Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
PUBLIC HEALTH / RESEARCH PAPER
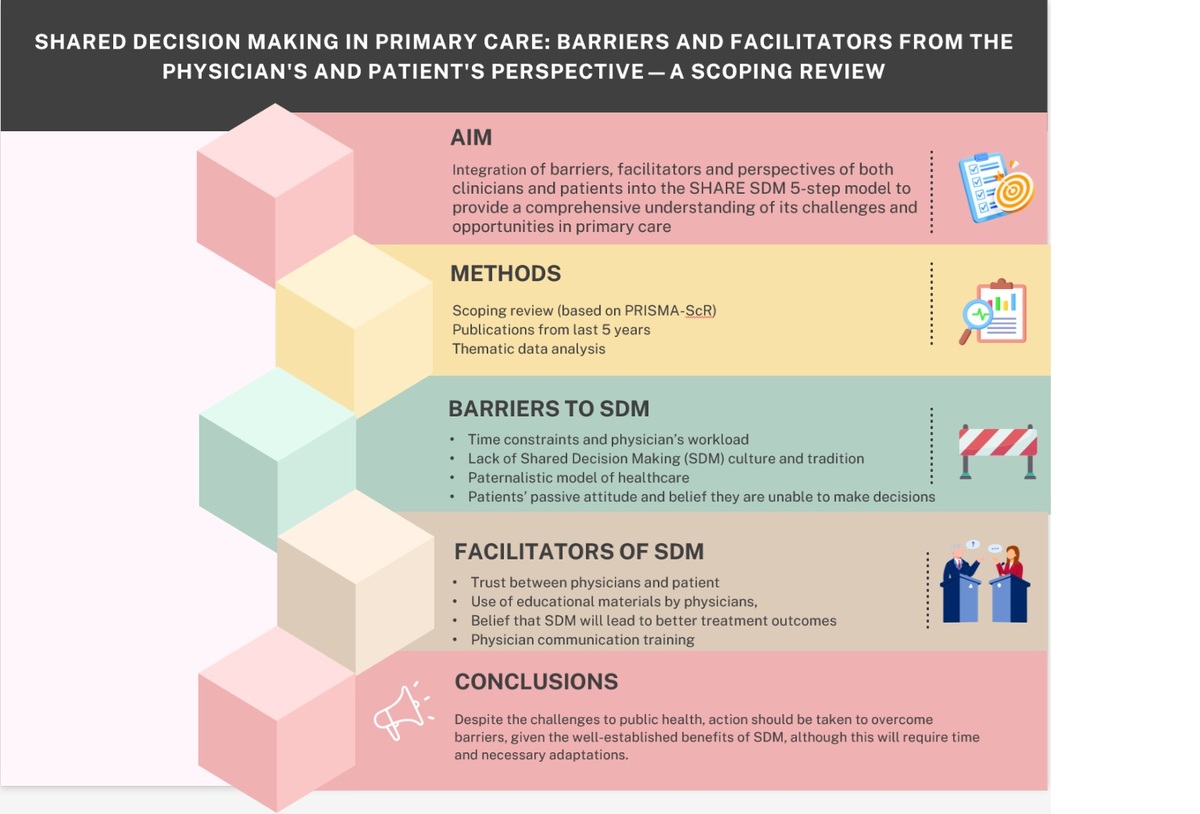
Shared Decision Making in primary care: barriers and facilitators from the physician's and patient's perspective—a scoping review.
1
Narodowy Instytut Zdrowia Publicznego Państwowy Zakład Higieny - Państwowy Instytut Badawczy, Poland
Submission date: 2024-10-29
Final revision date: 2025-06-11
Acceptance date: 2025-07-16
Online publication date: 2025-08-23
Corresponding author
Magdalena Krysińska-Pisarek
Narodowy Instytut Zdrowia Publicznego Państwowy Zakład Higieny - Państwowy Instytut Badawczy, Poland
Narodowy Instytut Zdrowia Publicznego Państwowy Zakład Higieny - Państwowy Instytut Badawczy, Poland
KEYWORDS
TOPICS
ABSTRACT
Introduction:
Health-related communication and Shared Decision Making (SDM) are crucial elements of patient-centered care. Multiple studies have showed that the decision-making process is often far from ideal, where an ideal process involves the patient being active, understanding their treatment options, and expressing preferences clearly, while the physician has sufficient time and willingness to share knowledge and involve the patient in the decision-making process. The aim of this review was to identify the key barriers and facilitators influencing the adoption of Shared Decision Making (SDM) approach from both the physician’s and patient’s perspectives in primary healthcare in relation to the 5-step model of SDM.
