Introduction
Congenital heart anomalies (CHAs) represent a major burden to global child health, particularly in regions with a low Socio-demographic Index (SDI) [1]. Although global data from 1990 to 2021 show a modest decline in the overall prevalence of CHAs, mortality rates remain disproportionately high in low-SDI areas, reflecting persistent gaps in public health infrastructure and access to medical care. This disparity underscores that while prevalence has only slightly decreased, the associated mortality has declined more markedly, likely due to advancements in diagnosis and treatment in higher-SDI settings [2, 3].
Recent advancements in CHA diagnosis and treatment, such as routine use of fetal echocardiography and pulse oximetry for early screening, and the critical roles of 3D printing and virtual reality in surgical planning, have been significant [4–8]. Additionally, the advancement of interventional catheter techniques and minimally invasive surgical approaches has expanded treatment options, reduced surgical risks, and improved long-term outcomes. However, data from 204 countries reveal significant regional variations in CHA incidence and mortality rates, with the highest mortality rates in low-SDI regions. These findings underscore the impact of disparities in public health strategies and healthcare services across regions on the survival and quality of life of CHA patients.
In the Global Burden of Disease (GBD) framework, CHAs are classified into five sub-categories based on anatomical features and treatment requirements: 1) single ventricle and single ventricle pathway defects; 2) complex congenital heart defects excluding single ventricle cases; 3) malformations of great vessels, congenital valvular heart disease, and patent ductus arteriosus; 4) ventricular septal defects (VSD) and atrial septal defects (ASD); and 5) other congenital cardiovascular anomalies. A proportion of VSD/ASD cases with favorable outcomes and no clinical symptoms are modeled as asymptomatic. These classifications enable more accurate modeling and burden estimation of CHA worldwide [9].
This study used the Global Burden of Disease (GBD) database to analyze CHA trends and outcomes in children across socioeconomic backgrounds, aiming to provide insights for healthcare professionals to refine prevention and management strategies and ultimately reduce CHAs’ global impact on children.
By leveraging the most up-to-date GBD 2021 data, the study further examined disparities across SDI levels and between sexes, addressing gaps in current literature. These findings are intended to inform equitable resource allocation and guide public health planning toward improving cardiovascular outcomes among children worldwide.
Material and methods
Data collection and approval
This cross-sectional study was approved by the Ethical Board of Wenzhou People’s Hospital, with a waiver of informed consent granted due to the use of de-identified data analysis. Data concerning children aged 0 to 14 years with CHAs were collected using the Global Health Data Exchange tool developed by the GBD study collaborators, covering prevalence, mortality, and disability-adjusted life years (DALYs). DALYs are a summary measure used to quantify the overall burden of disease. They represent the total number of healthy years lost due to illness, disability, or premature death. DALYs are the sum of two components: years of life lost (YLLs) due to premature mortality and years lived with disability (YLDs) due to time spent in less than full health. These metrics were assessed for the period 1990–2021 across 204 countries and territories [10].
Global and regional burden analysis
We generated global maps and regional comparative analyses to explore the burden of CHAs, using R (version 4.4.1) with ggplot2 and sf packages for visualization.
Temporal trend analysis
Trends in CHA metrics from 1990 to 2021 were assessed using Joinpoint regression analysis with the Joinpoint R package, calculating both annual percent change (APC – the yearly percentage change of a specific health indicator over a given time period; it reflects the direction and magnitude of the trend, typically calculated using a log-linear regression model, and represents the relative change per year compared to the previous year) and estimated annual percentage change (EAPC – a summary measure derived from fitting a regression model to time-series data, estimating the average annual percent change over time; it includes a 95% confidence interval and is widely used in epidemiological studies to assess whether the trend of a health outcome is increasing, decreasing, or stable over a specific period) with 95% CIs to identify significant changes over time.
Population and SDI analysis
Population-level data were stratified by age, sex, and SDI categories, analyzing the relationship between socioeconomic development and CHA burden. Descriptive statistics and SDI-specific disease rates were computed, with data manipulation and visualization conducted using dplyr and ggplot2 packages in R.
Results
CHAs in children: global trends
Prevalence
A total of 218,909,652 children – 113,892,505 (52.03%) males; 105,017,147 (47.97%) females – were included in the analysis. From 1990 to 2021, the global prevalence of CHAs decreased by 4.294% (95% UI: –5.696–2.695%). The corresponding prevalence rate decreased accordingly from 377.257 cases per 100,000 people (95% UI: 333.461–424.687) in 1990 to 361.060 cases per 100,000 people (95% UI: 320.042–406.507) in 2021; the EAPC was 0.007 (95% CI: –0.041 to –0.055) (Table I).
