77) were associated with an increased risk of constipation. There was no evidence supporting the causal effects of anxious feelings, sleep duration, and sleeplessness on constipation. The reverse MR analyses found no reverse causal association of constipation with depression, anxiety, and sleep disorders. In multivariable MR, only MD still had a robust causal association with constipation, while the effect of worry was attenuated to null, and the effects of BD and depressed affect were completely reversed.
Conclusions:
MD is causally associated with constipation, and worry might also increase the risk of constipation. Future studies are needed to confirm the causality and elucidate the underlying mechanisms.
REFERENCES (75)
1.
Diseases GBD, Injuries C. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020; 396: 1204-22.
2.
Organization WH. Depression and other common mental disorders: global health estimates: World Health Organization; 2017.
3.
Collaborators C-MD. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet 2021; 398: 1700-12.
5.
Hertenstein E, Feige B, Gmeiner T, et al. Insomnia as a predictor of mental disorders: a systematic review and meta-analysis. Sleep Med Rev 2019; 43: 96-105.
6.
Whiteford HA, Ferrari AJ, Degenhardt L, Feigin V, Vos T. The global burden of mental, neurological and substance use disorders: an analysis from the Global Burden of Disease Study 2010. PLoS One 2015; 10: e0116820.
7.
Hillman DR, Murphy AS, Pezzullo L. The economic cost of sleep disorders. Sleep 2006; 29: 299-305.
8.
Mugie SM, Benninga MA, Di Lorenzo C. Epidemiology of constipation in children and adults: a systematic review. Best Pract Res Clin Gastroenterol 2011; 25: 3-18.
9.
Werth BL, Christopher SA. Potential risk factors for constipation in the community. World J Gastroenterol 2021; 27: 2795-817.
10.
Adibi P, Abdoli M, Daghaghzadeh H, et al. Relationship between depression and constipation: results from a large cross-sectional study in adults. Korean J Gastroenterol 2022; 80: 77-84.
11.
Eustis SJ, McCall MW, Murphy EA, Wirth MD. Association between gastrointestinal symptoms and depression in a representative sample of adults in the United States: findings from National Health and Nutrition Examination Survey (2005-2016). J Acad Consult Liaison Psychiatry 2022; 63: 268-79.
12.
Yamamoto S, Kawamura Y, Yamamoto K, et al. Internet survey of Japanese patients with chronic constipation: focus on correlations between sleep quality, symptom severity, and quality of life. J Neurogastroenterol Motil 2021; 27: 602-11.
13.
Kawamura Y, Yamamoto S, Funaki Y, et al. Internet survey on the actual situation of constipation in the Japanese population under 70 years old: focus on functional constipation and constipation-predominant irritable bowel syndrome. J Gastroenterol 2020; 55: 27-38.
14.
Liang J, Zhao Y, Xi Y, et al. Association between depression, anxiety symptoms and gut microbiota in Chinese elderly with functional constipation. Nutrients 2022; 14: 5013.
15.
Fond G, Loundou A, Hamdani N, et al. Anxiety and depression comorbidities in irritable bowel syndrome (IBS): a systematic review and meta-analysis. Eur Arch Psychiatry Clin Neurosci 2014; 264: 651-60.
16.
Ballou S, Katon J, Singh P, et al. Chronic diarrhea and constipation are more common in depressed individuals. Clin Gastroenterol Hepatol 2019; 17: 2696-703.
17.
Wang K, Liu H, Liu J, et al. Factors related to irritable bowel syndrome and differences among subtypes: a cross-sectional study in the UK Biobank. Front Pharmacol 2022; 13: 905564.
18.
Xiao-Ling Q, Gang C, Bo L, et al. Depression is associated with constipation in patients with Parkinson’s disease. Front Neurol 2020; 11: 567574.
19.
Smith GD, Ebrahim S. ‘Mendelian randomization’: can genetic epidemiology contribute to understanding environmental determinants of disease? Int J Epidemiol 2003; 32: 1-22.
