Cardiovascular burden and the role of lifestyle changes
Cardiovascular disease (CVD) remains the leading cause of mortality globally, accounting for over 20 million deaths annually, with as many as 2/3 of them related to atherosclerotic cardiovascular disease (ASCVD) [1]. Historically, preventive strategies have primarily targeted sedentary behaviour, unhealthy diet, obesity, hypertension, diabetes, dyslipidemia, and tobacco smoking. Although these factors constitute a foundational approach, emerging evidence indicates that a more comprehensive and integrated strategy is necessary. Banach et al. have recently introduced and illustrated the broader approach required for optimal cardiovascular health promotion, highlighting a multidimensional, lifelong strategy that extends the approach previously recommended by Life’s Simple 7 (LS7) and the current Life’s Essential 8 (LE8) by the American Heart Association [2–4].
The conventional cardiovascular risk factors remain undeniably crucial. Physical inactivity alone contributes to approximately 6–10% of global coronary heart disease, while the burden of type 2 diabetes accounts for as many as 1 million CVD deaths annually [5]. Moreover, less than 8–9% of the adult population engages in regular everyday exercise, despite the very clear results indicating that exercise is directly associated with the prolongation of life through a reduction in blood pressure, inflammation, oxidative stress, improved lipid profile, endothelial functions, arterial stiffness, and many other risk factors [6]. The largest meta-analysis of step count also suggested that for those under 60 years of age, having an average of 7,000 to 13,000 steps per day may result in a 49% reduction in all-cause mortality. Furthermore, the benefits for reduction in cardiovascular and total mortality start as low as 4,000 steps per day (but the more, the better!) [7].
Dietary risks, particularly excessive consumption of saturated fats (SFA), trans-unsaturated fats, and added sugars, significantly contribute to disability-adjusted life years (DALYs) attributed to heart disease [8]. Diet should always be personalised, and numerous data clearly indicate that we should adopt well-balanced high-quality diets like the Mediterranean, Planetary, or Nordic diets, as well as hypolipidemic diets (with a strong emphasis on both quantity and the transition to polyunsaturated fatty acids [PUFAs]) or simply calorie restriction approaches, such as the Dietary Approaches to Stop Hypertension (DASH). Restrictive diets should be avoided and only recommended for highly selected populations that might benefit from them for a specific period, allowing them to achieve their goals and learn about healthy nutrition [9, 10]. Similarly, poor management of hypertension (still the most important CVD risk factor in relation to the mortality risk) [2] along with pre-diabetes and diabetes continues to be a significant contributor to premature cardiovascular mortality [11]. For the latter, careful monitoring of the micro- and macrovascular complications are essential to ensure early effective treatment [12]. The ongoing obesity pandemic, now recognised as the third most prevalent cardiovascular disease risk factor, alongside overweight issues affecting approximately 60% of the adult population, urgently calls for joint action [13, 14].
Sleep disturbances and cardiovascular risk
Nevertheless, the traditional framework overlooks several important dimensions that have recently been recognized as independent risk modifiers [2]. A comprehensive meta-analysis encompassing data from 34 studies and over 1.7 million participants, observed for an average of 11.6 years, broadened the scope of traditional risk factors to include sleep health, which was added in the current LE8. Optimal management across these eight risk domains was associated with a significant 53% reduction in overall cardiovascular risk (HR = 0.47; 95% CI: 0.39–0.56, p < 0.00001). This risk reduction was similarly pronounced for coronary heart disease (–56%) and stroke (–48%). Moreover, overall mortality risk was reduced by 46% (0.54; 95% CI: 0.43–0.69, p < 0.00001), with cardiovascular-related mortality reduced by 63% (0.37; 95% CI: 0.26–0.52, p < 0.00001) [15]. These findings, along with an increasing amount of evidence-based medicine regarding the impact of lifestyle changes on cardiovascular health, highlight the need to expand CVD risk assessment beyond conventional parameters. In particular, sleep duration and quality are now widely recognised as essential components of cardiovascular health. Insufficient sleep (typically less than 6 h per night) has been associated with a 20–25% heightened risk of incident CVD and a 45% increased risk of coronary heart disease [16]. Meta-analyses confirm a U-shaped relationship between sleep duration and cardiovascular and mortality outcomes. It has been shown that a 1-hour increase or decrease in sleep duration is associated with an increased risk of all-cause mortality when referenced to the mortality associated with 7 h of sleep duration (by 12% and 7%, respectively). Similar results were observed for coronary heart disease risk; compared with 7 h of sleep per day, the relative risk of coronary heart disease (CHD) was 11% higher for each 1-hour reduction and 7% higher for each 1-hour increase [17]. Our analysis also confirmed that longer sleep duration might also have harmful effects on renal function [18]. Cognitive-behavioural therapy for insomnia and digital sleep-tracking technologies represent promising, non-pharmacological interventions that can provide tangible cardiovascular benefits [2, 19].
