Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
DIABETOLOGY / CLINICAL RESEARCH
High-density lipoprotein cholesterol and nuclear factor I A in type 2 diabetes and mild cognitive impairment: biomarkers and mechanistic insights
1
Traditional Chinese Medicine Department, The Seventh Affiliated Hospital of Sun Yat-sen University, Shenzhen, China
2
Scientific Research Center, The Seventh Affiliated Hospital of Sun Yat-Sen University, Shenzhen, China
3
Shenzhen Key Laboratory of Chinese Medicine Active Substance Screening and Translational Research, the Seventh Affiliated Hospital of Sun Yat-sen University, Shenzhen, China
These authors had equal contribution to this work
Submission date: 2025-03-13
Final revision date: 2025-07-10
Acceptance date: 2025-07-23
Online publication date: 2025-09-06
Corresponding author
Taoli Liu
Shenzhen Key Laboratory of Chinese Medicine Active Substance Screening and Translational Research the Seventh Affiliated Hospital of Sun Yat-sen University No. 628 Zhenyuan Road 518107 Shenzhen, China
Shenzhen Key Laboratory of Chinese Medicine Active Substance Screening and Translational Research the Seventh Affiliated Hospital of Sun Yat-sen University No. 628 Zhenyuan Road 518107 Shenzhen, China
KEYWORDS
type 2 diabetesmild cognitive impairmenthigh-density lipoprotein cholesterolNHANESMendelian randomization
TOPICS
ABSTRACT
Introduction:
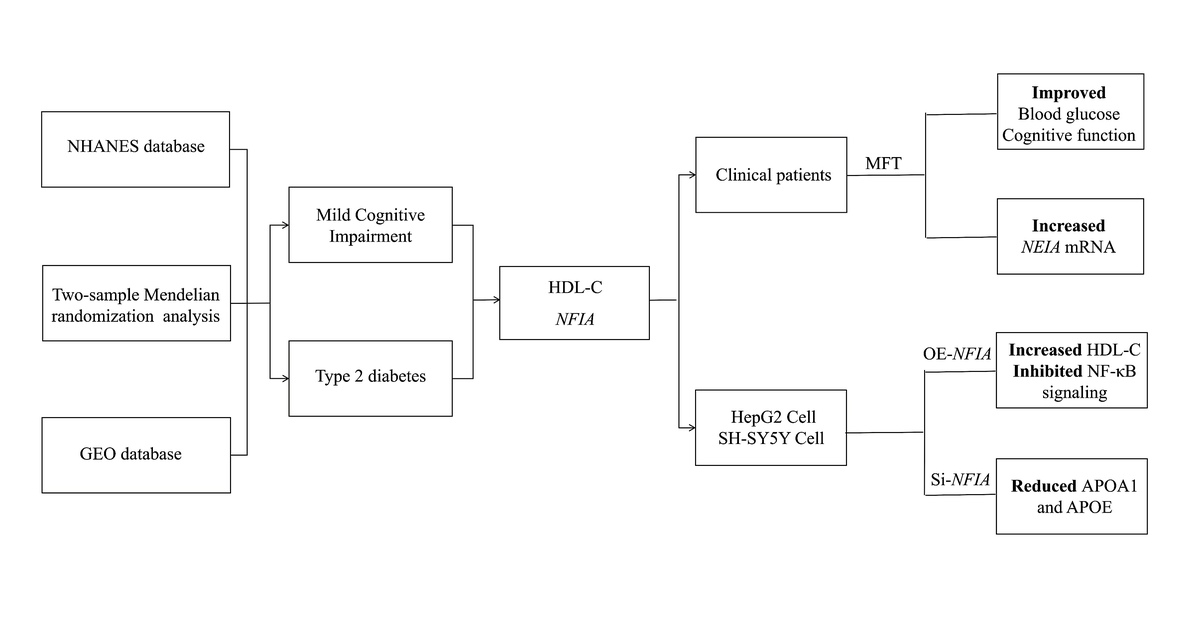
Type 2 diabetes (T2D) and mild cognitive impairment (MCI) are interrelated conditions that significantly impair quality of life. This study aimed to identify a feasible biomarker for assessing T2D-MCI risk and to evaluate a potential therapeutic strategy.
