Introduction
The life expectancy of human immunodeficiency virus (HIV)-infected people has significantly increased with highly active antiretroviral therapy [1]. However, among these individuals, there is a high likelihood of coinfections such as viral hepatitis and syphilis that share similar transmission routes with HIV, and these factors may adversely affect the course of the disease in the long term [2, 3]. In co-infected patients with hepatitis B virus (HBV) or hepatitis C virus (HCV), antiretroviral therapy-related hepatotoxicity may lead to the progression of liver damage [4, 5]. Therefore, chronic liver infections are among the most important causes of hospitalization and death among HIV-infected people today [6–8]. Syphilis, as another common infectious disease in the same group of people, serves as the gateway to HIV by causing ulcerative genital lesions. Syphilis may also facilitate HIV transmission by activating immune cells and increasing viral load. On the other hand, HIV infection may adversely affect the natural course of clinical manifestations and response to syphilis treatment [9–11]. Therefore; serological markers of viral hepatitis and syphilis should be investigated in terms of coinfections in HIV-infected people in order to select the appropriate treatment [12]. This study aimed to determine the seroprevalence of hepatitis A virus (HAV), HBV, HCV, and syphilis among HIV-infected people followed up at a university hospital at the initial stage of diagnosis.
Material and methods
A retrospective evaluation was made among HIV-infected people followed up at Ondokuz Mayis University Faculty of Medicine, Department of Infectious Diseases and Clinical Microbiology, Samsun, Turkey, between 2005 and 2018. Within the specified study period, 336 patients aged 18 years and older who were confirmed for HIV infection were evaluated in terms of initial serological markers for viral hepatitis (hepatitis B surface antigen [HBsAg], antibody to HBs antigen [anti-HBs], antibody to HCV [anti-HCV], total antibody to hepatitis B core antigen [anti-HBc total], total antibody to hepatitis A virus [anti-HAV total]) and syphilis (rapid plasma reagin [RPR] and Treponema pallidum hemagglutination [TPHA]). Isolated anti-HBc total positivity was defined as the presence of anti-HBc total in absence of any other serological markers of HBV infection.
An automated electrochemiluminescent immunoassay method (Cobas e411, Roche Diagnostics) was used to detect serologic markers of HIV, HAV, HBV and HCV infections during the study period. HIV-1 RNA, HBV DNA and HCV RNA levels were determined when necessary by real time-polymerase chain reaction (RT-PCR) using commercial kits (COBAS AmpliPrep/COBAS TaqMan HIV-1Test, COBAS AmpliPrep/COBAS TaqMan HBV Test, and COBAS AmpliPrep/COBAS TaqMan HCV Quantitative Test).
Definitive diagnosis of HIV infection was considered as reactive human immunodeficiency virus 1/2 antigen/antibodies (HIV 1/2 Ag/Ab) verified with a confirmatory method (Western blot, line immunoassay or indirect immunofluorescence) at a central public health laboratory. Serum RPR (Rapid labs, Great Britain) and TPHA (Plasmatec, United Kingdom) kits were used for syphilis and TPHA positivity (with positive or negative RPR) was considered as exposure to Treponema pallidum.
Results
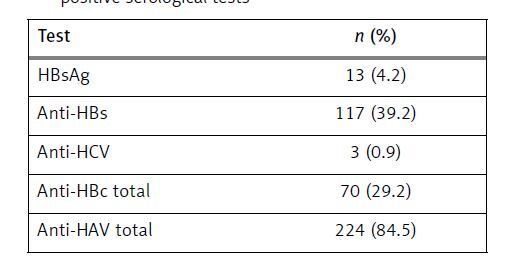
Between 2005 and 2018, 336 HIV-infected people were followed up in our clinic. Of these, 284 (84.5%) were male. The mean age at diagnosis was 39.02 years. HBsAg was positive in 13 (4.2%) of 303 patients, anti-HBs in 117 (39.2%) of 298 patients, anti-HCV in 3 (0.9%) of 301 patients, anti-HBc total in 70 (29.2%) of 239 patients and anti-HAV total in 224 (84.5%) of 265 patients. HCV ribonucleic acid (RNA) was confirmed positive (20 100 000 IU/ml) in 1 of the 3 patients positive for anti-HCV (Table I).
