Introduction
As living standards gradually improve, people’s eating habits change to a high protein, high fat, high energy and low fiber food diet; in addition people relieve stress by smoking and drinking alcohol, with a lack of exercise. These poor diet and lifestyle habits are among the risk factors for the increased number of colorectal cancer patients [1]. In 2012, the World Health Organization (WHO) announced the 20 countries with the largest number of new colorectal cancer cases and deaths in the world, and China ranked first [2]. As of 2017, more than 2.2 million patients have been diagnosed with colorectal cancer worldwide. There are 376,000 cases of colorectal cancer in China, and about 60% of the patients have low rectal cancer. Doctors can reduce the mortality and the incidence of postoperative anastomotic fistulae by establishing permanent or temporary enterostomy [3–6]. Enterostomy refers to the operation used to treat some intestinal diseases (such as rectal cancer and colon cancer). A surgeon will pull out a section of the intestinal lumen, turn it over, and sew it to the abdominal wall, thus forming an artificial opening [7]. There are more than 1 million patients with enterostomy in China, and the incidence of complications ranges from 22.8% to as high as 42.6% [8, 9]. Fecal water dermatitis is one of the common complications after enterostomy, and 45% of patients develop different degrees of fecal water dermatitis after the operation [10]. This not only increases the economic burden of patients [11] but also seriously affects the confidence of patients’ postoperative rehabilitation and quality of life [12].
In the present study, 79 patients with enterostomy in our hospital from April to July 2017 were examined, and 36 patients had fecal water dermatitis. The incidence was 45.56%, while the incidence in Chinese counterparts was only 22.80% [13]. In other countries, group interaction [14] and systematic management models [15] have been adopted for patients with fecal water dermatitis, achieving remarkable results. Early screening and prevention of fecal water dermatitis in patients with enterostomy in China are still in their infancy. However, the nutritional support of clinical medical staff in our department for patients with fecal water dermatitis is low and does not meet patients’ needs. In clinical practice, there is a lack of scientific and reasonable protective measures, and no effective management model has been established. Researchers such as Bai [16] found that in the multidisciplinary management of early postoperative dysphagia screening and rehabilitation of patients with cerebral hemorrhage, nurse-led multidisciplinary management has a significant effect. Therefore, in this study, through the establishment of nurse-led multidisciplinary cooperation in the management of enterostomy, we implemented a management plan of prevention of fecal water dermatitis in patients with enterostomy to identify and prevent fecal water dermatitis early and reduce the incidence of fecal water dermatitis and improve patients’ quality of life. The details are reported as follows.
Material and methods
Establish a nurse-led multidisciplinary enterostomy management team
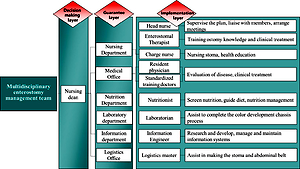
Under the colorectal cancer multidisciplinary team in our hospital, a nurse-led multidisciplinary enterostomy management team was established. The members include the following: four colorectal surgeons, one head nurse, two enterostomy therapists, five charge nurses, two information engineers, one dietitian, one clinical laboratory physician, and one logistics master.
Based on the multidisciplinary team of colorectal cancer in our hospital, a multidisciplinary enterostomy management team led by the nursing dean has been established, which consists of the nursing department, the medical department, the nutrition department, the laboratory department, the logistics department and the information department, and the three-step enterostomy management framework is composed of special administrators of each department. The construction team consisted of 4 colorectal surgeons, 1 head nurse, 2 enterostomy therapists, 5 nurses as cashiers, 2 information engineers, 1 nutritionist, 1 laboratorian, and 1 logistics master.
The relationships and roles of personnel of our colorectal cancer multidisciplinary team are shown in Figure 1.
Selection of participants
Inclusion criteria: (1) patients who underwent ileostomy, transverse colostomy, and sigmoid colostomy; (2) patients who could read and write; (3) patients without senile dementia; and (4) patients and their families provided signed informed consent. Exclusion criteria: (1) patients with mental illness and communication disorders; (2) patients with conscious disturbance or severe cognitive impairment; and (3) patients with language communication impairment. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of Shanxi University of Chinese Medicine and informed consent was taken from all the patients.