Material and methods:
We integrated data from the National Health and Nutrition Examination Survey (NHANES) with Mendelian randomization (MR) to investigate genetic causal relationships between T2D, MCI, and their shared biomarkers. Transcriptomic analysis identified T2D-associated genes. Clinical trials evaluated the short-term effects of modified fasting therapy (MFT) on glucose regulation and cognitive function. Cellular assays and patient samples were used to validate the regulatory roles of key genes in biochemical markers and downstream signaling pathways.
Results:
Among 6,356 T2D and 1,138 MCI subjects, vitamin D, high-density lipoprotein cholesterol (HDL-C), globulin, and creatinine were associated with both conditions. MR analysis showed that higher HDL-C levels reduced T2D risk (0.9059, 95% CI: 0.8666–0.9470) but increased MCI risk (OR = 1.0482, 95% CI: 1.0216–1.0755). Nuclear factor I A (NFIA) was identified as a key HDL-C regulator. In a clinical cohort (17 T2D patients and 23 controls), MFT reduced body mass index fasting glucose and HDL-C, increased NFIA expression, and improved Montreal Cognitive Assessment scores, especially in T2D-MCI patients. HDL-C rebounded at 6 months. In vitro, NFIA overexpression increased intracellular HDL-C and suppressed NF-κB signaling, while NFIA knockdown reduced APOA1 and APOE.
Conclusions:
HDL-C has divergent genetic effects on T2D and MCI. NFIA modulates HDL-C and NF-κB activity, supporting metabolic and cognitive improvements. Targeting NFIA through MFT may represent a promising strategy for T2D-MCI prevention and treatment.
Type 2 diabetes (T2D) and mild cognitive impairment (MCI) are interrelated conditions that significantly impair quality of life. This study aimed to identify a feasible biomarker for assessing T2D-MCI risk and to evaluate a potential therapeutic strategy.
Material and methods:
We integrated data from the National Health and Nutrition Examination Survey (NHANES) with Mendelian randomization (MR) to investigate genetic causal relationships between T2D, MCI, and their shared biomarkers. Transcriptomic analysis identified T2D-associated genes. Clinical trials evaluated the short-term effects of modified fasting therapy (MFT) on glucose regulation and cognitive function. Cellular assays and patient samples were used to validate the regulatory roles of key genes in biochemical markers and downstream signaling pathways.
Results:
Among 6,356 T2D and 1,138 MCI subjects, vitamin D, high-density lipoprotein cholesterol (HDL-C), globulin, and creatinine were associated with both conditions. MR analysis showed that higher HDL-C levels reduced T2D risk (0.9059, 95% CI: 0.8666–0.9470) but increased MCI risk (OR = 1.0482, 95% CI: 1.0216–1.0755). Nuclear factor I A (NFIA) was identified as a key HDL-C regulator. In a clinical cohort (17 T2D patients and 23 controls), MFT reduced body mass index fasting glucose and HDL-C, increased NFIA expression, and improved Montreal Cognitive Assessment scores, especially in T2D-MCI patients. HDL-C rebounded at 6 months. In vitro, NFIA overexpression increased intracellular HDL-C and suppressed NF-κB signaling, while NFIA knockdown reduced APOA1 and APOE.
Conclusions:
HDL-C has divergent genetic effects on T2D and MCI. NFIA modulates HDL-C and NF-κB activity, supporting metabolic and cognitive improvements. Targeting NFIA through MFT may represent a promising strategy for T2D-MCI prevention and treatment.
REFERENCES (55)
1.