Material and methods:
A scoping review of resources published within the last five years was conducted in June 2024 on the basis of PRISMA-ScR. Specific barriers hindering the adoption of SDM were identified, which can arise at any of the five steps.
Results:
The most common barriers include: time constraints and physician’s workload, lack of SDM culture and tradition, paternalistic model of healthcare, patients’ passive attitude and belief they are unable to make decisions. SDM facilitators include: trust, use of educational materials by physicians, belief that SDM will lead to better treatment outcomes, and training in communication for physicians.
Conclusions:
Despite the challenges to public health, action should be taken to overcome these barriers, given the well-established benefits of SDM, although this will require time and necessary adaptations.
Health-related communication and Shared Decision Making (SDM) are crucial elements of patient-centered care. Multiple studies have showed that the decision-making process is often far from ideal, where an ideal process involves the patient being active, understanding their treatment options, and expressing preferences clearly, while the physician has sufficient time and willingness to share knowledge and involve the patient in the decision-making process. The aim of this review was to identify the key barriers and facilitators influencing the adoption of Shared Decision Making (SDM) approach from both the physician’s and patient’s perspectives in primary healthcare in relation to the 5-step model of SDM.
Material and methods:
A scoping review of resources published within the last five years was conducted in June 2024 on the basis of PRISMA-ScR. Specific barriers hindering the adoption of SDM were identified, which can arise at any of the five steps.
Results:
The most common barriers include: time constraints and physician’s workload, lack of SDM culture and tradition, paternalistic model of healthcare, patients’ passive attitude and belief they are unable to make decisions. SDM facilitators include: trust, use of educational materials by physicians, belief that SDM will lead to better treatment outcomes, and training in communication for physicians.
Conclusions:
Despite the challenges to public health, action should be taken to overcome these barriers, given the well-established benefits of SDM, although this will require time and necessary adaptations.
REFERENCES (60)
1.
Ratna H. The importance of effective communication in healthcare practice. Harvard Public Health Review. 2019;23.DOI:10.54111/0001/W4.
2.
Siebinga VY, Driever EM, Stiggelbout AM, Brand PLP. Shared decision making, patient-centered communication and patient satisfaction - A cross-sectional analysis. Patient Educ Couns. 2022;105(7):2145-2150. doi: 10.1016/j.pec.2022.03.012.
3.
Expósito-Jiménez A, Alcaide-Leyva JM, Jiménez-Mérida MdR, Martínez-Angulo P. Health communication and shared decision-making between nurses and older adults in community setting: An integrative review. Journal of Clinical Nursing. 2024;33: 2922–2935. https://doi.org/10.1111/jocn.1....
4.
US Preventive Services Task Force. Collaboration and Shared Decision-Making Between Patients and Clinicians in Preventive Health Care Decisions and US Preventive Services Task Force Recommendations. JAMA. 2022;327(12),1171–1176. doi:10.1001/jama.2022.3267.
5.
President’s Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research. Making health care decisions. The ethical and legal implications of informed consent in the patient— practitioner relationship. Washington DC 1982: https://repository.library.geo....
6.
Ankolekar A, Dekker A, Fijten R, Berlanga A. The Benefits and Challenges of Using Patient Decision Aids to Support Shared Decision Making in Health Care. JCO Clin Cancer Inform. 2018; 2:1-10. doi: 10.1200/CCI.18.00013.
7.
Agency for Healthcare Research and Quality (AHRQ). The SHARE Approach. 2018; https://www.ahrq.gov/health-li....
8.
Hargraves IG, Fournier AK, Montori VM, Bierman AS. Generalized shared decision making approaches and patient problems. Adapting AHRQ's SHARE Approach for Purposeful SDM. Patient Educ Couns. 2020;103(10):2192-2199. doi: 10.1016/j.pec.2020.
9.
Ng CJ, Lee PY. Practising shared decision making in primary care. Malays Fam Physician. 2021; 22;16(1), 2-7. doi: 10.51866/cm0001.
10.
Buljac-Samardzic M, Clark MA, van Exel NJA, van Wijngaarden JDH. Patients as team members: factors affecting involvement in treatment decisions from the perspective of patients with a chronic condition. Health Expect. 2022; 25; 138-148. https://doi.org/10.1111/hex.13....