Implementation of early screening and protection measures of fecal water dermatitis in patients with enterostomy
According to the results of the evidence-based process, the “multidisciplinary procedure for prevention of fecal water dermatitis in patients with enterostomy” was formulated, as shown in Figure 2.
Specific implementation steps:
Revise the nutrition management system for patients with enterostomy
The low screening rates and long intervention times were analyzed, including the following: (1) Single assessor: evaluation was carried out relying on the dietitian only. Due to the large number of inpatients, the ward was not equipped with a full-time nutrition manager, so patients waited a long time for evaluation. (2) The intervention time of assessors was long: the nutritionist’s intervention time was up to 72 h, resulting in malnutrition, fistula retraction, and difficulty in excreta collection.
Improvement of measures: (1) The training and assessment of nutrition screening for nurses by nutrition doctors were as follows: the content and knowledge of nutrition screening forms were taught, and the nurses’ qualification rate was more than 90%. (2) After admission, 1–5 days after surgery, the responsible nurse used the NRS2002 Nutritional Risk Assessment form [17] to screen patients’ nutritional risk; dietitian intervention was performed for those with a score of ≥ 3. (3) Based on the results of nurses’ nutritional assessment, the nutrition department doctors implemented dynamic nutritional management for patients at nutritional risk within 48 h, and colorectal surgeons and nutritionists worked out a nutrition treatment plan together.
Construction of nurse-led whole process management model with enterostomy patients as the center
The existing factors of imperfect nursing measures for enterostomy were analyzed. The correct rate of stoma positioning by nurses was low. The early detection rate of fecal water leakage (within 1 h) was only 4.48%. The traditional enterostomy abdominal belt rolls up easily at the edge, causing basement edge warping and fecal water leakage.
Improvement of measures: (1) General nurses were trained in combining theory with practice: first, enterostomy therapists trained nurses in stoma structure, positioning, and nursing. Then, the head nurse explained the specific content of the PIO physical assessment kit and carried out clinical guidance and assessments. Before enterostomy, under the doctors’ guidance, the responsible nurses and doctors jointly completed the preoperative stoma positioning and health guidance. First of all, the ostomy surgeon developed a training plan for theory and clinical practice. The training period was 2 months, twice a week, 50 min each time. The theoretical teaching was conducted in the form of PPT combined with blackboard writing, including the physiological structure of enterostomy, positioning of enterostomy and enterostomy nursing knowledge. Clinical practice teaching was conducted in the form of mutual simulation of patients by responsible nurses, and the training contents included the use of a PIO body evaluation kit, measurement and cutting of the ostomy chassis, pasting the ostomy bag and basic skills of ostomy nursing, etc. (2) On the day of the operation, a stoma basement was prepared on the colored bowel. The laboratory physician selected the color reagent, and the information engineer drew the colored stoma basement drawing. The imaging layer was added on one side of the basement body. When the basement meets the fecal water, it turns green so nurses can find the fecal water leakage in time and replace the stoma basement. (3) On the day of the operation, the new enterostomy abdominal belt was worn. The information engineer drew the structural drawings of the new type of abdominal belt, and the logistics master thickened the abdominal belt. The belt supports the patient’s waist and could reduce the displacement of the abdominal belt, avoid basement warping, and reduce fecal water leakage. (4) Standardizing the shift handover process for enterostomy patients: The items of stoma exhaust, color, basement, bracket, and stitching removal were added to the shift handover record sheet. During shift handovers, rose signs were added at the head of the bed to remind the nurses on each shift to observe the stoma condition of patients and carry out nutritional risk screening. (5) The Self-Management Manual for Patients with Enterostomy was issued and explained in detail on the first and second day after the operation. (6) On days 3–5 after the operation, the responsible nurse demonstrated the nursing process of enterostomy to the patients and their families. When the basement was replaced for the second time, the patients and their family members were instructed to take enterostomy care by reverse teaching. Stomatologists used adhesive pressure tools to explain and demonstrate the adhesion method of the stoma basement. They also recorded the construction of stoma pockets, demonstrated adhesive pressures of stoma basements, the replacement of stoma basements and stoma pockets, and nursing of the stoma and surrounding skin into educational videos. Nurses arranged for patients and their families to watch the video together in the training classroom and uploaded it to the information platform for patients to learn by themselves. (7) On the sixth day after the operation, the responsible nurses scored the patients by using the Evaluation Guidance Sheet and the Self-Care Ability Evaluation Sheet for Patients with Enterostomy, then strengthened the education of content that the patients did not understand. (8) Before discharge, the responsible nurse taught patients to use the APP Management Platform for Enterostomy Patients and invited patients to join the WeChat group established by medical staff for regular follow-up. Follow-up was conducted 1 week, half a month and 3 months after discharge. Follow-up was conducted in the form of WeChat, telephone and APP management platform.