Eizirik DL, Pasquali L, Cnop M. Pancreatic beta-cells in type 1 and type 2 diabetes mellitus: different pathways to failure. Nat Rev Endocrinol 2020; 16: 349-62.
2.
Liu J, Liu M, Chai Z, et al. Projected rapid growth in diabetes disease burden and economic burden in China: a spatio-temporal study from 2020 to 2030. Lancet Reg Health West Pac 2023; 33: 100700.
3.
Tomic D, Shaw JE, Magliano DJ. The burden and risks of emerging complications of diabetes mellitus. Nat Rev Endocrinol 2022; 18: 525-39.
4.
Baiano C, Barone P, Trojano L, Santangelo G. Prevalence and clinical aspects of mild cognitive impairment in Parkinson’s disease: a meta-analysis. Mov Disord 2020; 35: 45-54.
5.
Xue M, Xu W, Ou YN, et al. Diabetes mellitus and risks of cognitive impairment and dementia: a systematic review and meta-analysis of 144 prospective studies. Ageing Res Rev 2019; 55: 100944.
6.
Biessels GJ, Despa F. Cognitive decline and dementia in diabetes mellitus: mechanisms and clinical implications. Nat Rev Endocrinol 2018; 14: 591-604.
7.
Shen Z, Li ZY, Yu MT, Tan KL, Chen S. Metabolic perspective of astrocyte dysfunction in Alzheimer’s disease and type 2 diabetes brains. Biomed Pharmacother 2023; 158: 114206.
8.
Durazo AA, Weigand AJ, Bangen KJ, et al. Type 2 diabetes moderates the association between amyloid and 1-year change in everyday functioning in older veterans. J Alzheimers Dis 2024; 97: 219-28.
9.
Brandhorst S, Levine ME, Wei M, et al. Fasting-mimicking diet causes hepatic and blood markers changes indicating reduced biological age and disease risk. Nat Commun 2024; 15: 1309.
10.
Cheng CW, Villani V, Buono R, et al. Fasting-mimicking diet promotes Ngn3-driven beta-cell regeneration to reverse diabetes. Cell 2017; 168: 775-88 e12.
11.
Brandhorst S, Choi IY, Wei M, et al. A periodic diet that mimics fasting promotes multi-system regeneration, enhanced cognitive performance, and healthspan. Cell Metab 2015; 22: 86-99.
12.
Kane JP, Pillinger CR, Goldfine ID, Malloy MJ. Dyslipidemia and diabetes mellitus: role of lipoprotein species and interrelated pathways of lipid metabolism in diabetes mellitus. Curr Opin Pharmacol 2021; 61: 21-7.
13.
Poliakova T, Wellington CL. Roles of peripheral lipoproteins and cholesteryl ester transfer protein in the vascular contributions to cognitive impairment and dementia. Mol Neurodegener 2023; 18: 86.
14.
von Eckardstein A, Nordestgaard BG, Remaley AT, Catapano AL. High-density lipoprotein revisited: biological functions and clinical relevance. Eur Heart J 2023; 44: 1394-407.
15.
Vital C, Wellington CL, Calabresi L. HDL and cholesterol handling in the brain. Cardiovasc Res 2014; 103: 405-13.
16.
American Diabetes Association. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2020. Diabetes Care 2020; 43 (Suppl 1): S14-31.
17.
Ciardullo S, Perseghin G. Statin use is associated with lower prevalence of advanced liver fibrosis in patients with type 2 diabetes. Metabolism 2021; 121: 154752.
18.
Chen SP, Bhattacharya J, Pershing S. Association of vision loss with cognition in older adults. JAMA Ophthalmol 2017; 135: 963-70.
19.
Virmani MA, Cirulli M. The role of l-carnitine in mitochondria, prevention of metabolic inflexibility and disease initiation. Int J Mol Sci 2022; 23: 2717.
20.
