Introduction
Based on prevalence studies, Slovakia is among countries with a high risk of cardiovascular (CV) disease (CVD), mortality, and morbidity. The annual incidence of CV mortality is 209.5 females and 333.8 males per 100 000 inhabitants [1]. Despite advances in both primary and secondary prevention, the decline in CV mortality is minimal. This is in marked contrast to the significant improvement in inpatient care of patients with acute CV events. This contradiction can be explained by inadequate control of risk factors in post-hospital, outpatient, and home settings [2]. One key factor is lipid profile control. However, the question remains as to where we stand in achieving target levels in the real population.
Dyslipidaemia is one of the major risk factors leading to the development of atherosclerotic cardiovascular disease (ACVD). When not treated properly, dyslipidaemia leads to ischaemic complications depending on the location [3, 4]. The relationship between low-density lipoprotein-cholesterol (LDL-C) levels and the risk of major cardiovascular events is now clearly demonstrated by medical evidence. The reduction in the relative risk of ACVD is proportional to the absolute reduction of LDL-C and is not dependent on any particular treatment modality [5]. A significant decrease in LDL-C leads to the stabilisation of atherosclerotic lesions. Using intravascular ultrasound, some studies have shown that plaque regression can be observed thanks to either intensified statin [6], or anti-PCSK9 therapy [7]. Taking these findings into account, recent EAS/ESC recommendations have tightened LDL target levels. For high-risk patients, a 50% reduction in LDL from baseline is recommended in addition to target levels of 1.4 mmol/l LDL-C.
This study aimed to retrospectively analyse an extensive amount of anonymised LDLC values in individual populations of very high cardiovascular risk patients (as defined by guidelines). Another aim was to determine the proportion of patients achieving LDL-C target values based on the recommendations in place at the time of each year of follow-up.
Material and methods
Study design
This study was conducted as a retrospective analysis of large, anonymized data of LDL-C values of patients examined in outpatient and inpatient care throughout Slovakia. The data were obtained by InovaHealth from records of laboratory tests provided by MEDIREX Group. The data used in this study covered a three-year time interval between 2017 and 2019. This is the period in which the ESC/EAS 2016 guideline recommendations were in effect, and the second half of 2019 was based on the 2019 guidelines. The data were without regional or centre specificity. The data were processed in anonymised form with the consent of both Novartis Slovakia Ltd and InovaHealth. After the initial selection of suitable patients based on diagnoses that clearly showed very high CV risk, all LDL-C measurements of such identified patients from 2017 to 2019 were gathered, regardless of the diagnosis code at the time of LDL-C measurement. Patients were stratified by LDL-C values into the following intervals for better monitoring of LDL-C levels: < 1.4 mmol/l (< 55 mg/dl); 1.4 (inclusive) – 1.8 mmol/l (55–70 mg/dl); 1.8 (inclusive) – 2.6 mmol/l (70–100 mg/dl); 2.6 (inclusive) – 3.0 mmol/l (100–115 mg/dl), 3.0 (inclusive) – 3.5 mmol/l (115–135.34 mg/dl), 3.5 (inclusive) – 4.0 mmol/l (135–155 mg/dl), 4.0 (inclusive) – 4.9 mmol/l (155–190 mg/dl), above 4.9 mmol/l (above 190 mg/dl).
Eligibility criteria
Patients enrolled in this study were men and women of all ages but not younger than 18 years, meeting the definition of very high CV risk based on ESC/EAS [5]. Patients were included based on reported International Classification of Diseases (ICD) diagnoses.
The following groups of patients with very high CV risk were analysed:
– Group 1: patients who in 2017 had a laboratory test with any of the diagnoses I20.0, I21, or I22 (history of ACS) and had at least one LDL-C test done in 2016.
– Group 2: patients who in 2017 had a laboratory test with any of the diagnoses I63.5, I63.8, and I63.9 (history of stroke) and at least one LDL-C test in 2016.
– Group 3: patients who had any of the diagnoses I20.0, I21, I22, I25, I63.5, I63.8, and I63.9 on any laboratory test during 2017–2019 (this was the set of patients with a history of ACS, stroke and CCS) and had at least one LDL test during 2017–2019 at the same time.
