Introduction
Chronic low back pain (CLBP) is defined as low back pain lasting more than 12 weeks, affecting more than 50% of the general population. It is estimated that more than 70% of the population experience at least one episode of lower lumbar pain, in a certain moment of life. Prevalence is higher among young people, being the second cause of absence from the workplace and one of the main reasons for consulting a doctor. Back pain typically occurs between the ages of 30 and 50, due to the ageing processes but also secondary to a sedentary lifestyle. Approximately 10–40% of low back pain complaints are chronic, of which 85% are nonspecific [1].
Data from the European Health surveys show a wide variation in the prevalence of self-reported low back pain. This ranges from less than 12% of respondents reporting ever having doctor-diagnosed low back pain in France to nearly 33% in Austria reporting ever having had this condition. Among the European countries, the highest proportion of people reporting ever having had low back pain (including not diagnosed by a doctor) is in Slovenia (40.7%) [2]. In Romania the prevalence of low back pain in adults is high (62%), second only to headaches (79%) in the ranking of painful disorders [3].
This condition may negatively impact the patient’s quality of life, and may influence activity for long periods of time, leading to absenteeism in the workplace. Apart from pain and disability the patients can present depression, due to chronic pain, and increased prescription drugs consumption [4]. Patients with chronic pain are more likely to develop depression and even higher levels of pain and worse health-related quality of life [5–12].
Increased attention has recently been given to the concept of pain catastrophizing, often encountered in patients with chronic conditions. This term was introduced to describe an inappropriately cognitive style used by patients with anxiety and depressive disorders. Catastrophic thinking with regard to pain involves a set of exaggerated and negative cognitive and emotional feelings related to actual or anticipated painful stimulation [13]. Some patients define catastrophizing as a tendency to magnify or exaggerate the value or seriousness of pain sensations, while others emphasized pain-related worry and fear, associated with the inability to divert the attention away from pain [14]. According to Sullivan et al., the catastrophic thinking incorporates magnification of pain-related symptoms, rumination about pain, helplessness, and pessimism about the underlying disease [15]. Previous studies demonstrated the association of catastrophizing and sensitization with increased clinical pain among patients with chronic low back pain and myofascial pain [16–18]. Central sensitization seems to mediate the relation between psychological factors (anxiety, depression, catastrophic thinking) and pain intensity [19, 20].
In this study, we aimed to assess the relationship between pain intensity, the components of catastrophizing, depression and disability in patients with chronic low back pain.
Material and methods
Subjects
A total of 100 consecutive patients who were seeking help for their low back pain in a rehabilitation medicine clinic in the period from December 2018 to February 2019 were selected.
Inclusion criteria were chronic low back pain, defined as pain in the back, located between the last rib and the gluteal fold, with mechanical characteristics lasting more than 3 months. Subjects with sciatica, history of back surgery, spinal tumor, spinal fracture, spinal stenosis or radiculopathy, fibromyalgia, inflammatory and infectious spinal diseases were excluded. Chronic pain relief drug users were also excluded from this study.
This study conformed to the principles outlined in the Helsinki Declaration and was approved by the local Ethics Committee (approval no. 198/2018). Participation in the study was voluntary. All subjects who met the inclusion criteria read and signed the informed consent.
Assessment
Participants’ socio-demographic data were collected – age, gender, height, weight, and work status (employed or retired). The main anthropometric parameters measured were weight, height and body mass index of the participants. All participants were asked to complete the Pain Catastrophizing Scale (PCS), the visual analogue scale (VAS), the Oswestry Disability Questionnaire (ODQ), and the Beck Depression Inventory (BDI).
The PCS was used to measure the degree of catastrophic thinking about pain. The scale has 13 items and three dimensions of pain catastrophizing: rumination, magnification, and helplessness. All items are scored through a 5-point Likert scale ranging from 0 (not at all) to 4 (all the time), relating to the past painful experience. Separate subscores for the three dimensions can be calculated. For example, rumination is the sum of items 8, 9, 10 and 11; magnification is the sum of items 6, 7 and 13; and helplessness is the sum of items 1, 2, 3, 4, 5 and 12. A total score ranging from 0 to 52 points can be calculated for the PCS. Higher scores denote a higher degree of catastrophizing. Patients were categorized as high or low catastrophizers based on a median split of PCS scores [15].
Pain intensity was self-completed by each patient on a single-item scale (Visual Analog Scale). This scale is most commonly anchored by “no pain” (score of 0) and “pain as bad as it could be” or “worst imaginable pain” (score of 10). Respondents were asked to report “current” pain intensity or pain intensity “in the last 24 hours”.