Zhang T, Zhang L, Ke B, et al. L-carnitine ameliorated weight loss in fasting therapy: a propensity score-matched study. Complement Ther Med 2019; 44: 162-5.
21.
Liu T, Ye Z, Feng J, et al. Efficacy and safety of modified fasting therapy for weight loss in 2054 hospitalized patients. Obesity 2023; 31: 1514-29.
22.
Cukierman-Yaffe T, Gerstein HC, Colhoun HM, et al. Effect of dulaglutide on cognitive impairment in type 2 diabetes: an exploratory analysis of the REWIND trial. Lancet Neurol 2020; 19: 582-90.
23.
Lovden M, Fratiglioni L, Glymour MM, Lindenberger U, Tucker-Drob EM. Education and cognitive functioning across the life span. Psychol Sci Public Interest 2020; 21: 6-41.
24.
Han YH, Onufer EJ, Huang LH, et al. Enterically derived high-density lipoprotein restrains liver injury through the portal vein. Science 2021; 373: eabe6729.
25.
Little K, Llorian-Salvador M, Scullion S, et al. Common pathways in dementia and diabetic retinopathy: understanding the mechanisms of diabetes-related cognitive decline. Trends Endocrinol Metab 2022; 33: 50-71.
26.
Dewanjee S, Chakraborty P, Bhattacharya H, et al. Altered glucose metabolism in Alzheimer’s disease: role of mitochondrial dysfunction and oxidative stress. Free Radic Biol Med 2022; 193: 134-57.
27.
Zhang S, Lachance BB, Mattson MP, Jia X. Glucose metabolic crosstalk and regulation in brain function and diseases. Prog Neurobiol 2021; 204: 102089.
28.
Dong B, Zhou Y, Wang W, et al. Vitamin D receptor activation in liver macrophages ameliorates hepatic inflammation, steatosis, and insulin resistance in mice. Hepatology 2020; 71: 1559-74.
29.
Pittas AG, Kawahara T, Jorde R, et al. Vitamin D and risk for type 2 diabetes in people with prediabetes: a systematic review and meta-analysis of individual participant data from 3 randomized clinical trials. Ann Intern Med 2023; 176: 355-63.
30.
Gall Z, Szekely O. Role of vitamin D in cognitive dysfunction: new molecular concepts and discrepancies between animal and human findings. Nutrients 2021; 13: 3672.
31.
Scarmeas N, Anastasiou CA, Yannakoulia M. Nutrition and prevention of cognitive impairment. Lancet Neurol 2018; 17: 1006-15.
32.
Holmes MV, Ala-Korpela M, Smith GD. Mendelian randomization in cardiometabolic disease: challenges in evaluating causality. Nat Rev Cardiol 2017; 14: 577-90.
33.
Davies NM, Holmes MV, Smith GD. Reading Mendelian randomisation studies: a guide, glossary, and checklist for clinicians. BMJ 2018; 362: k601.
34.
Li Z, Lai J, Wen et al. Higher levels of blood selenium are associated with higher levels of serum lipid profile in US adults with CKD: results from NHANES 2013-2018. Biol Trace Elem Res 2023; 201: 5501-11.
35.
Corder EH, Saunders AM, Strittmatter WJ, et al. Gene dose of apolipoprotein E type 4 allele and the risk of Alzheimer’s disease in late onset families. Science 1993; 261: 921-3.
36.
Serrano-Pozo A, Das S, Hyman BT. APOE and Alzheimer’s disease: advances in genetics, pathophysiology, and therapeutic approaches. Lancet Neurol 2021; 20: 68-80.
37.
Zhao Y, Wang Y, Zheng H, et al. Hydrogen sulfide upregulates SIRT1 to inhibit ox-HDL-induced endothelial cell damage and mitochondrial dysfunction. Nitric Oxide 2024; 152: 78-89.
38.
