Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
EXPERIMENTAL RESEARCH
Slc6a4 silencing alleviates ropivacaine-induced injury in myocardial infarction cell models
1
Department of Anesthesiology, The Central Hospital of Wuhan, Tongji Medical College, Huazhong University of Science and Technology, Wuhan City, Hubei Province, China
These authors had equal contribution to this work
Submission date: 2024-11-07
Final revision date: 2025-09-04
Acceptance date: 2025-10-09
Online publication date: 2026-01-20
Corresponding author
Jing Wan
Department of Anesthesiology The Central Hospital of Wuhan Tongji Medical College Huazhong University of Science and Technology No. 26, Shengli Street Jiang’an District Wuhan City Hubei Province China, 430014
Department of Anesthesiology The Central Hospital of Wuhan Tongji Medical College Huazhong University of Science and Technology No. 26, Shengli Street Jiang’an District Wuhan City Hubei Province China, 430014
Shenghua Li
Department of Anesthesiology The Central Hospital of Wuhan Tongji Medical College Huazhong University of Science and Technology No. 26, Shengli Street Jiang’an District Wuhan City Hubei Province China, 430014
Department of Anesthesiology The Central Hospital of Wuhan Tongji Medical College Huazhong University of Science and Technology No. 26, Shengli Street Jiang’an District Wuhan City Hubei Province China, 430014
KEYWORDS
TOPICS
ABSTRACT
Introduction:
Myocardial infarction (MI), often caused by atherosclerotic plaque rupture, leads to severe myocardial ischemia and necrosis. Despite advancements in treatment, its molecular mechanisms remain incompletely understood. Local anesthetics such as ropivacaine, while beneficial for pain control, may induce cardiotoxicity, complicating MI management. This study aimed to explore the effects of ropivacaine on H9c2 cardiomyocytes and the protective potential of Slc6a4 silencing against ropivacaine-induced cellular damage.
Material and methods:
Bioinformatics analysis of the GSE97320 dataset identified MI-associated differentially expressed genes (DEGs), which overlapped with ropivacaine-related genes. H9c2 cells were cultured and treated with ropivacaine to induce myocardial injury. The effects on cell cycle, apoptosis, and oxidative stress were assessed, and the role of Slc6a4 silencing under hypoxia/reoxygenation (H/R) conditions was investigated.
Results:
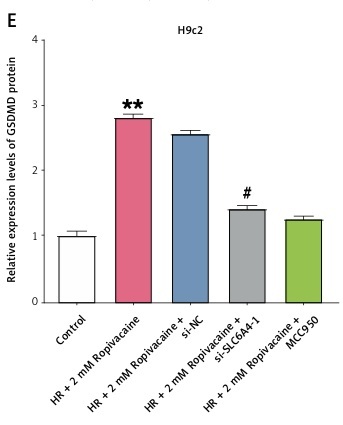
Ropivacaine induced G1 phase arrest and apoptosis in H9c2 cells, with increased Bax and caspase 3 levels and decreased Bcl-2. Oxidative stress was elevated, as evidenced by increased ROS, MDA, and LDH levels and reduced SOD, GSH, and ATP. Slc6a4 silencing under H/R conditions mitigated these effects, reducing cell cycle dysregulation and apoptosis by 40%, lowering NLRP3 inflammasome expression, and promoting Nrf2 nuclear translocation.
Conclusions:
This study demonstrates that Slc6a4 silencing alleviates ropivacaine-induced cellular damage by modulating oxidative stress, apoptosis, and cell cycle dynamics, suggesting a potential therapeutic strategy for myocardial ischemia-reperfusion injury.
Myocardial infarction (MI), often caused by atherosclerotic plaque rupture, leads to severe myocardial ischemia and necrosis. Despite advancements in treatment, its molecular mechanisms remain incompletely understood. Local anesthetics such as ropivacaine, while beneficial for pain control, may induce cardiotoxicity, complicating MI management. This study aimed to explore the effects of ropivacaine on H9c2 cardiomyocytes and the protective potential of Slc6a4 silencing against ropivacaine-induced cellular damage.
Material and methods:
Bioinformatics analysis of the GSE97320 dataset identified MI-associated differentially expressed genes (DEGs), which overlapped with ropivacaine-related genes. H9c2 cells were cultured and treated with ropivacaine to induce myocardial injury. The effects on cell cycle, apoptosis, and oxidative stress were assessed, and the role of Slc6a4 silencing under hypoxia/reoxygenation (H/R) conditions was investigated.
Results:
Ropivacaine induced G1 phase arrest and apoptosis in H9c2 cells, with increased Bax and caspase 3 levels and decreased Bcl-2. Oxidative stress was elevated, as evidenced by increased ROS, MDA, and LDH levels and reduced SOD, GSH, and ATP. Slc6a4 silencing under H/R conditions mitigated these effects, reducing cell cycle dysregulation and apoptosis by 40%, lowering NLRP3 inflammasome expression, and promoting Nrf2 nuclear translocation.