11.
Faiman B, Tariman J. Shared Decision Making: Improving Patient Outcomes by Understanding the Benefits of and Barriers to Effective Communication. Clinical journal of oncology nursing. 2019; 23: 540-542. 10.1188/19.CJON.540-542.
12.
van der Horst DEM, Hofstra N, van Uden-Kraan CF, Stiggelbout AM et al. Shared Decision Making in Health Care Visits for CKD: Patients’ Decisional Role Preferences and Experiences. AJKD. 2023; 20: doi: 10.1053/j.ajkd.2023.04.012.
13.
Matthias MS, Talib TL, Huffman MA. Managing chronic pain in an opioid crisis: what is the role of shared decision-making? Health Commun 2020; 1-9.
14.
Anagnostou A, Hourihane JOB, Greenhawt M. The role of shared decision making in pediatric food allergy management. J Allergy Clin Immunol Pract. 2020; 8: 46-51. 10.1016/j.jaip.2019.09.004.
15.
Sobczak K, Leoniuk K. Doctors’ attitudes in the situation of delivering bad news: patients’ experience and expectations. Archives of Medical Science. 2023;19(4):921-929. doi:10.5114/aoms/112756.
16.
Hoque F. Shared Decision Making: Pinnacle for Patient-Clinician Relationships. Journal of BMANA. 2023; 2(1): 1-4.
17.
Wieringa TH, Rodriguez-Gutierrez R, Spencer-Bonilla G, de Wit M, Ponce OJ, Sanchez-Herrera MF, Espinoza NR, Zisman-Ilani Y, Kunneman M, Schoonmade LJ, Montori VM, Snoek FJ. Decision aids that facilitate elements of shared decision making in chronic illnesses: a systematic review. Syst Rev. 2019;8,121. https://doi.org/10.1186/s13643....
18.
Berger Z. Navigating the unknown: shared decision-making in the face of uncertainty. J Gen Intern Med. 2015, 15; 359:675-8.
19.
Joseph‐Williams N, Lloyd A, Edwards A, et al. Implementing shared decision making in the NHS: lessons from the MAGIC programme. BMJ 2017; 357, j1744. 10.1136/bmj.j1744.
20.
Montori VM, Ruissen MM, Hargraves IG, Brito JP, Kunneman M. Shared decision-making as a method of care. BMJ Evid Based Med. 2023; 28(4): 213-217. doi: 10.1136/bmjebm-2022-112068.
21.
Moleman M, Regeer BJ, Schuitmaker-Warnaar TJ. Shared decision-making and the nuances of clinical work: Concepts, barriers and opportunities for a dynamic model. J Eval Clin Pract. 2021;27: 926–934. https://doi.org/10.1111/jep.13....
22.
Makoul G, Clayman ML. An integrative model of shared decision making in medical encounter. Patient Educ. Couns. 2006; 60(3):301-312.
23.
Harzheim L, Lorke M, Schulz S, Jünger S. Health literacy and shared decision-making in predictive medicine — professionals’ perceptions and communication strategies. J Public Health (Berl.). 2023: https://doi.org/10.1007/s10389....
24.
Schoefs E, Vermeire S, Janssens R, Huys I. HSD68 Barriers and Facilitators of Shared Decision Making in Clinical Practice: An Umbrella Review. Value in Health. 2022; 25(12): 287. https://doi.org/10.1016/j.jval..., 2021;.
25.
National Institute for Health and Care Excellence (NICE). (2021). Evidence review for effectiveness of approaches and activities to increase engagement in shared decision making and the barriers and facilitators to engagement: Shared decision making: Evidence Review. (NICE Guideline, No. 197.) https://www.ncbi.nlm.nih.gov/b....
26.
Eales OO, Smith S. Do socio-economically disadvantaged patients prefer shared decision-making? S Afr Fam Pract. 2021;17;63(1), e1-e6. doi: 10.4102/safp.v63i1.5293.
27.
Caverly TJ, Hayward RA. Dealing with the Lack of Time for Detailed Shared Decision-making in Primary Care: Everyday Shared Decision-making. J Gen Intern Med. 2020 Oct;35(10):3045-3049.
28.
Tan NQP, Maki KG, López-Olivo MA, Geng Y, Volk RJ. Cultural influences on shared decision-making among Asian Americans: A systematic review and meta-synthesis of qualitative studies. Patient Educ Couns. 2023;106:17-30. doi: 10.1016/j.pec.2022.10.350.