The role of stress in cardiovascular health
To be effective, we cannot, however, overlook other critical components of life and lifestyle improvements that might significantly contribute to risk and undermine all efforts related to well-recognised risk factors. Therefore, we should also consider alcohol consumption, elevated lipoprotein(a), managing stress, and adherence to medicines and lifestyle recommendations [2]. An inseparable aspect of sleep quality is stress. Chronic stress remains an underappreciated yet significant risk factor for cardiovascular disease, with the INTERHEART study identifying psychosocial stress as having a comparable impact on myocardial infarction risk to hypertension or diabetes [20]. The role of chronic stress on the risk of depression and their joint effect on cardiovascular health cannot be also overlooked [20–22]. The physiological underpinnings involve inflammatory and neurohormonal mechanisms, highlighting the importance of integrating stress management strategies – such as mindfulness, exercise, and comprehensive counselling – into effective cardiovascular prevention [21]. However, the clinical quantification and management of stress remain challenging, highlighting the necessity for multidisciplinary intervention approaches. There should also be efforts to standardise the tests for optimal stress assessment and its connection to cardiovascular risk. Currently, standardised methods for stress assessment include questionnaires such as the Perceived Stress Scale (PSS), the Holmes and Rahe Stress Scale (HRSS), and the Occupational Stress Questionnaire (OSQ), as well as physiological measures like heart rate variability (HRV) and salivary cortisol tests [22].
Eliminate alcohol consumption for better cardiovascular health
Alcohol consumption calls for distinct consideration, especially given that the recent Organisation for Economic Cooperation and Development (OECD) Health Statistics 2024 indicate that the mean overall alcohol consumption among the population aged 15 and over in Europe remains very high, at over 10 l per adult per year, with 11 l in Poland and 11.9 litres per adult in Latvia [23]. Although moderate alcohol intake was traditionally thought to confer cardiovascular protection, recent comprehensive analyses clearly contradict this assumption. A meta-analysis involving over 600,000 individuals demonstrated increased risks of stroke and hypertension, even at moderate levels of alcohol consumption [24]. Similarly, the Global Burden of Disease (GBD) analysis suggested that any amount of alcohol is harmful, and its use is a major risk factor for the global disease burden, leading to substantial health loss. It found that the risk of all-cause mortality, particularly from cancer, increases with rising levels of consumption, and the level of consumption that minimises health loss is zero [25]. Nonetheless, individual variability, drinking patterns, and the quality of alcoholic beverages may modulate these risks, suggesting that reducing alcohol consumption should be a central focus, particularly for those already at elevated cardiovascular risk. Taking into account the current unfavourable trends in alcohol and alcohol-based beverage consumption, all forthcoming guidelines should unify their recommendations towards completely eliminating alcohol consumption.
Know your lipoprotein(a)
A pivotal advancement in cardiovascular prevention is the recent trend to transition from a short-term (10-year) risk evaluation to a lifetime risk assessment. Tools such as the PREVENT calculator developed by the American Heart Association provide sex-specific, race-neutral lifetime risk projections for adults aged 30 to 79 years [26]. Recognising lifetime risk rather than short-term estimates facilitates early, proactive preventive strategies, significantly enhancing patients’ motivation and adherence [27]. This is especially relevant to the genetically predisposed and easily monitored (lifetime) risk factor, such as lipoprotein(a) (Lp(a)), which is six times more atherogenic than LDL cholesterol and is responsible for the significant increased risk of myocardial infarction, stroke, peripheral artery disease, heart failure, or aortic valve stenosis [28]. Lp(a) should be measured at least once in each person’s lifetime, preferably in children and adolescents, to promote lifestyle changes and prevent CVD events in parents and grandparents, thereby effectively reducing the risk of premature CVD events [29, 30]. Elevated Lp(a) (> 50 mg/dl/>125 nmol/l) significantly modifies CVD risk, increasing and altering the risk category. Additionally, we have the dedicated lifetime calculator, which clearly demonstrates not only how the risk increases but also how effectively we can modulate this by optimising the treatment of other CVD risk factors (https://www.lpaclinicalguidance.com) [29]. The introduction of Lp(a) into the ILEP Simple Tips for the Healthy Heart also serves a strong educational role and addresses the significant ineffectiveness in Lp(a) measurement, as only a small percentage of patients, even those at high risk of CVD, know their Lp(a) levels [2, 28]. It is worth mentioning that Poland has recently implemented the first universal screening of Lp(a) within the “My Health” programme of the Ministry of Health, for all individuals aged 20 and over.