Table I
Prevalence of CHA in children from 1990 to 2021 globally, in five SDI regions, and 21 areas
From 1990 to 2021, the prevalence among children under one year of age showed a declining trend, with the most significant decrease observed in neonates within the first 28 days of life (3.661%). Conversely, the prevalence among children over 1 year of age increased, with the most pronounced increase observed in children aged 5 to 14 years (22.423%). In 1990 and 2021, the prevalence rates of CHAs in neonates within the first 28 days of life were 1.551% and 1.539%, respectively (Figure 1 and Supplementary Table SIII).
In 2021, the prevalence of CHAs was higher in girls than in boys. The male–female ratio of CHA prevalence among children in different age groups followed a unimodal distribution, peaking in neonates within the first 28 days of life (Supplementary Table SIII and Figure 1).
Death
Over the past 30 years, the global number of child deaths related to CHAs decreased by 55.336% (from 497,979 deaths with a 95% UI of 282,166–642,052 in 1990 to 222,415 deaths with a 95% UI of 181,359–275,182 in 2021). Similarly, the mortality rate associated with CHAs decreased from 28.633 deaths per 100,000 people (95% UI: 16.224–36.918) in 1990 to 11.055 deaths per 100,000 people (95% UI: 9.014–13.678) in 2021; the EAPC was –2.574 (95% CI: –2.737 to –2.410) (Supplementary Table SI).
A decrease in the mortality rate associated with CHAs was observed across all age groups of children. The largest decrease in the mortality rate (49.515%) occurred in newborns within the first 28 days of life. In 2021, among children under 1 year of age and those aged 2–4 years, the mortality rate associated with CHAs was higher in boys than in girls (rate per 100 000 children under 28 days of age: boys, 914.500 deaths; girls, 595.260 deaths; 1–5 months: boys, 117.663 deaths; girls, 106.471 deaths; 6–11 months: boys, 53.867 deaths; girls, 52.275 deaths; 2–4 years: boys, 4.487 deaths; girls, 4.125 deaths). In children aged 12–23 months and 5–14 years, the rate was higher among girls than among boys (12–23 months: boys, 14.568 deaths; girls, 14.813 deaths; 5–14 years: boys, 1.337 deaths; girls, 1.351 deaths). In boys, the lowest CHA-associated mortality rate was observed among those aged 5 to 14 years (1.337); in girls, the lowest rate was observed among those aged 2 to 4 years (1.351) (Supplementary Table SIV and Supplementary Figure S1).
DALYs
From 1990 to 2021, the global number of DALYs associated with CHAs in children decreased by 54.588%, from 44,749,235 (95% UI: 25,585,020–575,955,340) in 1990 to 20,321,186 (95% UI: 16,692,532–25,028,860) in 2021. The EAPC was –2.527 (95% CI: –2.687 to –2.366) (Supplementary Table SII).
Over the same period, there was a decline in the DALY rate associated with CHAs for children in all age groups. The greatest reduction (62.977%) occurred among children aged 12–23 months. In both 1990 and 2021, the highest number of DALYs associated with CHAs was observed in children under 28 days of age, with 13,611,565 DALYs in 1990 and 6,674,473 DALYs in 2021. In 2021, the DALY rate for CHAs in children aged 12–23 months was higher among girls (1,367.344 per 100,000) than boys (1,349.648). For all the other age groups, boys had a higher DALY rate than girls did (Supplementary Table SV and Supplementary Figure S2).
CHAs in children: SDI regional trends
Prevalence
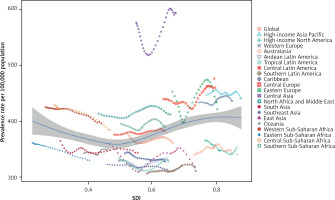
In 2021, the low-middle-SDI group had the highest number of cases of CHAs in children (2,068,011 cases; 95% UI: 1,819,242–2,328,074). The greatest decrease in the prevalence of CHAs among children was observed in the low-SDI group (EAPC = –0.177; 95% CI: –0.205 to –0.149) (Table I, Figure 2).
Death
Across the five SDI groups, a significant decrease in mortality rates linked to CHAs in children was observed. Notably, the low-SDI regions presented the highest number of deaths related to CHAs (86447; 95% UI: 59760–117370, p < 0.001), whereas the high-middle-SDI regions presented the greatest reduction in CHA-related mortality rates (81.362%). In 2021, the highest mortality rate for CHAs in children was observed in low-SDI regions (18.784; 95% UI: 12.985–25.503), and the lowest mortality rate was observed in high-SDI regions (2.366; 95% UI: 1.926–2.874). Among these regions, the high-middle-SDI regions had the lowest EAPC in CHAs-related mortality (–4.867; 95% UI: –5.148 to –4.585) (Supplementary Table SI, Supplementary Figure S3).