Statistical analysis
Descriptive statistics and methods designed to test statistical hypotheses were used to process the results. For categorical variables, the number and percentage of patients in each group are reported. To follow the dynamics of LDL-C in 2017–2019, patients with at least one LDL-C measurement in each year were included in the statistical analysis. Differences in the LDL-C values between the years in certain groups of patients were analysed by repeated measures of ANOVA Tukey post-hoc tests. In the analyses of LDL-C by age, the age of the patient as of 1 January 2019 was taken. Values of p < 0.05 were considered statistically significant. Attainment of target LDL-C values was calculated as a % value, including only the patients with an available LDL measurement in each year of the study.
Results
Patients’ characteristics
In total, 72 039 eligible patients were enrolled from all the participating outpatient clinics and hospitals together with 220 657 LDL-C medical records. On average, each patient had 3.06 LDL-C tests done during the study period. Based on the protocol, we divided patients into groups based on CV disease type and then selected subgroups of patients with LDL-C measurement in each year of follow-up.
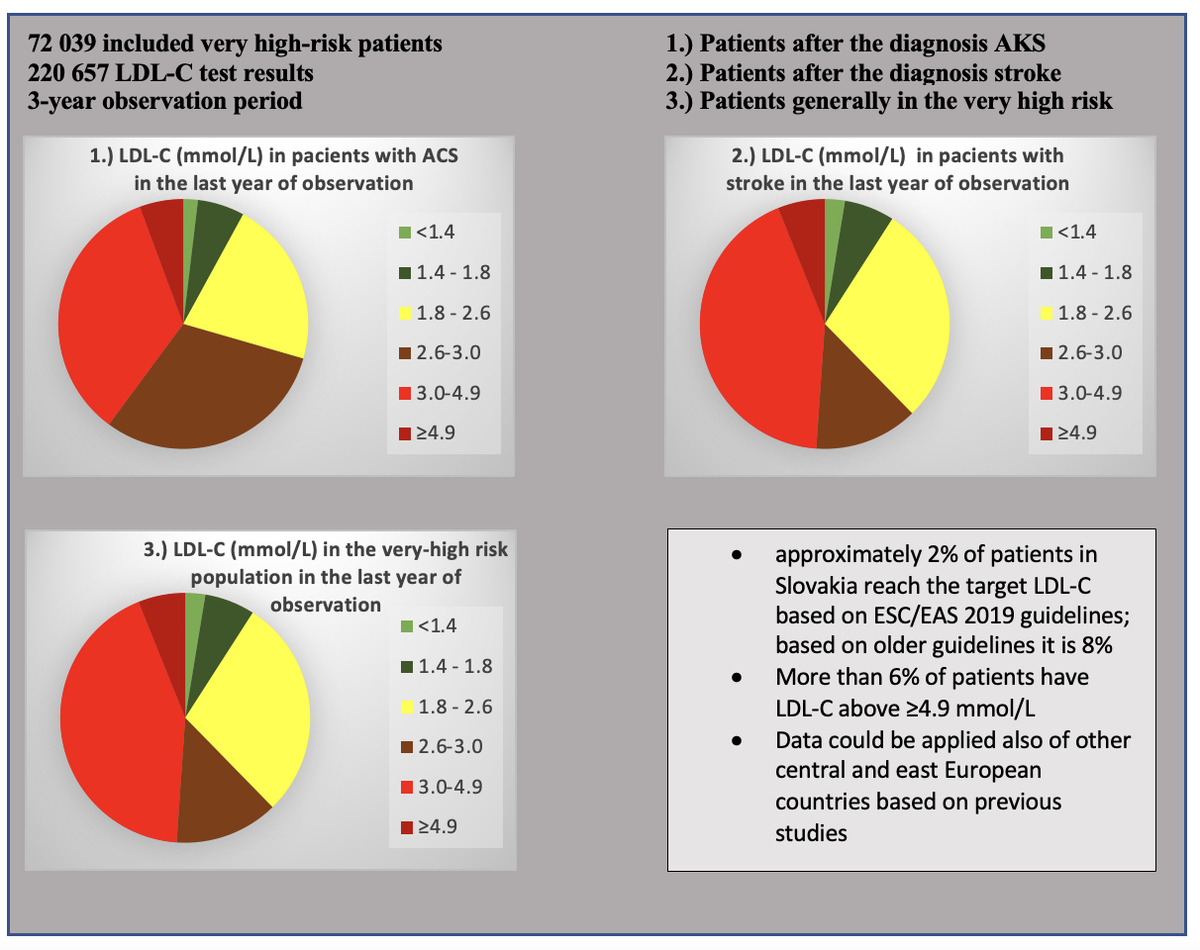
The group of patients with diagnosed acute coronary syndrome (ACS) included N = 1366 patients with a total of 5897 LDL-C values, with an average of 4.3 measurements per patient over the entire study period and with an average LDL-C in the years 2017, 2018, 2019 of 2.94, 2.84, 2.84 mmol/l, respectively (Figure 1, Table I). LDL-C levels decreased significantly (p = 0.007) in 2018 in comparison with the year 2017, and in 2019 in comparison with 2017 (p = 0.012). Between the years 2018 and 2019, no significant change was observed (p = 0.99) (Figure 1, Table I). The group with diagnosed stroke included N = 527 patients and a total of 1905 LDL-C values, with an average of 3.6 measurements per patient over the entire study period and with an average LDL-C in the years 2017, 2018, 2019 of 3.01, 2.79, 2.88 mmol/l, respectively. LDL-C levels decreased significantly (p = 0.0005) in 2018 in comparison with the year 2017. Between the years 2018 vs. 2019 and 2017 vs. 2019 no significant change was observed (p = 0.357; 0.088) (Figure 2, Table I). The overall group of patients meeting the criteria for very high CV risk included patients with a history of ACS and/or stroke, as well as patients with a chronic coronary syndrome diagnosis based on ESC