In recent years, the use of electronic nicotine delivery systems (ENDS) has dramatically increased, particularly as an alternative to traditional tobacco smoking. In the United States, it is estimated that about 8 million adults have used ENDS at some point in their lives [1]. While the association of ENDS with myocardial infarction has been suggested by multiple studies, their association with stroke remains unclear and inconsistent across relevant studies [2]. Therefore, we conducted this meta-analysis to evaluate the relationship between ENDS use and the risk of stroke when compared to non-smokers.
Methods
A comprehensive search of PubMed, Scopus, and Web of Science was conducted from inception year of each database until June 15, 2023, using a combination of relevant keywords such as “e-cigarette”, “ENDS” and “stroke”. We included observational studies that assessed association of current or former usage of ENDS with risk of stroke compared with non-smokers, reported the risk estimate as odds ratio (OR) or hazard ratio (HR) with a 95% confidence interval (CI), and adjusted for possible confounders (as per each individual study). We assessed the risk of bias in cohort studies using the Newcastle-Ottawa Scale and in cross-sectional studies using the Agency for Healthcare Research and Quality checklist. Under the assumption of rare event prevalence (< 10%), we employed the random-effects model to combine adjusted risk estimates as a pooled OR with corresponding 95% CI. We used the I2 and χ2 tests for heterogeneity assessment. A leave-one-out sensitivity analysis was conducted to assess the impact of each individual study on the overall combined risk estimate. Furthermore, an additional sensitivity analysis was conducted, excluding studies that utilized HR as their risk estimate. Due to the inclusion of < 10 studies in this meta-analysis, it was not possible to reliably assess publication bias using funnel plot asymmetry tests, as recommended by Cochrane. All analyses were conducted using MetaXL version 5.3 (Microsoft Excel add-in; www.epigear.com).
Results
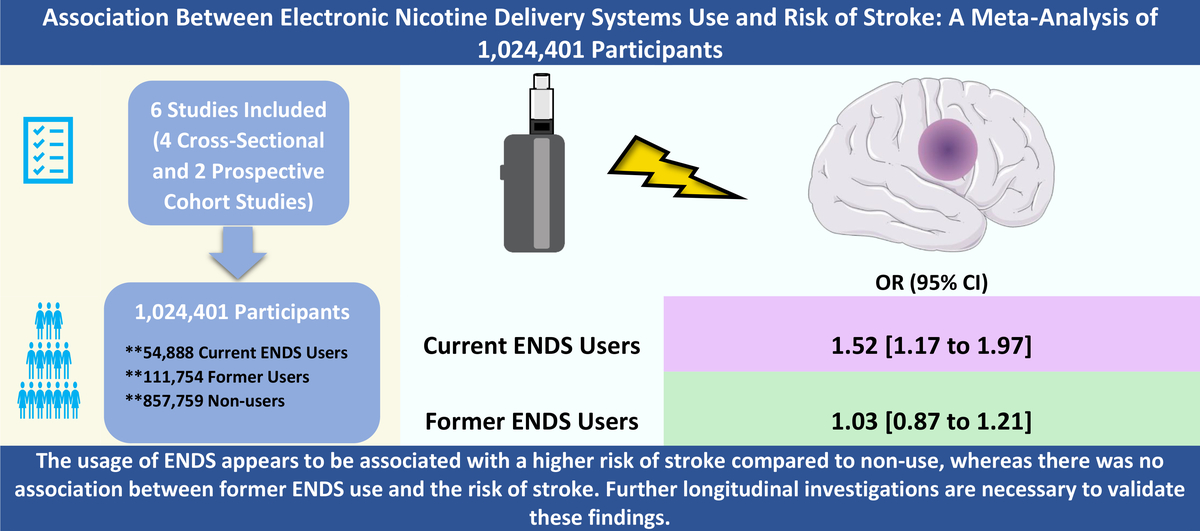
Our search yielded 296 unique records, of which 19 articles underwent full-text screening. Only 6 studies (4 cross-sectional and 2 prospective cohort studies) matched our criteria and were included in this meta-analysis [3–8]. A total of 1,024,401 participants were included in our analysis, consisting of 54,888 current ENDS users, 111,754 former users, and 857,759 non-users. All included studies were conducted in the USA and were published between 2021 and 2023. All studies reported their risk estimates as ORs, except for two studies, which reported HRs [5, 8]. Both included cohort studies were of high quality and scored 8 out of 9 on the Newcastle-Ottawa Scale. Moreover, the cross-sectional studies showed acceptable quality; however, these studies relied on self-reported stroke diagnosis, which may be a potential source of bias.