DALYs
In 1990, the global rate of DALYs for CHAs in children aged 0-14 years was 2,573.050 (95% UI: 1,471.121–3,311.704) per 100,000 people. By 2021, this figure had decreased to 1,010.069 (95% UI: 829.706–1,244.065), indicating a long-term downward trend (p < 0.001). Among the regions, the low-SDI regions had the highest DALY rate in 1990, at 3,525.146 (95% UI: 1,266.476–5,155.793) per 100,000 people (p < 0.001). By 2021, this rate had dropped to 1,692.466 (95% UI: 1,175.580–2,285.878), approximately halving the burden. Regarding sex differences, the charts indicated that, globally, male children usually had a higher rate of DALYs than females did, a trend that was consistent across different SDI regions and especially pronounced in the low-SDI regions (Supplementary Table SII, Supplementary Figure S4).
CHA in children: geographic regional trends
Prevalence
Among 21 geographic regions globally, South Asia had the highest number of CHA cases in children in 1990, totaling 1,578,563 (95% UI: 1,374,375 to 1,808,754), whereas Oceania had the fewest, with only 9,179 cases (95% UI: 8,052 to 10,452). By 2021, South Asia still had the highest number of cases, at 1,739,987 (95% UI: 1,531,918 to 1,978,759); the number of cases in Oceania slightly increased to 9,179 (95% UI: 15,515 to 20,228). Additionally, in 1990, the lowest prevalence of CHAs in children was in Tropical Latin America, at 333.760 cases per 100,000 people (95% UI: 269.048 to 355.529), with Central Asia having the highest prevalence, at 575.927 cases per 100,000 (95% UI: 503.846 to 659.502). By 2021, Southern Latin America had the lowest prevalence, at 310.790 cases per 100,000 people (95% UI: 300.230 to 373.028), Central Asia had the highest rate, at 592.915 cases per 100,000 people (95% UI: 517.648 to 678.322). From 1990 to 2021, the greatest increase in the prevalence of CHAs in children was observed in Eastern Europe, with an average annual percentage change of 0.330 (95% CI: 0.125 to 0.536), whereas Eastern Sub-Saharan Africa experienced a decline, with an average annual percentage change of –0.305 (95% CI: –0.333 to –0.277). At the global and continental levels, the prevalence of birth defects showed a slight increase with rising socio-demographic index (SDI) levels (r = 0.2135, p < 0.001), indicating a weak but positive correlation between prevalence and SDI (Table I, Figure 3).
Death
In 1990, South Asia had the highest number of deaths from CHAs in children, totaling 116,856 deaths (95% UI: 72,956 to 162,097), whereas Australasia had the fewest, at 247 deaths (95% UI: 225 to 276). By 2021, South Asia still had the highest number of deaths at 51,312 (95% UI: 36,235 to 72,898), with an SDI of 0.558; Australasia had the fewest deaths at 95% UI, 68 to 119, with an SDI of 0.846. From 1990 to 2021, the high-income Asia–Pacific region experienced the largest decrease in the mortality rate, with an EAPC of –5.352; however, Central Asia experienced a slight increase in the mortality rate, with an EAPC of 0.920 (95% CI: 0.608 to 1.232). In 2021, the mortality rates in 13 regions were above the global average (11.055 deaths per 100,000 people), whereas those in 14 regions were below the global average. The correlation analysis between DALYs and SDI revealed that with increasing SDI levels, DALYs decreased significantly, indicating a strong negative correlation between DALYs and SDI (r = –0.8307, p < 0.001) (Supplementary Table SI and Supplementary Figure S5).
DALYs
In 1990, East Asia had the highest number of DALYs associated with CHAs in children, totaling 10,443,910 (95% UI: 6,546,745 to 14,441,534). By 2021, Southeast Asia had the highest number, with 4,697,324 DALYs (95% UI: 3,334,571 to 6,610,005), whereas Australasia had the lowest number, at only 10,356 (95% UI: 7,848 to 12,726). During this period, Oceania had the highest DALY rate, at 2,911.336 per 100,000 people (95% UI: 1,203.550 to 4,414.854); Australasia had the lowest rate, at 180.695 per 100,000 people (95% UI: 136.939 to 222.045). From 1990 to 2021, Central Asia experienced an increase in the DALY rate (EAPC = 0.916; 95% CI: 0.610 to 1.223), whereas East Asia experienced the most significant decrease (EAPC = –5.197; 95% CI: –5.48– –4.913, p < 0.001). In 2021, 9 regions had DALY rates above the global average (1010.069) and 12 regions had rates below it. The analysis showed a strong negative correlation between mortality rate and SDI, with mortality rate decreasing significantly as SDI increased (r = –0.8325, p < 0.001) (Supplementary Table SII, Supplementary Figure S6).