Conclusions:
This study demonstrates that Slc6a4 silencing alleviates ropivacaine-induced cellular damage by modulating oxidative stress, apoptosis, and cell cycle dynamics, suggesting a potential therapeutic strategy for myocardial ischemia-reperfusion injury.
REFERENCES (62)
1.
Upadhyay RK. High cholesterol disorders, myocardial infarction and its therapeutics. World J Cardiovasc Dis 2023; 13: 433-69.
2.
Ambroziak M, Niewczas-Wieprzowska K, Maicka A, Budaj A. Younger age of patients with myocardial infarction is associated with a higher number of relatives with a history of premature atherosclerosis. BMC Cardiovasc Disord 2020; 20: 410.
3.
Libby P, Ridker PM, Hansson GK. Inflammation in atherosclerosis: from pathophysiology to practice. J Am Coll Cardiol 2009; 54: 2129-38.
4.
Messerli FH, Rimoldi SF, Bangalore S. The transition from hypertension to heart failure: contemporary update. JACC Heart Fail 2017; 5: 543-51.
5.
Low Wang CC, Hess CN, Hiatt WR, Goldfine AB. Clinical update: cardiovascular disease in diabetes mellitus: atherosclerotic cardiovascular disease and heart failure in type 2 diabetes mellitus - mechanisms, management, and clinical considerations. Circulation 2016; 133: 2459-502.
6.
Sardu C, Paolisso G, Marfella R. Inflammatory related cardiovascular diseases: from molecular mechanisms to therapeutic targets. Curr Pharm Des 2020; 26: 2565-73.
7.
Sardu C, Massetti M, Testa N, et al. Effects of sodium-glucose transporter 2 inhibitors (SGLT2-I) in patients with ischemic heart disease (IHD) treated by coronary artery bypass grafting via MiECC: inflammatory burden, and clinical outcomes at 5 years of follow-up. Front Pharmacol 2021; 12: 777083.
8.
Sardu C, D’Onofrio N, Torella M, et al. Metformin therapy effects on the expression of sodium-glucose cotransporter 2, leptin, and SIRT6 levels in pericoronary fat excised from pre-diabetic patients with acute myocardial infarction. Biomedicines 2021; 9: 904.
9.
Marfella R, Prattichizzo F, Sardu C, et al. Evidence of an anti-inflammatory effect of PCSK9 inhibitors within the human atherosclerotic plaque. Atherosclerosis 2023; 378: 117180.
10.
Ambrose JA, Barua RS. The pathophysiology of cigarette smoking and cardiovascular disease: an update. J Am Coll Cardiol 2004; 43: 1731-7.
11.
Kumar Singh A, Kumar Jat R. Myocardial infarction. Himalayan J Health Sci 2022; 6: 16-32.
12.
Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Kardiol Pol 2018; 76: 229-313.
13.
Anderson JL, Morrow DA. Acute myocardial infarction. N Engl J Med 2017; 376: 2053-64.
14.
Stevens JR, Zamani A, Osborne JIA, Zamani R, Akrami M. Critical evaluation of stents in coronary angioplasty: a systematic review. Biomed Engineering Online 2021; 20: 46.
15.
Satish S. Advancements in pharmacotherapy for myocardial infarction: a comprehensive review. Int J Pharm Sci 2023; 1: 534.
16.
Jankovic D. Regional nerve block in anesthesia and pain therapy: general consideration. In: Regional Nerve Blocks in Anesthesia and Pain Therapy: Imaging-guided and Traditional Techniques. Jankovic D, Peng P (eds.). Springer International Publishing, Cham 2022; 3-31.
17.
Jin Z, Liu J, Li R, Gan TJ, He Y, Lin J. Single injection Quadratus Lumborum block for postoperative analgesia in adult surgical population: a systematic review and meta-analysis. J Clin Anesth 2020; 62: 109715.
19.
Graf BM, Abraham I, Eberbach N, Kunst G, Stowe DF, Martin E. Differences in cardiotoxicity of bupivacaine and ropivacaine are the result of physicochemical and stereoselective properties. Anesthesiology 2002; 96: 1427-34.
20.
Capdevila X, Pirat P, Bringuier S, et al. Continuous peripheral nerve blocks in hospital wards after orthopedic surgery: a multicenter prospective analysis of the quality of postoperative analgesia and complications in 1,416 patients. Anesthesiology 2005; 103: 1035-45.
21.
Ilfeld BM. Continuous peripheral nerve blocks: a review of the published evidence. Anesth Analg 2011; 113: 904-25.