Education and adherence – we cannot achieve effective prevention without them
Ultimately, lifestyle changes and effective CVD prevention can only be successful if supported by good health education, which consequently leads to the optimal implementation of lifestyle changes and adherence to therapy [31]. We have accumulated sufficient data indicating that without a good education, only a small percentage of the population – those most aware – will be inclined to invest in their health as early as possible (when they are still healthy and asymptomatic). This involves continuously optimising and adapting their lifestyle, participating in health screening programmes, regularly monitoring their health, and being compliant and adherent to therapy [31–33]. We have outstanding examples of effective education, with the best referring to the programmes introduced by Prof. Valentin Fuster for school and preschool children (the FAMILIA projects, the SI! Program) [34, 35]. Attempts to introduce school Health Education subjects have already been made in other countries, including Poland (starting as a subject from 1st September 2025). Even with the best programmes and the most innovative therapies, we may still fail in CVD prevention due to nonadherence, which is an independent CVD risk factor. In the case of statin therapy, nonadherence may increase the risk of all-cause mortality by 45% [36, 37]. Education – for example, through the ILEP – Personalised Lipid Intervention Plan (PLIP) – may effectively overcome the nocebo/drucebo effect and make patients more inclined to use statin therapy [38].
The ILEP-SMILE approach
Figure 1 effectively synthesises traditional factors (diet, exercise, smoking) with previously overlooked elements: sleep hygiene, alcohol moderation, stress management, patient education, and routine risk measurement, including at least one lifetime assessment of Lp(a) plasma levels. This comprehensive model reflects an evolved understanding of cardiovascular risk as cumulative, multifactorial, and modifiable across an individual’s lifespan, highlighting patient engagement and adherence as fundamental to long-term success. Educational interventions enhancing health literacy have demonstrated the potential to reduce cardiovascular events by up to 20% in high-risk groups [39], while medication adherence, particularly to statins, remains a significant challenge, with nearly 50% discontinuation within 1 year [40]. The detailed ILEP-SMILE algorithm, along with the specific recommendations, is presented in Figure 2. The abbreviation SMILE is also not coincidental – by addressing all 12 points comprehensively, we can practically guarantee a long and high-quality life without any cardiovascular issues events.
Figure 1
The interplay of different modifiable risk factors with cardiovascular health in relation to the ILEP-SMILE approach
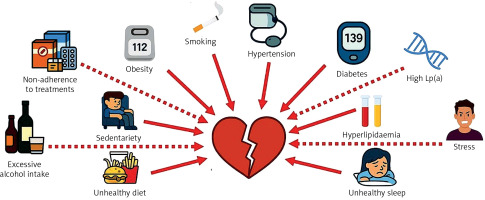
Figure 2
The International Lipid Expert Panel SiMple tIps for the heaLthy hEart (ILEP-SMILE). Details on the risk factors and suitable recommendations

Digital health innovations, such as step counters, dietary tracking apps, and HRV and sleep monitors, ideally supported by proper education, demonstrate potential in encouraging physical activity, enhancing nutritional awareness, and enabling early detection of cardiovascular anomalies [41, 42]. Integrating these digital solutions into clinical workflows enhances patient-provider communication and individualises preventive strategies. They are already and will soon commonly be completed with AI-based tools that assist, for example, based on imaging methods, not only to diagnose very early atherosclerosis (with soft atheroma plaques) but also to monitor its volume, morphology, and artery lumen, clearly demonstrating and further motivating patients that their efforts associated with lifestyle changes and therapy adherence translate into specific health effects [43].
Beyond primary and secondary prevention, primordial prevention (preventing the initial development of risk factors) and tertiary prevention (reducing disability and the recurrence of events) are also vital. Encouraging healthy behaviours from childhood through community education and public policy can lead to significant long-term benefits [44]. Likewise, incorporating intensive lifestyle management into rehabilitation programmes for post-myocardial infarction or stroke significantly reduces the occurrence of recurrent cardiovascular events [45].
Take-home message and conclusions
Despite significant advances [2], several challenges remain. Optimal dietary recommendations, such as Mediterranean, DASH, or Planetary Health Diets, must accommodate local cultural and socioeconomic factors that influence adherence. In many countries, we also need to advocate for systemic healthcare changes and the regulation of the dietitian profession. Additionally, analyses that focus on one component of the diet at a single timepoint and/or short-term study endpoints complicate the assessment of long-term atherosclerosis progression [46, 47]. Current clinical guidelines still inadequately incorporate emerging risk factors such as sleep, stress, alcohol, and issues of compliance, persistence, and nonadherence. Implementation science should now prioritise integrating these expanded risk assessments into routine clinical practice, ensuring that digital health tools remain accessible to mitigate health inequities. In conclusion, cardiovascular prevention must transition from a linear, risk-factor checklist to an integrated, dynamic model. A comprehensive, 360-degree approach within the suggested the ILEP Simple Tips for the Healthy Heart (ILEP-SMILE) incorporates not only traditional factors (diet, exercise, smoking cessation) but also sleep hygiene, stress management, alcohol moderation, lifelong risk assessment, and extensive education of patients. Only by embracing this holistic framework can we substantially mitigate the global cardiovascular disease burden more effectively and, in the consequence, effectively fight with this largest worldwide killer.