definitions. A total of N = 72 039 patients with 220 657 LDL-C measurements were included in this group, with an average of 3.1 results per patient over the entire study period. The mean LDL-C values in this group over the study period were 3.30, 3.21, 3.18 mmol/l. LDL-C levels decreased significantly (p < 0.0001) in 2018 in comparison with the year 2017, and in 2019 in comparison with 2017 (p < 0.0001). Between the years 2018 and 2019, no significant change was observed (p = 0.99) (Figure 3; Table I).
Figure 1
Mean LDL-C concentrations in ACS patients in different years after the initial diagnosis from all the obtained data from all specialists
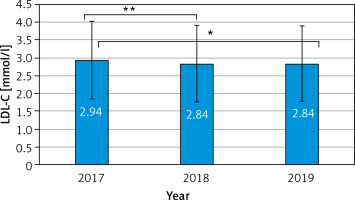
Figure 2
Mean LDL-C concentrations in stroke patients in different years after the initial diagnosis from all the obtained data from all specialists
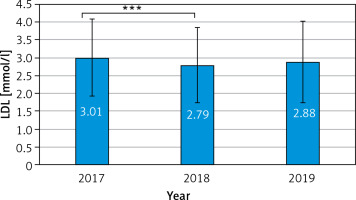
Figure 3
Mean LDL-C concentrations of patients in group 3 in each year after the initial diagnosis from all the obtained data from all specialists
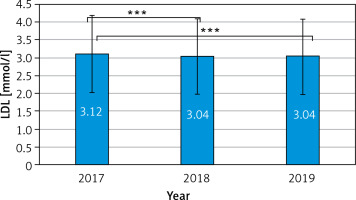
Table I
Characteristics of each study group
Attainment of the 2016 European Society of Cardiology/European Atherosclerosis Society guideline-recommended LDL-C targets
In the subgroup of acute coronary syndrome (ACS) patients with LDL-C tests done each year (n = 683), we found that only 6.9% (95% CI: 5.1–9.1), 8.9% (95% CI: 6.9–11.3), and 8.5% (95% CI: 6.5–10.8) met the 2016 EAS/ESC-based LDL-C targets of LDL-C < 1.8 mmol/l (< 70 mg/dl) in 2017, 2018, and 2019, respectively (Table II, Figure 4). In each year of follow-up, the largest proportion consisted of ACS patients with measured LDL-C levels between 1.8 and 2.6 mmol/l (70–100 mg/dl). At the same time, the proportion of these patients is increasing year by year. Over the 3 years (2017–2019), the patients who had high (≥ 4.9 mmol/l; ≥ 190 mg/dl) or higher (3.0–4.9 mmol/l; 115–190 mg/dl) measured LDL-C values at baseline (year 2017) were the most successful in lowering LDL-C (Figure 5). Among patients with stroke and an LDL-C test done each year (n = 231), only 7.8% (95% CI: 4.7–12.0), 8.7% (95% CI: 5.4–13.1), and 9.1% (95% CI: 5.7–13.6) of patients met the target LDL-C values based on EAS/ESC 2016, 2017, 2018, and 2019, respectively (Table II, Figure 5). Patients in the very high CV risk group with an LDL-C test every year (n = 23 491) had target values achieved in only 5.4% (95% CI: 5.1–5.7), 6.0% (95% CI: 5.7–6.4), and 6.6% (95% CI: 6.3–6.9) of cases in each year of follow-up (Table II, Figure 6).