20.
Cho Y, Haycock PC, Sanderson E, et al. Exploiting horizontal pleiotropy to search for causal pathways within a Mendelian randomization framework. Nat Commun 2020; 11: 1010.
21.
Smith GD, Lawlor DA, Harbord R, Timpson N, Day I, Ebrahim S. Clustered environments and randomized genes: a fundamental distinction between conventional and genetic epidemiology. PLoS Med 2007; 4: e352.
22.
Deng Z, Buyang Z, Hou T. Visual impairment and frailty: insight from genetic correlation and Mendelian randomization. Arch Med Sci 2025; DOI: https://doi.org/10.5114/aoms/2....
23.
Burgess S, Thompson SG. Multivariable Mendelian randomization: the use of pleiotropic genetic variants to estimate causal effects. Am J Epidemiol 2015; 181: 251-60.
24.
Sanderson E, Davey Smith G, Windmeijer F, Bowden J. An examination of multivariable Mendelian randomization in the single-sample and two-sample summary data settings. Int J Epidemiol 2019; 48: 713-27.
25.
Rosoff DB, Kaminsky ZA, McIntosh AM, Davey Smith G, Lohoff FW. Educational attainment reduces the risk of suicide attempt among individuals with and without psychiatric disorders independent of cognition: a bidirectional and multivariable Mendelian randomization study with more than 815,000 participants. Transl Psychiatry 2020; 10: 388.
26.
Davies NM, Holmes MV, Davey Smith G. Reading Mendelian randomisation studies: a guide, glossary, and checklist for clinicians. BMJ 2018; 362: k601.
27.
Morneau-Vaillancourt G, Coleman JRI, Purves KL, et al. The genetic and environmental hierarchical structure of anxiety and depression in the UK Biobank. Depress Anxiety 2020; 37: 512-20.
28.
Lind MJ, Hawn SE, Sheerin CM, et al. An examination of the etiologic overlap between the genetic and environmental influences on insomnia and common psychopathology. Depress Anxiety 2017; 34: 453-62.
29.
Howard DM, Adams MJ, Clarke TK, et al. Genome-wide meta-analysis of depression identifies 102 independent variants and highlights the importance of the prefrontal brain regions. Nat Neurosci 2019; 22: 343-52.
30.
Nagel M, Jansen PR, Stringer S, et al. Meta-analysis of genome-wide association studies for neuroticism in 449,484 individuals identifies novel genetic loci and pathways. Nat Genet 2018; 50: 920-7.
31.
Howard DM, Adams MJ, Shirali M, et al. Genome-wide association study of depression phenotypes in UK Biobank identifies variants in excitatory synaptic pathways. Nat Commun 2018; 9: 1470.
32.
Power RA, Tansey KE, Buttenschon HN, et al. Genome-wide association for major depression through age at onset stratification: major depressive disorder working group of the Psychiatric Genomics Consortium. Biol Psychiatry 2017; 81: 325-35.
33.
Hyde CL, Nagle MW, Tian C, et al. Identification of 15 genetic loci associated with risk of major depression in individuals of European descent. Nat Genet 2016; 48: 1031-6.
34.
Major Depressive Disorder Working Group of the Psychiatric GC, Ripke S, Wray NR, Lewis CM, et al. A mega-analysis of genome-wide association studies for major depressive disorder. Mol Psychiatry 2013; 18: 497-511.
35.
Lee LO, Grimm KJ, Spiro A 3rd, Kubzansky LD. Neuroticism, worry, and cardiometabolic risk trajectories: findings from a 40-year study of men. J Am Heart Assoc 2022; 11: e022006.
36.
Davis KAS, Coleman JRI, Adams M, et al. Mental health in UK Biobank: development, implementation and results from an online questionnaire completed by 157 366 participants. BJPsych Open 2018; 4: 83-90.
37.
Dashti HS, Jones SE, Wood AR, et al. Genome-wide association study identifies genetic loci for self-reported habitual sleep duration supported by accelerometer-derived estimates. Nat Commun 2019; 10: 1100.