Table I
Number (n) and ratio (%) of patients with positive serological tests
| Test | n (%) |
|---|---|
| HBsAg | 13 (4.2) |
| Anti-HBs | 117 (39.2) |
| Anti-HCV | 3 (0.9) |
| Anti-HBc total | 70 (29.2) |
| Anti-HAV total | 224 (84.5) |
Isolated anti-HBc total positivity was present in 12 (5%) of the patients with anti-HBc total positivity. Eight of the patients with isolated anti-HBc total positivity were studied for HBV deoxyribonucleic acid (DNA) and HBV DNA was detected (116 IU/ml) in 1 (12.5%) of these patients.
Of the 224 patients examined for syphilis by RPR, results of 37 patients (16.5%) were reported as positive and 4 (1.7%) were reported as the gray zone. Of the 37 patients who were positive for RPR, TPHA was positive in 34 (91.8%), gray zone in 2 (4%) and negative in 1 (3.3%) patient. The TPHA results of 4 patients whose RPR test was reported to be in the gray zone were positive in 1 patient, gray zone in 2 patients and negative in 1 patient. Generally, of the 224 patients screened for syphilis, 35 (15.6%) had a positive TPHA confirmation test at the first screening tests.
Discussion
In our study, HBsAg seroprevalence was found to be 4.2%, while anti-HBc total and anti-HCV seroprevalences were 29.2% and 0.9%, respectively. Although the prevalence of coinfections varies according to the epidemiology of the disease, it is estimated that approximately 10% of HIV-infected people worldwide are co-infected with HBV and the prevalence of coinfection may be as high as 25% in countries in Asia and Africa, which are endemic for chronic hepatitis B [13, 14]. In terms of the prevalence of chronic HBV infection, Turkey is in the moderately endemic group, similar to the other Mediterranean and Middle Eastern countries, and HBsAg positivity is reported to be around 4% in the normal population [15–17]. Although studies have reported some regional differences, anti-HCV seroprevalence in the general population has been reported to be between 0.4% to 1.5% in Turkey [18–21]. In a global meta-analysis evaluating HCV co-infections among HIV-infected people, the mean HCV seroprevalence was found to be 6.2%, while prevalence was 27% in eastern Europe and central Asia, where intravenous drug use was the main source of transmission for HIV [22]. Among 949 HIV-infected people from Istanbul, Turkey, HBsAg and anti-HCV seroprevalences were determined as 6.2% and 0.9%, respectively [23]. In another study evaluating serological data of 3,896 HIV-infected people across Turkey, HBV and HCV co-infections were reported as 3.2% and 0.5%, respectively [24]. Serological prevalence rates obtained in our study showed similarities with chronic viral hepatitis infection rates among the general population and other HIV-infected people in Turkey. In countries where higher seroprevalence rates for chronic viral hepatitis have been reported among HIV-infected people, this situation is often attributed to higher rates of intravenous drug usage. HIV is mainly transmitted sexually and intravenous drug use rates are low among HIV-infected people, as in the general population in Turkey [25–27].
In our study, 39.2% of HIV-infected people had antibodies to HBV and 84.5% to HAV. In this case, more than half of the diagnosed individuals were found to be susceptible to HBV. HAV seropositivity is up to 90% in adulthood in Turkey, which is similar to the seropositivity results of HIV-infected people in our study [28]. HIV-infected people should be vaccinated against HBV, as HBV co-infection causes a higher risk of cirrhosis and hepatocarcinoma. Also, the viral load is higher during HAV infection, and the duration of viremia is prolonged with simultaneous fecal excretion [29, 30]. While both the Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO) recommend vaccination against HAV if any other medical, behavioral, epidemiological or occupational condition is added to the HIV infection, the Turkish Ministry of Health recommends the implementation of the HAV vaccine to all HIV-infected people susceptible to HAV infection [31–33].