22.
Martínez-Martínez E, Ibarrola J, Fernández-Celis A, et al. Differential proteomics identifies reticulocalbin-3 as a novel negative mediator of collagen production in human cardiac fibroblasts. Sci Rep 2017; 7: 12192.
23.
Zeng L, Li A, Zhang Z, et al. Ropivacaine induces cell cycle arrest in the G0/G1 phase and apoptosis of PC12 cells via inhibiting mitochondrial STAT3 translocation. Inflammation 2021; 44: 2362-76.
24.
Zhang W, Shi C, Yao Z, Qian S. Bardoxolone methyl attenuates doxorubicin-induced cardiotoxicity by inhibiting the TXNIP-NLRP3 pathway through Nrf2 activation. Environ Toxicol 2024; 39: 1936-50.
25.
Tong R, Jia T, Shi R, Yan F. Inhibition of microRNA-15 protects H9c2 cells against CVB3-induced myocardial injury by targeting NLRX1 to regulate the NLRP3 inflammasome. Cell Mol Biol Lett 2020; 25: 6.
26.
Xia W, Li Y, Wu M, et al. Gasdermin E deficiency attenuates acute kidney injury by inhibiting pyroptosis and inflammation. Cell Death Dis 2021; 12: 139.
27.
Yang X, Chen D, Zheng S, et al. The Prmt5-Vasa module is essential for spermatogenesis in Bombyx mori. PLoS Genet 2023; 19: e1010600.
28.
Valussi M, Besser J, Wystub-Lis K, et al. Repression of Osmr and Fgfr1 by miR-1/133a prevents cardiomyocyte dedifferentiation and cell cycle entry in the adult heart. Sci Adv 2021; 7: eabi6648.
29.
Wang AJ, Tang Y, Zhang J, et al. Cardiac SIRT1 ameliorates doxorubicin-induced cardiotoxicity by targeting sestrin 2. Redox Biol 2022; 52: 102310.
30.
Wang J, Xie SA, Li N, et al. Matrix stiffness exacerbates the proinflammatory responses of vascular smooth muscle cell through the DDR1-DNMT1 mechanotransduction axis. Bioact Mater 2022; 17: 406-24.
31.
Wang L, Liu J, Wang Z, et al. Dexmedetomidine abates myocardial ischemia reperfusion injury through inhibition of pyroptosis via regulation of miR-665/MEF2D/Nrf2 axis. Biomed Pharmacother 2023; 165: 115255.
32.
Li F, Zhu H, Chang Z, Li Y. Gentiopicroside alleviates acute myocardial infarction injury in rats by disrupting Nrf2/NLRP3 signaling. Exp Biol Med 2023; 248: 1254-66.
33.
Zhang YM, Zhang ZY, Wang RX. Protective mechanisms of quercetin against myocardial ischemia reperfusion injury. Front Physiol 2020; 11: 506938.
34.
Lin P, Cao J, Ren P, et al. Network pharmacology and experimental validation to explore mechanism of tetrahydropalmatine on acute myocardial ischemia. Chin J Integr Med 2023; 29: 1087-98.
35.
Coto E, Reguero JR, Alvarez V, et al. 5-Hydroxytryptamine 5-HT2A receptor and 5-hydroxytryptamine transporter polymorphisms in acute myocardial infarction. Clin Sci 2003; 104: 241-5.
36.
Bhatt DL, Lopes RD, Harrington RA. Diagnosis and treatment of acute coronary syndromes: a review. JAMA 2022; 327: 662-75.
37.
Akşit E, Büyük B, Oğuz S. Histopathological changes in myocardial tissue due to coronary venous hypertension. Arch Med Sci 2023; 19: 1714-20.
38.
Awasthi S, Chalapathy CV. BEYOND THE BEATS. A Comprehensive Guide to. LAP LAMBERT Academic Publishing 2023.
39.
Bays HE, Taub PR, Epstein E, et al. Ten things to know about ten cardiovascular disease risk factors. Am J Prev Cardiol 2021; 5: 100149.
40.
Sardu C, Gatta G, Pieretti G, et al. Pre-menopausal breast fat density might predict MACE during 10 years of follow-up: the BRECARD Study. JACC Cardiovasc Imaging 2021; 14: 426-38.
41.
Fishbein GA, Fishbein MC, Wang J, Buja LM. Myocardial ischemia and its complications. In: Cardiovascular Pathology. Buja LM, Butany J (eds.). Elsevier 2022; 407-45.
42.
Moyer AM, Walker DL, Avula R, et al. Relationship of genetic variation in the serotonin transporter gene (SLC6A4) and congenital and acquired cardiovascular diseases. Genet Test Mol Biomarkers 2015; 19: 115-23.
43.