Information management of patients with enterostomy based on APP management platform
The imperfect information platform factors were analyzed. The existing official account of WeChat only pushes the knowledge of enterostomy and cannot interact with patients. The layout lacks the knowledge that patients find easy to accept and cannot meet patients’ needs.
Improvement of measures: Based on an Addie model, we made a questionnaire to investigate the general situation, psychological status, self-efficacy, and quality of life of patients with enterostomy. This questionnaire was to help us understand the needs of patients with enterostomy. We designed an enterostomy health education knowledge module with information department engineers, created an APP management platform for patients with enterostomy, and built the hospital and patient site. The responsible nurses provided individualized guidance for patients with enterostomy through the APP management platform and completed remote follow-up after discharge to complete the information-based and intelligent whole process management.
Quality control
Completing the nursing records: The record sheet included the first nutritional screening of patients with enterostomy, the time of nutritional management intervention, the accurate positioning of the stoma before the operation, the screening of early detection of fecal water dermatitis (within 1 h), and the edge warping of the stoma basement.
The colorectal surgery specialist nursing quality index was used for quality control analysis. Based on the literature review, evidence-based results, and expert consultation, the incidence of fecal water dermatitis in patients with enterostomy was set as the main index of specialized nursing in colorectal surgery. Other secondary quality indicators included the screening rate by nurses of nutritional risks for patients with enterostomy, the correct positioning rate of enterostomy for patients by responsible nurses, the incidence of basement warping for patients with enterostomy, the incidence of fecal water leakage, the incidence of stoma basement leakage in the early stage (within 1 h), the awareness rate of relevant knowledge of enterostomy patients, and the self-care ability of patients with enterostomy (family members). Enterostomy therapists acted as quality control specialists. They registered the above indicators daily, conducted statistical analysis every month, fed back the existing problems in the department’s morning meeting, and continuously improved the quality to reduce the incidence of fecal water dermatitis in patients with enterostomy.
Strengthening communication and learning among members: A WeChat group was set up to provide feedback on patients’ condition information, adjust patients’ treatment and nutritional support plans, and send new guidelines and materials for members to learn.
Statistical analysis
Statistical software SPSS22.0 was used for statistical analysis of data. Count data were described as frequency. Measurement data were described as mean ± standard deviation (x ± SD) and percentage (%). The scores of age and self-care ability were normally distributed and compared using two independent sample t-tests. Gender, education level, body mass index (BMI), the incidence of fecal water dermatitis, nutrition screening rate, correct positioning rate of the stoma, awareness rate of relevant knowledge of patients, the incidence of basement warping, the incidence of fecal water leakage, and the incidence of stoma basement leakage in the early stage (within 1 h) were compared using the χ2 test, in which the BMI was compared using Fisher’s exact test. P < 0.05 was considered statistically significant.