38.
Holub F, Petri R, Schiel J, et al. Associations between insomnia symptoms and functional connectivity in the UK Biobank cohort (n = 29,423). J Sleep Res 2023; 32: e13790.
39.
Kurki MI, Karjalainen J, Palta P, et al. FinnGen provides genetic insights from a well-phenotyped isolated population. Nature 2023; 613: 508-18.
40.
Littlejohns TJ, Holliday J, Gibson LM, et al. The UK Biobank imaging enhancement of 100,000 participants: rationale, data collection, management and future directions. Nat Commun 2020; 11: 2624.
41.
Pierce BL, Ahsan H, Vanderweele TJ. Power and instrument strength requirements for Mendelian randomization studies using multiple genetic variants. Int J Epidemiol 2011; 40: 740-52.
42.
Kamat MA, Blackshaw JA, Young R, et al. PhenoScanner V2: an expanded tool for searching human genotype-phenotype associations. Bioinformatics 2019; 35: 4851-3.
43.
Staley JR, Blackshaw J, Kamat MA, et al. PhenoScanner: a database of human genotype-phenotype associations. Bioinformatics 2016; 32: 3207-9.
44.
Verbanck M, Chen CY, Neale B, Do R. Detection of widespread horizontal pleiotropy in causal relationships inferred from Mendelian randomization between complex traits and diseases. Nat Genet 2018; 50: 693-8.
45.
Ding L, Chen Q, Liang H, Shen M, Zheng M, Li Z. Physical activities and breast cancer: a Mendelian randomization study. Arch Med Sci 2024; 20: 1957-67.
46.
Burgess S, Butterworth A, Thompson SG. Mendelian randomization analysis with multiple genetic variants using summarized data. Genet Epidemiol 2013; 37: 658-65.
47.
Zhao Q, Chen Y, Wang J, Small DS. Powerful three-sample genome-wide design and robust statistical inference in summary-data Mendelian randomization. Int J Epidemiol 2019; 48: 1478-92.
48.
Meier SM, Trontti K, Purves KL, et al. Genetic variants associated with anxiety and stress-related disorders: a genome-wide association study and mouse-model study. JAMA Psychiatry 2019; 76: 924-32.
49.
Purves KL, Coleman JRI, Meier SM, et al. A major role for common genetic variation in anxiety disorders. Mol Psychiatry 2020; 25: 3292-303.
50.
Yu K, Dai X, Bu F, et al. Sleep disorders and renal failure: exploring the role of creatinine and sleep apnea syndrome through cross-sectional studies and Mendelian randomization analysis. Arch Med Sci 2025; DOI: https://doi.org/10.5114/aoms/1....
51.
Hemani G, Zheng J, Elsworth B, et al. The MR-Base platform supports systematic causal inference across the human phenome. Elife2018; 7: e34408.
52.
Zhao Q, Wang J, Hemani G, Bowden J, Small DS. Statistical inference in two-sample summary-data Mendelian randomization using robust adjusted profile score. Ann Statist 2020; 48: 1742-69.
53.
Werth BL, Fisher MJ, Williams KA, Pont LG. Chronic constipation in the community: a national survey of australian adults. J Wound Ostomy Continence Nurs 2020; 47: 259-64.
54.
Chen HD, Bair MJ, Chang WC, et al. Similarities and differences between IBS-C and FC with regards to symptomatology, sleep quality and psychological attributes. J Formos Med Assoc 2020; 119: 75-80.
55.
Dore MP, Pes GM, Bibbo S, Tedde P, Bassotti G. Constipation in the elderly from Northern Sardinia is positively associated with depression, malnutrition and female gender. Scand J Gastroenterol 2018; 53: 797-802.
56.
Salmoirago-Blotcher E, Crawford S, Jackson E, Ockene J, Ockene I. Constipation and risk of cardiovascular disease among postmenopausal women. Am J Med 2011; 124: 714-23.