The ODQ scale was used to measure the limitation in everyday life activities. It is based on 10 sections with six levels each, assessing the limitation of various activities of daily living [21, 22]. The values range from 0 (the best health state) to 100 (the worst health state). For each section of the questionnaire, the total possible score is 5. The first statement was scored 0, and consecutive statements were scored from 1 to 5. The total score was then divided by the total possible score and expressed as a percentage to produce the Oswestry Disability Index (ODI). The ODI is interpreted as follows: 0–20%, minimal disability; 21–40%, moderate disability; 41–60%, severe disability; 61–80%, crippled; 81–100%, patients are either bed-bound or exaggerate their symptoms [21, 22].
The Beck Depression Inventory (BDI) is a 21-item, self-report rating inventory that measures the intensity of depression [23]. Each question had a set of four possible responses, ranging in intensity, and a score of 0 to 3 is assigned for each answer. The sum of the 21 scored questions gives the total score. A score of 0 to 9 indicates minimal depression; 10 to 18 indicates mild depression; 19 to 29 indicates moderate depression; 30 to 63 indicates severe depression. Higher total scores indicate more severe depressive symptoms.
Statistical analysis
The statistical analysis was performed using MedCalc Statistical Software version 19 (MedCalc Software bvba, Ostend, Belgium). All data were tested for normality with Shapiro-Wilk’s test. Descriptive statistics were calculated for patients’ characteristics (mean and standard deviations) and for VAS, PCS, ODI and BDI (median and interquartile range). Correlation (Spearman’s rank correlation coefficient) and multivariate linear regression with a stepwise procedure were conducted to examine the relationship between ODI and the other variables (gender, age, BMI, work status, pain intensity (VAS), rumination, magnification, helplessness and BDI). The criterion for entry into the regression model was p < 0.05 and for removal from the regression was p > 0.1. The significance level was set at p < 0.05 for all tests.
In order to calculate the required sample size for a multiple regression analysis, the G*Power 3.1 software was used. Using up to 8 variables in the regression analysis, at a large effect size 0f 0.35, at an alpha level of 0.05 and a power of 0.8, a minimum sample of 52 participants was required [24].
Results
Of the 100 patients recruited for this study, only 76 (aged ranged 25–77 years; 73.7% female) agreed to participate, signed the informed consent and answered the questionnaires. Table I outlines the patients’ socio-demographic data.
Table I
Patients socio-demographic data
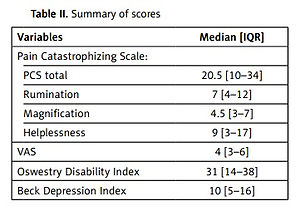
The responses of the VAS, PCS scores, ODI and BDI are presented in Table II. None of the variables showed a normal distribution. The mean group scores revealed moderate CLBP complaints (VAS – 4 [3–6]), mild depression (BDI – 10 [5–16]), a moderate level of catastrophizing (PCS total score 20.5 [10–34]) and moderate disability (ODI – 31 [14–38]). The majority of the patients (55.26%) were low catastrophizers (PCS total < 24), with a VAS of 4 [2–4], a BDI of 7 [2–11] and an ODI of 18 [12–28]. The high catastrophizers (44.74%) had significantly higher scores (VAS – 7 [5–7]), BDI – 16 [11–30] and ODI – 38 [34–52]). Twenty-four patients (31.58%) were scored as having minimal disability, 36 patients (47.37%) moderate disability, and 16 patients (21.05%) severe disability.
Table II
Summary of scores
There were positive weak significant correlations between socio-demographic data (age, residence, work status) and pain, PCS subscales, depression and disability. Positive significant correlations were found between ODI and age, residence, work status, VAS, PCS total, PCS-rumination, PCS-magnification, PCS-helplessness and BDI, and also between PCS total score, PCS subscales and VAS (Table III).
Table III
Correlation among measured variables
| Sex | Age | Residence | Work status | BMI | VAS | ODI | PCS total | PCS-R | PCS-M | PCS-H | BDI | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sex | ||||||||||||
| Age | 0.30* | |||||||||||
| Residence | –0.19 | –0.06 | ||||||||||
| Work status | 0.22 | 0.80* | 0.15 | |||||||||
| BMI | 0.03 | 0.05 | 0.05 | 0.02 | ||||||||
| VAS | 0.08 | 0.29* | 0.30* | 0.46* | –0.15 | |||||||
| ODI | 0.15 | 0.63* | 0.31* | 0.61* | 0.10 | 0.72* | ||||||
| PCS total | 0.11 | 0.56* | 0.32* | 0.57* | 0.06 | 0.75* | 0.85* | |||||
| PCS-R | 0.08 | 0.44* | 0.30* | 0.48* | 0.07 | 0.67* | 0.74* | 0.94* | ||||
| PCS-M | 0.0 | 0.48* | 0.29* | 0.51* | 0.06 | 0.71* | 0.80* | 0.95* | 0.91* | |||
| PCS-H | 0.18 | 0.58* | 0.28* | 0.56* | 0.10* | 0.74* | 0.87* | 0.96* | 0.85* | 0.88* | ||
| BDI | 0.06 | 0.44* | 0.26* | 0.47* | 0.08 | 0.66* | 0.77* | 0.76* | 0.69* | 0.74* | 0.75* |
A multivariate linear regression with a stepwise procedure was conducted to examine the relationship between ODI and the other variables. Only those variables that were significant in the correlation analysis were entered into the regression. A significant model emerged (F(4.71) = 101.38, p < 0.0001), explaining 84% of the variance of disability (R2 = 0.851, adjusted R2 = 0.843). Age, VAS, PCS-helplessness and BDI contributed significantly in this model. The excluded variables from this regression model were residence, work status, PCS-rumination and PCS-magnification. The regression coefficients of the predictors are shown in Table IV.