Results
General data
According to the inclusion and exclusion criteria, the number of patients in the experimental group and the control group was selected by the random number table method; 79 patients with enterostomy in the Department of Anorectal Surgery of Shanxi Provincial People’s Hospital from April to July 2017 were enrolled in this study as the control group. Among these patients, 27 were male, and 52 were female. The patients’ age range was 29–78 years, with an average age of 57.61 ±11.44. A total of 82 patients with enterostomy from January to June in 2019 were enrolled in this study as the experimental group. Among these patients, 38 were male, and 44 were female. These patients’ age range was 29–80 years, with an average age of 57.16 ±10.32. The t test or χ2 test was performed on age, gender, degree of education and BMI between the experimental group and control group; the differences in general data between the two groups were not statistically significant, as shown in Table I. All patients provided signed informed consent.
Table I
Comparison of general data between two groups of patients (cases/%)
Problems of fecal water dermatitis of patients with enterostomy
Field investigation showed that 50.67% of patients with enterostomy had fecal water leakage, which is the main cause of fecal water dermatitis. Through the cause analysis, the following factors were obtained: (1) The screening rate of nutritional risk was only 45.57%. (2) The nutrition intervention time of the dietitian was 72 h, which was 48 h more than that required for consultation. (3) The correct rate of stoma positioning was only 65.82% because the enterostomy therapist completes routine stoma positioning. In emergencies or when the enterostomy therapist is unavailable, the responsible nurse’s positioning is not always accurate, which leads to poor adhesion of the stoma basement. (4) The early detection rate of fecal water leakage was only 4.48%. Due to the thick material and deep color of the traditional stoma basement, it is not easy to find fecal water leakage. (5) The edge warping rate of the stoma basement was 29.8%. (6) The information system is not perfect: the enterostomy information on the existing WeChat public platform is relatively incomplete and cannot meet the needs of patients and their families. This results in patients’ poor self-care ability, with an average score of only 99.5 points.
Data of main outcome indicator
The main outcome indicator was the incidence of fecal water dermatitis. The incidence of fecal water dermatitis was 45.6% before intervention and decreased to 7% after intervention. The difference between the two groups was statistically significant (p < 0.01, Table II).
Secondary outcome indicators
Secondary outcome indicators include the following: nutrition screening rate, correct stoma positioning rate, awareness rate of patients’ knowledge, self-care ability of patients with enterostomy (family members), living quality, self-efficacy, the incidence of basement warping in enterostomy, the incidence of fecal water leakage, and the leakage rate of the stoma basement in the early stages (within 1 h). The differences between the two groups were statistically significant (p < 0.01, Tables III and IV).
Table III
Comparison of secondary outcome indicators between the two groups (cases/%)
Table IV
Comparison of secondary outcome indicators between the two groups (cases/%)
Discussion
Nurse-led multidisciplinary cooperation is important in the management of fecal dermatitis in enterostomy patients
The multidisciplinary team implemented standard, individualized, and fully comprehensive process management to patients with enterostomy, and then found fecal water leakage of enterostomy patients and conducted effective protection, which could reduce occurrence of fecal dermatitis. Currently, some researchers in China use the cluster care mode for enterostomy patients [18], but most of the hospitals are still at the starting stage of managing enterostomy patients, so they lack scientific and reasonable management in clinical practice. Before establishing the multidisciplinary team, nurses always took care of the colostomy with their knowledge and each department lacked effective communication. Also, most of the nurses took care of the enterostomy patients by depending on their nursing experience or following the doctors’ advice, so there are still some gaps to fill to achieve comprehensive care. Therefore, it is necessary to have a multidisciplinary team that can provide high-quality standard management [19]. While doctors have been dominant in most of the multidisciplinary teams rather than nurses, who have less decision-making authority, the nurse-led multidisciplinary team conforms to the trend of medical development and it would promote communication and cooperation among disciplines, reduce risks and potential hazards, and avoid the drawbacks of the traditional mode [20, 21]. Ostomy nurses have absolute advantages at managing enterostomy patients and can follow up the patients’ situation after they are discharged from the hospital, so it is more advantageous to let a nurse-led team implement this study.