29.
Creaney R. What Works to Support and Promote Shared Decision Making: A synthesis of recent evidence. Scottish Government 2019. https://www.gov.scot/binaries/... (accessed on 7 Jun 2024).
30.
Grad R, Sandhu A, Majdpour D, Kitner S, Rodriguez C, Elwyn G. Perspectives of family physician educators on shared decision making in preventive health care: A Qualitative Descriptive Inquiry. Patient Education and Counseling. 2025; 134: 108681.
31.
Yahanda AT, Mozersky J. What's the Role of Time in Shared Decision Making? AMA J Ethics. 2020 May 1;22(5):E416-422. doi: 10.1001/amajethics.2020.416.
32.
Hu Q, Feng Z, Zong Q, Wang J, Zheng Z, Feng D. Analysis of factors that promote the participation of patients with chronic diseases in shared decision making on medication: a cross-sectional survey in Hubei Province, China. BMC Public Health 2023; 23, 2440. https://doi.org/10.1186/s12889....
33.
Bartels EA, Meijboom BR, Nahar-van Venrooij LMW, de Vries E. How service modularity can provide the flexibility to support person-centered care and shared decision-making. BMC Health Serv Res, 2021;18;21(1),1245. doi: 10.1186/s12913-021-07267-6. Erratum in: BMC Health Serv Res. 2022, 23;22(1),815.
34.
Alsulamy N, Lee A, Thokala P, Alessa T. Views of stakeholders on factors influencing shared decision-making in the Eastern Mediterranean Region: a systematic review. East Mediterr Health J. 2021; 23;27(3),300-311. doi: 10.26719/emhj.20.139.
35.
Tang C, Wang A, Yan J. Exploring motivations and resistances for implementing shared decision-making in clinical practice: a systematic review based on a structure–process–outcome model. Health Expect. 2022; 25: 1254-1268. doi:10.1111/hex.13541.
36.
Li X, Yang D, Meng M, Zhao J, Yin Y, Wang H, Zhang X, Liu Q, Li M, Liu J, Hao Y. Shared decision-making in healthcare in mainland China: a scoping review. Front Public Health. 2023; 7(11): 1162993. doi: 10.3389/fpubh.2023.1162993.
37.
Légaré F, Härter M, Stiggelbout AM, Thomson R, Stacey D, North J.(2020). Choosing treatments and the role of shared decision-making. In: E. Nolte, S. Merkur, A. Anell, (Ed.). Achieving Person-Centred Health Systems: Evidence, Strategies and Challenges European Observatory on Health Systems and Policies. Cambridge University Press 2020; p. 283-316.
38.
Caverly TJ, Hayward RA. Dealing with the Lack of Time for Detailed Shared Decision-making in Primary Care: Everyday Shared Decision-making. J Gen Intern Med. 2020; 35(10),3045-3049. doi: 10.1007/s11606-020-06043-2.
39.
Ousseine YM, Durand MA, Bouhnik AD, Smith A, Mancini J. Multiple health literacy dimensions are associated with physicians' efforts to achieve shared decision-making. Patient Educ Couns. 2019;102(11):1949-1956. doi: 10.1016/j.pec.2019.05.015.
40.
Goto Y, Miura H, Son D, Scholl I, Kriston L, Härter M, Sato K, Kusaba T, Arai H. Association between physicians' and patients' perspectives of shared decision making in primary care settings in Japan: The impact of environmental factors. PLoS One. 2021;10;16(2), e0246518. doi: 10.1371/journal.pone.0246518.
41.
Hawley ST, Morris AM. Cultural challenges to engaging patients in shared decision making. Patient Educ Couns. 2017;100(1),18-24. doi: 10.1016/j.pec.2016.07.008.
42.
Fisher KA, Tan ASL, Matlock DD, Saver B, Mazor KM, Pieterse AH. Keeping the patient in the center: Common challenges in the practice of shared decision making. Patient Educ Couns.2018; 101(12): 2195-2201. doi: 10.1016/j.pec.2018.08.007.
43.
Keij SM, de Boer JE, Stiggelbout AM, Bruine de Bruin W, Peters E, Moaddine S, Kunneman M, Pieterse AH. How are patient-related characteristics associated with shared decision-making about treatment? A scoping review of quantitative studies. BMJ Open. 2022; 24,12(5), e057293. doi: 10.1136/bmjopen-2021-057293.