Speer T, Rohrer L, Blyszczuk P, et al. Abnormal high-density lipoprotein induces endothelial dysfunction via activation of Toll-like receptor-2. Immunity 2013; 38: 754-68.
39.
Jensen NJ, Wodschow HZ, Nilsson M, Rungby J. Effects of ketone bodies on brain metabolism and function in neurodegenerative diseases. Int J Mol Sci 2020; 21: 8767.
40.
Veneti S, Grammatikopoulou MG, Kintiraki E, et al. Ketone bodies in diabetes mellitus: friend or foe? Nutrients 2023; 15: 4383.
41.
Gershuni VM, Yan SL, Medici V. Nutritional ketosis for weight management and reversal of metabolic syndrome. Curr Nutr Rep 2018; 7: 97-106.
42.
Chung JY, Kim OY, Song J. Role of ketone bodies in diabetes-induced dementia: sirtuins, insulin resistance, synaptic plasticity, mitochondrial dysfunction, and neurotransmitter. Nutr Rev 2022; 80: 774-85.
43.
Fortier M, Castellano CA, St-Pierre V, et al. A ketogenic drink improves cognition in mild cognitive impairment: results of a 6-month RCT. Alzheimers Dement 2021; 17: 543-52.
44.
Taylor MK, Sullivan DK, Mahnken JD, et al. Feasibility and efficacy data from a ketogenic diet intervention in Alzheimer’s disease. Alzheimers Dement 2018; 4: 28-36.
45.
Galetti V, Brnic M, Lotin B, Frigeri M. Observational study of lipid profile and c-reactive protein after a seven-day fast. Nutrients 2021; 13: 255.
46.
Wei M, Brandhorst S, Shelehchi M, et al. Fasting-mimicking diet and markers/risk factors for aging, diabetes, cancer, and cardiovascular disease. Sci Transl Med 2017; 9: eaai8700.
47.
Hiraike Y, Waki H, Yu J, et al. NFIA co-localizes with PPARgamma and transcriptionally controls the brown fat gene program. Nat Cell Biol 2017; 19: 1081-92.
48.
Zhao JJ, Hu YW, Huang C, et al. Dihydrocapsaicin suppresses proinflammatory cytokines expression by enhancing nuclear factor IA in a NF-kappaB-dependent manner. Arch Biochem Biophys 2016; 604: 27-35.
49.
Hu YW, Zhao JY, Li SF, et al. RP5-833A20.1/miR-382-5p/NFIA-dependent signal transduction pathway contributes to the regulation of cholesterol homeostasis and inflammatory reaction. Arterioscler Thromb Vasc Biol 2015; 35: 87-101.
50.
Hiraike Y, Saito K, Oguchi M, et al. NFIA in adipocytes reciprocally regulates mitochondrial and inflammatory gene program to improve glucose homeostasis. Proc Natl Acad Sci USA 2023; 120: e2308750120.
51.
Otocka-Kmiecik A, Mikhailidis DP, Nicholls SJ, et al. Dysfunctional HDL: a novel important diagnostic and therapeutic target in cardiovascular disease? Prog Lipid Res 2012; 51: 314-24.
52.
Ganjali S, Dallinga-Thie GM, Simental-Mendia LE, et al. HDL functionality in type 1 diabetes. Atherosclerosis 2017; 267: 99-109.
53.
Liu D, Huang Y, Huang C, et al. Calorie restriction with or without time-restricted eating in weight loss. N Engl. J Med 2022; 386: 1495-504.
54.
James DL, Hawley NA, Mohr AE, et al. Impact of intermittent fasting and/or caloric restriction on aging-related outcomes in adults: a scoping review of randomized controlled trials. Nutrients 2024; 16: 316.
55.
Arciero PJ, Poe M, Mohr AE, et al. Intermittent fasting and protein pacing are superior to caloric restriction for weight and visceral fat loss. Obesity 2023; 31 Suppl 1: 139-49.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.