This study introduced the concept of multidisciplinary team cooperation, and it used the nurse-led team as a hub, linking multiple departments and establishing a multidisciplinary cooperation management mode for patients with enterostomy as the focus. In the whole process, the multidisciplinary team was responsible for the patients’ hospital admission, before surgery, after surgery, discharge from hospital, and follow-up visits. They also had a deep understanding and dynamic assessment of, and immediate intervention in, the patients’ condition. With the nurse-led team dealing with hospital admission and nutritional screening during surgery, it was effective to shorten the timing for the dietary nutritionist, so that patients could get effective treatment as early as possible after the doctor in charge made a normative treating plan based on the nutritional assessment. According to Ayik et al. [22], with nurses’ care and follow-up procedures for enterostomy patients, there was an effective reduction in complicating disease occurrence rate. The multidisciplinary team performed standard, individualized, and comprehensive process management for every enterotomy patient, and cooperated with Yuanli Guo et al. as a multidisciplinary team. They obtained good study results during the process in the practice of improving the nutrition of patients with dysphagia after stroke. Nursing played a crucial role in managing enterostomy patients. Therefore, it emphasized once again that a nurse-led team would be more favorable to implement the study, and it is also a reliable assurance for enterostomy patients.
Feasibility analysis of nurse-led multidisciplinary cooperation in the management of fecal dermatitis in enterostomy patients
According to Luo et al. [23], the occurrence rate of fecal dermatitis decreased through the nursing intervention, which is consistent with the results of this study. It developed a “multidisciplinary prevention process of fecal dermatitis in enterostomy patients” according to the evidence-based results, which is a more scientific method as it provides patients with intelligent, informative, and fully processed multidisciplinary management through establishing a nurse-led multidisciplinary enterostomy management team. After carrying out nurse-led multidisciplinary cooperation, there is a significant difference in leading and secondary indicators compared to the results before establishing a multidisciplinary team. Both indicators have statistical significance (p < 0.01). The use of the stoma basement allows for the timely replacement of the stoma basement when fecal leakage is detected at an early stage (within 1 h), thus shortening the time of fecal irritation of the skin and ultimately enabling early screening for fecal dermatitis. Also it provided the most effective protection against fecal water leakage. Through the intervention of nurse-led multidisciplinary cooperation, enterostomy patients not only improved their standard of living but also enhanced their self-efficiency and confidence in triumphing over the disease. Thus, it is feasible to establish nurse-led multidisciplinary cooperation for the treatment and nursing of patients with enterostomy.
Nurse-led multidisciplinary cooperation in the management of fecal dermatitis in patients with enterostomy promotes the development of nursing specialization
One important measurement index of professional nursing standards is the rapid development of clinical nursing specialization. Enterostomy specialized nursing in western countries was developed earlier than that in China and gradually became standardized. However, with the change of the disease spectrum, many complications have been occurring, so it is more challenging to deal with difficult enterostomy, which is also an important research project that researchers and specialized nurses have been working on in some countries [24]. It is more meaningful to prevent fecal dermatitis from happening in enterostomy patients compared to treatments. Severe cases often relate to specialization such as nutrition, medicine, infection, and other problems. Usually, these patients are a high-risk group within whom fecal dermatitis may occur, so linking multiple disciplines together to achieve our goals is the number one priority to prevent and treat fecal dermatitis [25]. The rate of increase to educate specialized enterostomy nurses is much slower than the rate of increase in number of patients, which restricts enterostomy nursing and causes many other issues [26]. It is a great opportunity to establish an advanced and specialized team if medical resources can be coordinated, further optimized, joint consultation and inspection can be developed, and the urgent treatment, nursing, and recovery can be combined. The establishment of a nurse-led multidiscipline mode provides us with a platform that we need. From start to end, the nurse-led multidisciplinary team provides nursing and monitoring during a hospital stay, also adjusts the nursing plan dynamically, and tracks the condition of patients requiring continued nursing services, which can increase patients’ confidence, and deliver the smooth transition from hospital to home. These are the current and future goals that require all medical staff to join their efforts to achieve them.