57.
Chen Z, Peng Y, Shi Q, et al. Prevalence and risk factors of functional constipation according to the Rome Criteria in China: a systematic review and meta-analysis. Front Med (Lausanne) 2022; 9: 815156.
58.
McEvoy PM, Watson H, Watkins ER, Nathan P. The relationship between worry, rumination, and comorbidity: evidence for repetitive negative thinking as a transdiagnostic construct. J Affect Disord 2013; 151: 313-20.
59.
Barlow DH, Sauer-Zavala S, Carl JR, Bullis JR, Ellard KK. The nature, diagnosis, and treatment of neuroticism: back to the future. Clin Psychol Sci 2014; 2: 344-65.
60.
Moezi P, Salehi A, Molavi H, et al. Prevalence of chronic constipation and its associated factors in pars cohort study: a study of 9000 adults in Southern Iran. Middle East J Dig Dis 2018; 10: 75-83.
61.
Cheng C, Chan AO, Hui WM, Lam SK. Coping strategies, illness perception, anxiety and depression of patients with idiopathic constipation: a population-based study. Aliment Pharmacol Ther 2003; 18: 319-26.
62.
Nordin G, Sundqvist R, Nordin S, Gruber M. Somatic symptoms in sleep disturbance. Psychol Health Med 2023; 28: 884-94.
63.
Yun BY, Sim J, Yoon JH, Kim SK. Association between insomnia and constipation: a multicenter three-year cross-sectional study using shift workers’ health check-up data. Saf Health Work 2022; 13: 240-7.
64.
Mayer EA, Savidge T, Shulman RJ. Brain-gut microbiome interactions and functional bowel disorders. Gastroenterology 2014; 146: 1500-12.
65.
Carabotti M, Scirocco A, Maselli MA, Severi C. The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems. Ann Gastroenterol 2015; 28: 203-9.
66.
Liu X, Liu H, Wei F, et al. Fecal metabolomics and network pharmacology reveal the correlations between constipation and depression. J Proteome Res 2021; 20: 4771-86.
67.
Li G, Zhang W, Hu Y, et al. Distinct basal brain functional activity and connectivity in the emotional-arousal network and thalamus in patients with functional constipation associated with anxiety and/or depressive disorders. Psychosom Med 2021; 83: 707-14.
68.
Barandouzi ZA, Starkweather AR, Henderson WA, Gyamfi A, Cong XS. Altered composition of gut microbiota in depression: a systematic review. Front Psychiatry 2020; 11: 541.
69.
Simpson CA, Diaz-Arteche C, Eliby D, Schwartz OS, Simmons JG, Cowan CSM. The gut microbiota in anxiety and depression - a systematic review. Clin Psychol Rev 2021; 83: 101943.
70.
Liu X, Zhao Z, Fan Y, et al. Microbiome and metabolome reveal the metabolic and microbial variations induced by depression and constipation. Psychogeriatrics 2023; 23: 319-36.
71.
Zhang X, Chen S, Zhang M, et al. Effects of fermented milk containing lacticaseibacillus paracasei strain shirota on constipation in patients with depression: a randomized, double-blind, placebo-controlled trial. Nutrients 2021; 13: 2238.
72.
Wallace CJK, Milev R. The effects of probiotics on depressive symptoms in humans: a systematic review. Ann Gen Psychiatry 2017; 16: 14.
73.
Chen S, Ou Y, Zhao L, et al. Differential effects of Lactobacillus casei strain shirota on patients with constipation regarding stool consistency in China. J Neurogastroenterol Motil 2019; 25: 148-58.
74.
Amdanee N, Shao M, Hu X, et al. Serum metabolic profile in schizophrenia patients with antipsychotic-induced constipation and its relationship with gut microbiome. Schizophr Bull 2023; 49: 646-58.
75.
Camilleri M, Ford AC, Mawe GM, et al. Chronic constipation. Nat Rev Dis Primers 2017; 3: 17095.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.