44.
Büdenbender B, Köther AK, Grüne B, Michel MS, Kriegmair MC, Alpers GW. When attitudes and beliefs get in the way of shared decision-making: A mediation analysis of participation preference. Health Expect. 2023; 26(2):740-751. doi: 10.1111/hex.13699.
45.
Ajzen I, Schmidt P. Changing behavior using the theory of planned behavior. In: MS Hagger, LD Cameron, K Hamilton, N Hankonen, & T Lintunen, (Ed). The Handbook of Behavior Change. Cambridge University Press, 2020, p.17-31.
46.
Alsulamy N, Lee AP, Thokala P, Alessa T. What Influences the Implementation of Shared Decision Making: An Umbrella Review. Patient Education and Counseling. 2020; 103(12):2400-7. https://doi.org/10.1016/j.pec.....
47.
Roodbeen R, Vreke A, Boland G, Rademakers J, van den Muijsenbergh M, Noordman J, van Dulmen S. Communication and shared decision-making with patients with limited health literacy; helpful strategies, barriers and suggestions for improvement reported by hospital-based palliative care providers. PLoS One. 2020;15(6), e0234926. doi: 10.1371/journal.pone.0234926.
48.
Muscat DM, Shepherd HL, Nutbeam D, Trevena L, McCaffery KJ. Health Literacy and Shared Decision-making: Exploring the Relationship to Enable Meaningful Patient Engagement in Healthcare. J Gen Intern Med. 2021; 36(2): 521-524. doi: 10.1007/s11606-020-05912-0.
49.
Stacey D, Légaré F, Lewis K, Barry MJ, Bennett CL, Eden KB, Holmes-Rovner M, Llewellyn-Thomas H, Lyddiatt A, Thomson R, Trevena L. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst.Rev , 4, CD001431.
50.
Visscher BB, Steunenberg B, Heijmans M, Hofstede JM, Deville W, van der Heide I, Rademakers J. Evidence on the effectiveness of health literacy interventions in the EU: a systematic review. BMC Public Health. 2018; 18(1).
51.
Tringale M, Stephen G, Boylan AM, Heneghan C. Integrating patient values and preferences in healthcare: a systematic review of qualitative evidence. BMJ Open. 2022 18;12(11), e067268. doi: 10.1136/bmjopen-2022-067268.
52.
Bialosky JE, Cleland JA, Mintken P, Beneciuk JM, Bishop MD.The healthcare buffet: preferences in the clinical decision-making process for patients with musculoskeletal pain. J Man Manip Ther. 2022; 30(2),68-77. doi: 10.1080/10669817.2021.1989754.
53.
Thériault G, Grad R, Dickinson JA, Breault P, Singh H, Bell NR, Szafran O. To share or not to share: When is shared decision making the best option? Can Fam Physician. 2020; 66(5), 327-331.
54.
Coulter A. Partnerships with patients: the pros and cons of shared clinical decision-making. J Health Serv Res Policy. 1997; 2(2): 112-21. doi: 10.1177/135581969700200209.
55.
Cox CL. Patient understanding: how should it be defined and assessed in clinical practice? J Eval Clin Pract. 2023; 29: 1127-1134. doi:10.1111/jep.13882.
56.
Barstow C, Shahan B, Roberts M. Evaluating Medical Decision-Making Capacity in Practice. Am Fam Physician, 2018; 1,98(1):40-46.
57.
Verwijmeren D, Grootens KP. Shifting Perspectives on the Challenges of Shared Decision Making in Mental Health Care. Community Ment Health J. 2024; 60:292–307. https://doi.org/10.1007/s10597....
58.
Laight D. Risk communication: a pillar of shared decision making. Prescriber 2022; 33: 24-28. https://doi.org/10.1002/psb.19....
59.
Elwyn G, Price A, Franco JVA, Gulbrandsen P. The limits of shared decision making. BMJ Evid Based Med. 2023; 28(4): 218-221. doi: 10.1136/bmjebm-2022-112089.
60.
Scholl I, LaRussa A, Hahlweg P, Kobrin S, Elwyn G. Organizational- and system-level characteristics that influence implementation of shared decision-making and strategies to address them - a scoping review. Implement Sci. 2018 Mar 9;13(1):40. doi: 10.1186/s13012-018-0731-z.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.