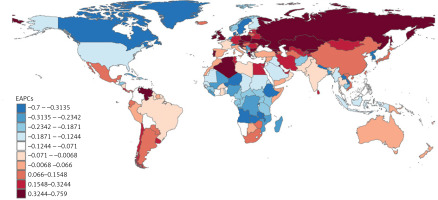
Prevalence
In 2021, among 204 countries, India had the highest number of CHA cases in children, with 1,249,145 cases (95% UI: 1,101,670–1,412,452). Armenia had the highest prevalence of CHAs in children, at 649.051 cases per 100,000 people (95% UI: 566.055–741.582). Georgia experienced the largest increase in the prevalence of CHAs in children (EAPC = 0.759; 95% CI: 0.523–0.995), whereas Equatorial Guinea experienced the largest decrease (EAPC = –0.700; 95% CI: –0.710 to –0.689). In 2021, India had the highest prevalence of CHAs among children, while Dominica had the lowest value. The global prevalence of CHAs in children in 2021 was 361.060 (95% UI: 320.042–406.507); 97 countries had a prevalence rate higher than the global average, and 107 countries had a prevalence rate lower than the global average (Supplementary Table SVI, Figure 4).
Death
In 2021, India had the highest number of deaths related to CHAs among children, totaling 35,232 (95% UI: 25,272–50,611). Afghanistan had the highest mortality rate for CHAs among children, at 59.127 (95% UI: 28.978–84.462), whereas San Marino had the lowest, at 0.446 (95% UI: 0.246–0.796). Guatemala experienced the largest increase in the mortality rate, with an EAPC of 3.234 (95% CI: 2.428–4.046); conversely, Saudi Arabia experienced the most significant decrease, with an EAPC of -7.888 (95% CI: –8.028 to –7.749). In 2021, Afghanistan had the highest mortality rate related to CHAs among children, whereas San Marino had the lowest rate. The global mortality rate for CHAs in children in 2021 was 11.055 (95% UI: 9.014–13.678), with 58 countries having rates above the global average and 146 countries having rates below it (Supplementary Table SVII, Supplementary Figure S7).
DALYs
In 2021, India had the highest number of DALYs related to CHAs among children, totaling 3,239,958 (95% UI: 2,351,581–4,603,448). Afghanistan had the highest rate of CHAs-related DALYs among children, at 5,306.324 (95% UI: 2,618.402–7,558.485). Guatemala experienced the largest increase in DALY rates for CHAs, with an EAPC of 3.151 (95% CI: 2.372 to 3.936). Conversely, Saudi Arabia and Turkey experienced the most significant decreases, with EAPCs of –7.605 (95% CI: –7.754 to –7.455) and –5.17 (95% CI: –5.50 to –4.84), respectively. Afghanistan had the highest DALY rate related to CHAs among children, whereas San Marino had the lowest rate. In 2021, the global DALY rate for CHAs among children was 1,010.069 (95% UI: 829.706–1,244.065), with 59 countries having rates above the global average and 145 countries having rates below it (Supplementary Table SVIII, Supplementary Figure S8).
Discussion
Data from the last thirty years reveal significant regional disparities in the impact of CHAs on children aged 0 to 14 years across different economic areas worldwide. With increasing medical and societal costs, CHA has emerged as a significant concern within the global public health sphere. This study, which used GBD data from 1990–2021, examined the prevalence, mortality and DALY rates of CHAs among children in regions with varying SDIs [11–13]. The findings highlight that despite overall advancements in medical technology, the burden of CHAs remains pronounced in lower-middle-SDI regions. This underscores the persistent challenges in addressing CHAs faced globally and highlights areas where urgent interventions are needed. This study underscores the importance of developing targeted prevention and management strategies to address the specific needs of these populations, aiming to foster the development and refinement of global public health policies.