Hartopo AB, Puspitawati I, Gharini PP, Setianto BY. Platelet microparticle number is associated with the extent of myocardial damage in acute myocardial infarction. Arch Med Sci 2016; 12: 529-37.
44.
Malumbres M. Control of the cell cycle. In: Abeloff’s Clinical Oncology. Niederhuber JE, Armitage JO, Doro-show JH, et al. (eds.). Elsevier 2020; 56-73.
45.
Hu XM, Zhang Q, Zhou RX, et al. Programmed cell death in stem cell-based therapy: mechanisms and clinical applications. World J Stem Cells 2021; 13: 386-415.
46.
Luo X, Zhou J, Wang Z, et al. An inhibitor role of Nrf2 in the regulation of myocardial senescence and dysfunction after myocardial infarction. Life Sci 2020; 259: 118199.
47.
Zink W, Bohl JR, Hacke N, Sinner B, Martin E, Graf BM. The long term myotoxic effects of bupivacaine and ropivacaine after continuous peripheral nerve blocks. Anesthesia Analgesia 2005; 101: 548-54.
48.
Zhu Y, Yuan Z, Liu X, Jing G. Effect of metallothionein on myocyte apoptosis and energy supply of isolated rabbit heart muscle during perfusion with ropivacaine. Nan Fang Yi Ke Da Xue Xue Bao 2011; 31: 1425-7.
49.
Zhu G, Zhang L, Dan J, Zhu Q. Differential effects and mechanisms of local anesthetics on esophageal carcinoma cell migration, growth, survival and chemosensitivity. BMC Anesthesiol 2020; 20: 126.
50.
Demirci-Cekic S, Özkan G, Avan AN, Uzunboy S, Çapanoğlu E, Apak R. Biomarkers of oxidative stress and antioxidant defense. J Pharm Biomed Analysis 2022; 209: 114477.
51.
Martemucci G, Costagliola C, Mariano M, D’andrea L, Napolitano P, D’Alessandro AG. Free radical properties, source and targets, antioxidant consumption and health. Oxygen 2022; 2: 48-78.
52.
Jelic MD, Mandic AD, Maricic SM, Srdjenovic BU. Oxidative stress and its role in cancer. J Cancer Res Ther 2021; 17: 22-8.
53.
Saxena P, Selvaraj K, Khare SK, Chaudhary N. Superoxide dismutase as multipotent therapeutic antioxidant enzyme: role in human diseases. Biotechnol Letters 2022; 44: 1-22.
54.
Zhu XA, Gao LF, Zhang ZG, Xiang DK. Down-regulation of miR-320 exerts protective effects on myocardial IR injury via facilitating Nrf2 expression. Eur Rev Med Pharmacol Sci 2019; 23: 1730-41.
55.
Zhang Z, Zhao X, Gao M, et al. Dioscin alleviates myocardial infarction injury via regulating BMP4/NOX1-mediated oxidative stress and inflammation. Phytomedicine 2022; 103: 154222.
56.
Zhang W, Shi C, Yao Z, Qian S. Bardoxolone methyl attenuates doxorubicin‐induced cardiotoxicity by inhibiting the TXNIP–NLRP3 pathway through Nrf2 activation. Environ Toxicol 2024; 39: 1936-50.
57.
Zhang Q, Wang L, Wang S, et al. Signaling pathways and targeted therapy for myocardial infarction. Signal Transd Targeted Ther 2022; 7: 78.
58.
Fan ZX, Yang CJ, Li YH, Yang J, Huang CX. Ginsenoside Rh2 attenuates myocardial ischaemia reperfusion injury by regulating the Nrf2/HO 1/NLRP3 signalling pathway. Exp Ther Med 2023; 25: 35.
59.
Marfella R, Sardu C, D’Onofrio N, et al. SGLT-2 inhibitors and in-stent restenosis-related events after acute myocardial infarction: an observational study in patients with type 2 diabetes. BMC Med 2023; 21: 71.
60.
Paolisso P, Bergamaschi L, Cesaro A, et al. Impact of SGLT2-inhibitors on contrast-induced acute kidney injury in diabetic patients with acute myocardial infarction with and without chronic kidney disease: insight from SGLT2-I AMI PROTECT registry. Diabetes Res Clin Pract 2023; 202: 110766.
61.
Rahim I, Sayed RK, Fernández-Ortiz M, et al. Melatonin alleviates sepsis-induced heart injury through activating the Nrf2 pathway and inhibiting the NLRP3 inflammasome. Naunyn-Schmiedeberg’s Arch Pharmacol 2021; 394: 261-77.
62.
Gurbanov R, Kalkanci B. SLC6A4 (solute carrier family 6 member 4). Atlas Atlas Genet Cytogenet Oncol Haematol 2020; 24: 39-50.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.