Discussion
This study investigated whether socio-demographic data, catastrophizing, pain intensity and depression would predict disability in patients with chronic low back pain. In our regression model, age, pain intensity, helplessness and depression explained the variance of disability in patients with nonspecific CLBP.
Socio-demographic (e.g. age, sex, work status, BMI), pain characteristics (intensity, duration, localization, causes) and psychological factors (fear-avoidance beliefs, catastrophizing, anxiety, depression) are reported as predictors of disability not only in patients with chronic pain, but also in patients with CLBP [25–29].
Our results showed that age, residence and work status were significantly correlated with the disability, but only age contributed significantly in the prediction of disability in CLBP patients, similar to previous studies [30–32].
Consistent with previous research, we found that pain intensity was correlated with disability and was one of the independent variables which significantly influenced the disability in our CLBP patients. Significant correlations between CLBP intensity and disability have also been reported in the literature [33–36]. Pain intensity was proved to be a strong predictor of disability in populations with non-specific low back pain in previous studies [37–39].
Catastrophizing has been defined as exaggerated negative emotions regarding pain experience and stimuli [15, 40]. It was reported that catastrophizing could predict pain intensity, disability and psychological distress, and that it has a detrimental effect on general health perception, functional status, medical consumption and quality of life [41–43]. There are a lot of studies in the literature regarding the role of pain catastrophizing in the prognosis and disability of patients with low back pain. Catastrophizing was strongly correlated with disability and the impact on daily living in populations with low back pain [33, 34, 38, 44, 45]. In contrast, there are contradicting studies which report that catastrophizing does not explain the unique variance in disability when assessed alongside factors such as pain-related fear or coping styles [35, 46, 47].
Our study revealed that helplessness was the only component of catastrophizing that significantly predicted disability in patients with NCLBP. One explanation for this situation could be the strong correlations observed between the three PCS subscales. It is possible for some patients to identify so much with pain and to pay more attention to it so that they develop in time helplessness phenomena and implicitly pain-related disability. Similar results were reported by Rosenstiel and Keefe, who found that helplessness (assessed with the Coping Strategy Questionnaire) was associated with greater disability [48]. Sullivan et al. found that helplessness was the strongest predictor of pain-related disability in the group of patients off work for more than 4 years [49]. In the same study they observed that for patients who had been off work for 2–4 years rumination was the only component that predicted disability. Vienneau et al. observed in their study that helplessness was the best predictor of disability in patients with CLBP [50]. Our results are not in accordance with other studies. Sullivan et al. reported that rumination was the component of catastrophizing that was strongly associated with disability in patients with soft-tissue injuries [51]. Ogunlana et al. found that the magnification and rumination components of pain catastrophizing explained 22.6% of the variance of disability in patients with NLBP [34].
It is known that depression is the most frequent emotional condition in individuals with chronic pain or chronic conditions [52, 53]. In our study the correlation between disability and depression was positive and significant, suggesting that the greater the disability related to chronic back pain is, the greater is the possibility of depression-related symptoms. Depression contributed significantly in our model for predicting CLBP-related disability. It is common for depressed patients to avoid activities they used to do, such as housework, sports, social interaction, etc., which leads to disability-related symptoms. Our findings are in accordance with previous research. Hung et al. reported that depression was the most powerful factor associated with disability in their studied populations with CLBP [54].
Another interesting study focused on mechanisms that might be involved in the development of depression and disability. The authors suggest that a potential mechanism is the individual’s health locus of control (HLoC). In psychology, health locus of control refers to people’s beliefs that they have control over different events in their lives (internal locus of control) or that their own actions are a result of external factors beyond their control (external locus of control). The primary outcome of this study is that peoples with low control over their health (internal HLoC) report high levels of depression resulting from pain and pain interference, but moderate levels of disability [55].
There are a number of limitations of our study that should be considered. We did not take into account the stage of chronicity of low back pain or the use of medication. We also did not evaluate the fear avoidance beliefs and the coping strategies that could interfere with catastrophizing and depression in our study sample.
Our findings can contribute to a better understanding of the predictive factors of disability in patients with CLBP, such as age, pain intensity, catastrophizing pain and depression. The need to assess the abovementioned variables is an essential element in the complex approach of the patient with CLBP. Moreover, the knowledge of these factors can provide support for health professionals to choose more effective therapeutic approaches.