From 1990 to 2021, there was a significant decrease in the number of deaths and DALYs associated with CHAs in children aged 0 to 14 years worldwide. This trend is likely due to advancements in medical technology, more effective early intervention measures, and increased attention to pediatric cardiac health within global health systems. Research indicates that improved neonatal cardiac screening and treatment techniques have significantly reduced mortality and health burdens in these age groups [14–17]. However, despite a slight decrease in the global prevalence of CHAs in children, the total number of cases has increased, primarily due to population growth, lifestyle changes, and environmental changes driven by globalization [18, 19]. In particular, the notable increase in prevalence among children aged 5 to 14 years may reflect the accumulation and manifestation of potential cardiac risk factors as children age.
Moreover, our study revealed sex differences in the distribution of CHAs, with higher incidence rates among girls than boys. These differences might be related to genetic factors, hormonal levels, and their impacts on cardiac development [20–22]. SDI analysis revealed that regions with higher SDIs experienced more pronounced decreases in CHA prevalence, likely due to greater investment in healthcare resources, broader coverage of health services, and better living conditions in these areas [23].
With the acceleration of globalization, the risk factors for CHAs have also shown certain trends. Advances in genetic technology have enabled more accurate identification of genetic and chromosomal abnormalities related to CHAs [24], whereas global changes in environmental pollution and lifestyles have led to new triggers for the development of CHAs. Additionally, as the prevalence of CHAs and other chronic diseases increases among pregnant women, these conditions become significant factors affecting fetal cardiac development [25].
In terms of global disease surveillance and health strategies for CHAs, some progress has been made, especially in high-SDI regions, where improved prenatal and antenatal health screenings have reduced the incidence and mortality associated with CHAs.
Beyond postnatal treatment improvements, the widespread adoption of prenatal screening – including fetal echocardiography – has allowed for earlier detection of severe cases, enabling informed decisions such as selective termination of pregnancies with fatal or uncorrectable anomalies. In certain cases, in utero interventions have also been implemented to address specific defects prior to birth. These strategies have collectively contributed to the observed decline in CHA-related mortality in high- and middle-SDI regions. Their integration into public health policy in lower-SDI regions could offer significant benefits in mitigating the burden of CHAs. However, due to the limited resources and inadequate health education, low-SDI regions still face challenges in prevention and early intervention for CHAs [11, 26].
Future policy directions should focus more on the equitable distribution of global health resources, particularly in terms of enhancing medical facilities and public health education levels in low-SDI regions. Furthermore, strengthening international cooperation and sharing effective genetic screening and environmental intervention technologies may be key to reducing the global burden of CHAs.
This study has several limitations. First, the analysis relied heavily on the GBD database, meaning that data accuracy may be constrained by the completeness of national registry data and the number of undiagnosed cases. Additionally, due to the lack of detailed classification of congenital heart anomalies (CHAs) into anatomical and functional types, this study could not provide in-depth insights into specific epidemiological characteristics. Moreover, the study did not include a systematic analysis of risk factors associated with CHAs, limiting our understanding of how these factors influence CHA development. Furthermore, low- and middle-income countries (LMICs) often lack comprehensive CHA registries, with many regions relying solely on limited hospital records or localized data, which may not be representative, potentially underestimating the burden of CHAs in certain areas. For instance, in resource-limited countries such as Myanmar, the absence of key data on CHAs further exacerbates errors in global burden estimates. Additionally, the underdeveloped public health infrastructure in LMICs, coupled with inadequate screening and diagnostic capabilities, may result in many CHA cases being undiagnosed or misdiagnosed, further affecting the accuracy of burden estimation. Biases in sample selection may also impact data representativeness, compromising the reliability of global burden estimates. While this study employed data weighting and multi-source calibration methods to mitigate these biases and validated its findings by comparing them with data from high-income countries, the impact of missing or low-quality data cannot be fully eliminated. Future research should focus on refining data categorization methods to incorporate more detailed CHA classification and explore new methodologies, such as predictive models, to more accurately assess and manage the global CHA burden. Additionally, strengthening CHA screening systems in LMICs, enhancing diagnostic capabilities, and improving data collection and long-term monitoring mechanisms will help reduce data bias and provide a more scientific and accurate foundation for developing public health policies and interventions.
In conclusion, this study demonstrated that despite significant advancements in the treatment and diagnosis of CHAs in children over the past three decades – reflected in the decline in the associated mortality rates and DALYs – the prevalence of CHAs has remained relatively unchanged. Research has also highlighted significant disparities in CHA incidence across different sexes and SDI regions, highlighting global inequalities in the distribution of public health resources and health education. Future policies need to address these disparities with targeted strategies to alleviate the global burden of CHAs, especially by enhancing resource allocation and international cooperation among low-SDI regions.