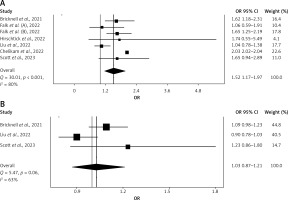
The analysis revealed that ENDS use was associated with a statistically significant increased risk of stroke (OR = 1.52; 95% CI: 1.17–1.97; Figure 1 A) compared with non-users. However, a non-significant association was found between former ENDS use and risk of stroke (OR = 1.03; 95% CI: 0.87–1.21; Figure 1 B). Significant heterogeneity was observed in both current and former ENDS use analyses (I2: 80% and 63%, respectively). Leave-one-out sensitivity analysis confirmed the robustness of both presented results. In addition, exclusion of the two studies that employed HR as their risk estimate did not change the result significance in terms of current ENDS use (OR = 1.49; 95% CI: 1.10–2.01).
Discussion
The current meta-analysis, which included over one million participants, suggested that the use of ENDS may be associated with approximately a 50% increased risk of stroke compared to non-smokers. However, the analysis found no significant association in the case of former ENDS users, emphasizing the importance of smoking cessation. Multiple meta-analyses have consistently reported a significant increase in the risk of stroke among former traditional tobacco smokers, in contrast to the findings related to former ENDS use. Nevertheless, this discrepancy may be attributed to the limited number of available studies assessing the risk of stroke associated with former ENDS use.
Long-term exposure to nicotine has been recognized to significantly elevate the risk of developing atherosclerosis, consequently increasing the likelihood of experiencing a stroke. Besides nicotine, ENDS contain other harmful components, such as carbonyls (e.g., acrolein, formaldehyde, and acetaldehyde), benzene, toluene, as well as fine and ultrafine particulate matters [9]. Many of these components have been linked to various pathophysiological mechanisms that could potentially explain the observed rise in stroke risk. These mechanisms involve damaging of the blood-brain barrier, blood pressure elevation, impairment of vascular repair, induction of vascular inflammation and injury, endothelial dysfunction, and platelet activation, all of which contribute to an increased susceptibility to thrombosis [9].
In a recent meta-analysis, Zhao et al. [10] aimed to assess the association of ENDS use with the risk of stroke. However, their analysis included a study that did not report stroke as a separate outcome but rather as part of the composite cardiovascular diseases’ outcome. In addition, another completely unrelated study, to the analysis objectives, that assessed the awareness (by sociodemographic variables) of the health effects of ENDS use was included. Therefore, the reliability of that analysis is compromised, and it should not be considered as a credible reference on this issue.
This meta-analysis has some limitations. Most of the included studies (4 out of 6) had a cross-sectional design, and as a result the temporal association of ENDS and the risk of stroke still needs to be established in future cohort or case-control studies. Additionally, the reliance on surveys and self-reporting methods (e.g., stroke history) for data collection might have been a source for recall and non-response biases. Furthermore, the study by Chelikam et al. [7] did not adjust for possible history of traditional smoking. Lastly, there is insufficient reported data on the frequency and duration of ENDS use, as well as the different types of strokes in the included studies.
In conclusion, the usage of ENDS appears to be associated with a higher risk of stroke compared to non-use, whereas there was no association between former ENDS use and the risk of stroke. However, further longitudinal investigations are necessary to validate these findings.