In recent years, there have been many analyses on the role of steps in cardiovascular and cause-specific outcomes and mortality, evaluating not only steps/day in different populations, but also speed (cadence × stride length), variation in pace and the impact of intermittence of the physical activity [1–5]. This is of particular importance, as physical activity levels are worryingly low, with about 30% of adults globally being insufficiently active. A mere 22% of individuals over 65 years meet the WHO recommendations for minimum physical activity per week, with only 40% reporting regular physical activity and just one in five engaging in daily physical activity [2, 3]. Importantly, based on various data, physical inactivity may be attributable to as many as 3.2 million deaths per year (with 2.6 million in low- and middle-income countries), and is the fourth highest risk factor for death worldwide, ahead of unsafe sex, undernutrition, and alcohol use [6, 7]. It is also worth emphasising that the global estimate of the cost of physical inactivity to public healthcare systems between 2020 and 2030 is about US$ 300 billion (approximately US$ 27 billion per year) if levels of physical inactivity are not reduced [6].
The recent meta-analysis by Ding et al. also raised these important issues, addressing all the most important endpoints that physical activity (PA) may impact, from all-cause mortality, cardiovascular incidence and mortality, and cancer incidence and mortality, to dementia, depressive symptoms, physical function and falls [1]. The authors also attempted to examine the effect of PA using different devices (accelerometer vs. pedometer-measured steps), which is mostly raised as a limitation of similar analyses. However, they did not indicate which method is superior – information that would be useful to make recommendations regarding the optimal method for step measurement. While still requiring confirmation, it seems that what matters most is simply taking steps and engaging in physical exercise, rather than the method used to count steps [1, 5]. The authors also attempted to evaluate the effect of cadence (peak 30-min step cadence) on health benefits; however, the results were ultimately inconclusive [1]. While cadence is a significant factor in running speed, it is not the sole determinant. Optimising both cadence and stride length, along with other factors, is essential for improving speed, which may be better understood from a practical perspective [4]. Evidence suggests that pacing (variation of exercise intensity) is associated with beneficial health outcomes, even in children and adolescents [8].
Another issue requiring further investigation is what benefits we should expect when comparing the effect of steps for generally healthy individuals and those with concomitant chronic diseases, such as diabetes, cardiovascular disease and cancer [1–5]. Although the authors included patients with various conditions, they did not perform separate analyses for apparently healthy subjects and those with chronic diseases to ascertain whether the effect of PA might differ. Considering the potential plateau effect of exercise at approximately 16,000 steps, observed in many available analyses, and the ongoing debate regarding the effect of 20,000 steps or more (extremely intensive PA) on health outcomes [5, 9, 10], it is regrettable that the authors limited their analyses (even acknowledging the potential paucity of data) to around 12,000 steps/day. Given the increasing number of people engaging in extremely intensive physical activity (with daily step counts exceeding 20,000–30,000), we need to determine whether health benefits continue to follow the “more is better” rule, or whether such activity might even be harmful [5, 9, 10].
In their meta-analysis, Ding et al. compared largely sedentary individuals averaging 2,000 steps per day (typically defined as basal activity, which is arguably a low reference number, even for those with health limitations, yet observed in previous analyses) with those averaging 7,000 steps per day, demonstrating substantial benefits from increasing step counts for the endpoints investigated [1]. However, it should be emphasised that the average adult takes between 3,000 and 4,000 steps per day (approximately 2.5 km), and that walking fewer than 5,000 steps per day is considered sedentary (some studies suggest a lower threshold, e.g. < 4,300 [11]). Based on these results, which align with our previous analysis [5], a revision of the definition of a sedentary lifestyle to < 4000 steps/day should be considered. It is also somewhat surprising, and at odds with previous analyses [12], that such an increase was not associated with a significant reduction in cancer incidence, warranting further investigation, specifically examining the types of cancers considered.
Another point of discussion regarding the benefits of walking is when to start regular PA. Thus, the authors rightly identified age as a potential differentiating factor, which we addressed in our previous analysis, suggesting a significantly lesser impact of physical activity in older versus younger adults (42.3 vs. 48.7% all-cause death reduction [5]), supporting the “earlier, the better” approach for starting PA. Interestingly, the authors’ results appear to contradict the aforementioned findings. Nonetheless, similarly to our results, the greatest effect on outcomes was achieved with higher step counts for younger versus older adults (in our study, 7–13 and 6–10 thousand, respectively) [5]. However, the authors’ results might suggest that this is associated with a greater reduction of the investigated outcomes for older adults (especially for CVD incidence) [1]. Therefore, this issue still requires further investigation, and we cannot yet conclude whether differing step targets should be recommended for younger and older adults.