In our study, isolated anti-HBc total positivity was detected in 12 (5%) patients, of whom HBV DNA was detected in 1 (12.5%) of 8 patients who were evaluated by a molecular test. The prevalence of isolated anti-HBc total positivity varies between 1% and 30% in different populations depending on the endemics of HBV [34–36]. Isolated anti-HBc total positivity was found to be between 1.8 and 5% in the studies conducted in the general population in our country, which is similar to the HBsAg seropositivity rate in the population [37–39]. Isolated anti-HBc total positivity is a common serological pattern in HIV-infected people. Studies published in different regions have reported that the prevalence of isolated anti-HBc total in HIV-infected people is between 10.6% and 45%, and the prevalence of occult infection with intermittent viremia has been reported to range from 0% to 89.5% [40–43]. Two studies conducted among HIV-infected people from Turkey determined the isolated anti-HBc total positivity as 2.8% and 13.5%, and occult HBV infection as 100% and 10.3%, respectively [12, 44]. Although the prevalence of isolated anti-HBc total positivity and occult HBV infection rates obtained in our study have shown similarities with the data obtained from Turkey and with other national prevalence study results, rates have generally a very wide range because of the limited number of patients. Therefore, it is not appropriate to generalize the results, and studies conducted with higher numbers of patients are needed.
Of 224 patients who were examined for syphilis, 34 (15.1%) patients were positive for TPHA. Syphilis and HIV have similar routes of transmission and the same risk factors. Sex workers, intravenous drug users, men who have sex with men, those with a history of sexually transmitted diseases and people with multiple partners have a higher risk of acquiring HIV, syphilis and other sexually transmitted diseases [45]. Syphilis coinfection rates in HIV-infected people are in the range 2–43% in Europe and 1–21% in North America [46]. While syphilis prevalence in the general population in Turkey is between 0% and 0.46%, it is has been reported between 8.7% to 31.6% among transgenders and sex workers [47–50]. The seroprevalence of syphilis in HIV-infected people from Turkey has been found in two studies as 8% and 9.8% [51, 52]. In our study, the prevalence of syphilis was significantly higher than the prevalence in the general population but was similar to the domestic and international prevalences with similar patient groups. As the risk factors (occupation, number of partners, sexual orientation) of HIV-infected people in the patient group may be different in global and local studies, prevalence of syphilis may be affected by this variables [53].
In conclusion, in 2018, a total of 6519 people were newly diagnosed with HIV from the 15 countries in the Centre of the WHO European Region, giving a rate of 3.3 per 100 000 population. The highest rates (> 3.0) were reported by Cyprus (9.0), Bulgaria (4.4), Turkey (3.9), Montenegro (3.7), Albania (3.5), Romania (3.4) and Poland (3.1) [54]. With the increasing number of patients, surveillance is important for newly diagnosed patients in terms of the frequency of sexually transmitted diseases such as viral hepatitis and syphilis.
In the study conducted in our center, a high seroprevalence rate of syphilis and low rate of immunity to HBV were detected. Screening of infection agents such as HAV, HBV, HCV, and syphilis among HIV-infected people in the initial period of diagnosis is important in preventing the negative effects of coinfections on the course of the disease and provides the chance of protection in people who are susceptible to HAV and HBV by vaccination.
In addition, our findings have shown that HIV infection should be considered in patients newly diagnosed with syphilis, which is detected at a higher rate in HIV-infected people compared to the general population; in this way early detection and treatment can prevent HIV transmission as well as syphilis.
Therefore, health care facilities that follow up HIV-infected people should determine the serological profiles of their patients initially once the patients are diagnosed.