I believe we should also exercise caution with the wording, as we faced similar challenges after publication of our meta-analysis, which suggested significant health benefits at as few as 4000 steps/day [5]). Presenting in the meta-analysis the statistical attenuation or lack of improvement at 7000 steps and beyond for some of the investigated outcomes could be demotivating for many who currently achieve more than 7000 steps/day, particularly given that the authors’ results actually indicate the contrary. Examining the authors’ results for 12,000 steps, we observe a greater reduction, with, for example, a doubling of the risk reduction for cancer incidence (from 6 to 12%) and an additional 8% increase in all-cause death risk reduction (from 47% to 55%). Furthermore, there is a significant benefit above 7000 steps/day for all-cause mortality, cardiovascular disease incidence, cancer mortality, dementia and depressive symptoms, suggesting that more is better for longevity [1]. It would also be useful to ascertain the degree to which changes of 500 steps/day (rather than 1000/day), as assessed in our analysis, which demonstrated a further 7% reduction in cardiovascular mortality for every 500-step increase [5], might be beneficial, as this could be far more motivating for the stepwise increase in daily step count for our patients.
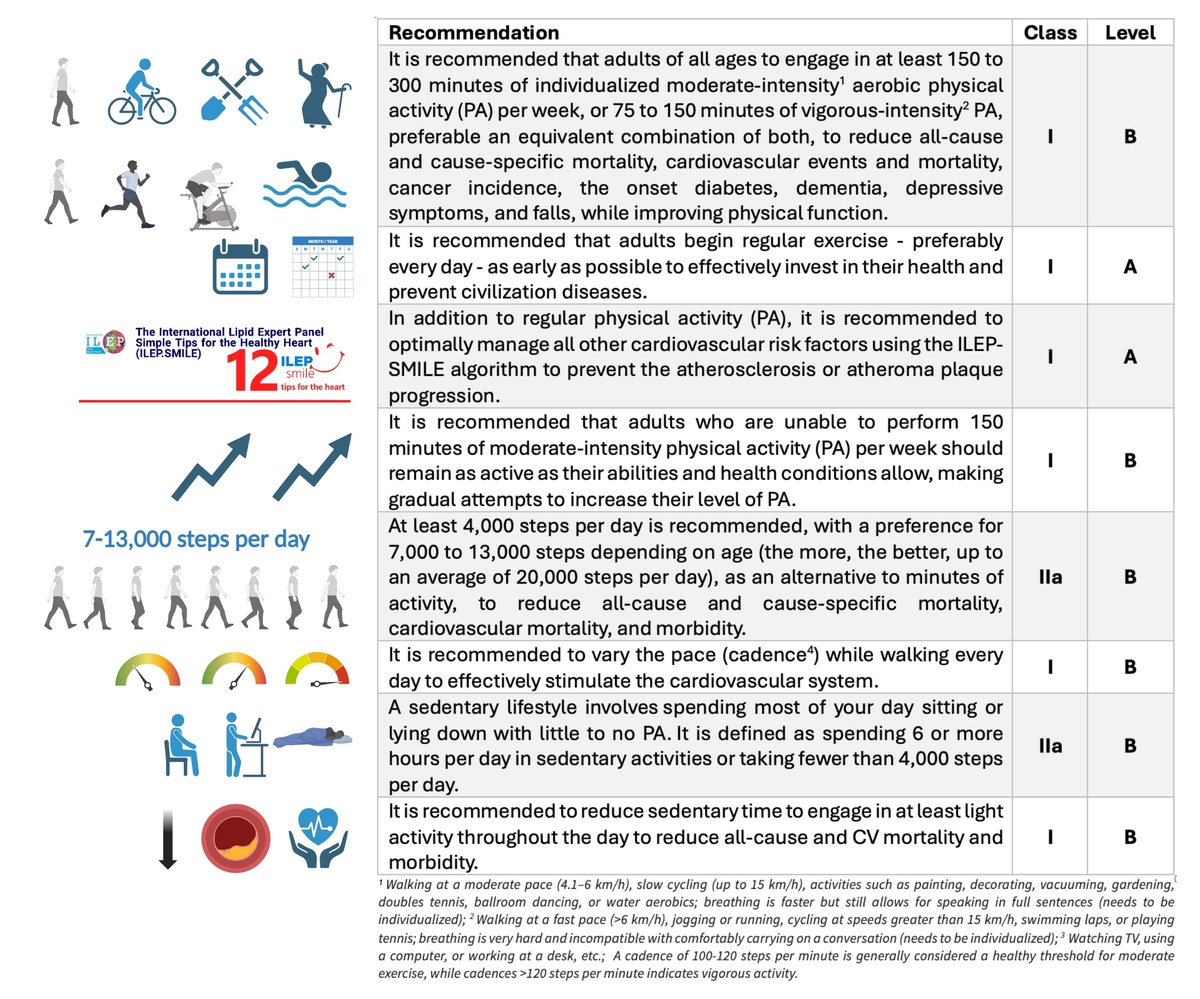
Despite some of the aforementioned points that may still raise questions for discussion, the authors of the meta-analysis [1] deserve congratulations for their remarkable effort and critically important results. Based on these findings and numerous other available data suggesting a significant association between daily steps and health outcomes [13], I firmly believe that, similarly to the recent International Lipid Expert Panel (ILEP) recommendations on simple tips for a healthy heart (ILEP-SMILE), which include step counts as part of the guidance (at least 4,000 steps per day; preferably 6–13,000 depending on age; and the more the better up to 20,000 steps/day) [10], daily step counts should be incorporated into all forthcoming guidelines (Figure 1).