Figure 4
Attainment of target LDL-C (mmol/l) values in 2017–2019 in the ACS subgroup of patients with LDL-C tests done each year (n = 683)
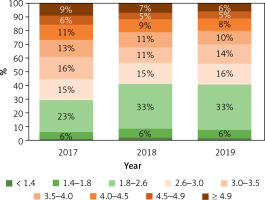
Figure 5
Attainment of target LDL-C (mmol/l) values in 2017–2019 in group 2, in patients with dg. stroke with at least one examination in each year (n = 231)
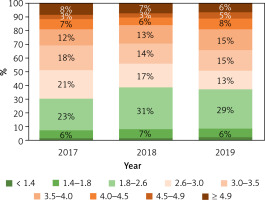
Figure 6
Attainment of target LDL-C values (mmol/l) between years 2017–2019 in group 3, patients at very high CV risk, the subgroup of patients with LDL-C test done each year (n = 23 491)
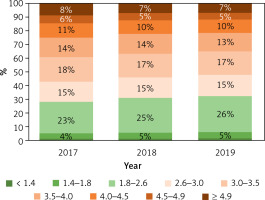
Table II
Parameters monitored in individual patient groups with LDL measurement in each year
Attainment of the 2019 European Society of Cardiology/European Atherosclerosis Society guideline-recommended LDL-C targets
When analysing the data again using the new EAS/ESC 2019 recommendations, namely LDL-C < 1.4 mmol/l (< 55 mg/dl), the target levels in the general population of patients at very high CV risk are only 1.1% (95% CI: 0.9–1.2), 1.3% (95% CI: 1.2–1.5), 1.6% (95% CI: 1.4–1.8) in years 2017, 2018, and 2019, respectively. For patients with ACS, this was 1.2% (95% CI: 0.5–2.3), 2.5% (95% CI: 1.5–4.0), and 2.1% (95% CI: 1.1–3.4) of patients in 2017, 2018, and 2019, respectively. For patients in the stroke diagnosis group, LDL-C target levels were achieved by only 1.7% (95% CI: 0.5–4.4), 1.7% (95% CI: 0.5–4.4), and 2.6% (95% CI: 1.0–5.6) of patients in the years 2017, 2018, 2019, respectively (Table III).
Table III
Attainment of target LDL-C in the mentioned observational studies (more details, selection criteria in the text and in the mentioned publications [16, 18–23, 32])
| Study | Country | Number of observed patients | Attainment of target LDL-C valid in the years of the study |
|---|---|---|---|
| SlovakLipid | Slovakia | 72 039 | 5% |
| EUROASPIRE IV [16] | 24 European countries | 16 426 | 19.5% |
| DYSIS II [18] | Belgium, France, Germany, Greece, Ireland, Italy Russia | 880 ACS and 2778 CHD | ACS 23.2% CCS 29.6% |
| EUROASPIRE V [19] | 27 countries in Europe | 7824 | 30% |
| EPHESUS study [20] | Turkey | 1868 | 18% |
| [21] | Germany | 25 848 (ASCVD group) | 8.5% |
| SAFEHEART [22] | Spain | 4132 (HeFH) | 11.2% |
| DA VINCI study [23] | 14 European countries | 9602 | 54% in primary prevention and 30% ASCVD (2016 guidelines) 33% in primary prevention, 18% with ASCVD (2019 guidelines) |
| DA VINCI study CEE [32] | Central and Eastern Europe (Czech Republic, Hungary, Poland, Romania, Slovakia, Ukraine | 2154 | 60% in primary prevention and 31% in secondary prevention (2016 guidelines) 37% in primary prevention and 13% in secondary prevention (2019 guidelines) |
Discussion
Globally, elevated levels of cholesterol and atherogenic lipoproteins are estimated to cause 2.6 million deaths per year and 29.7 million cases of decreased quality of life. Overall, up to 39% of women and 37% of men are thought to have total cholesterol levels above 5.0 mmol/l [8, 9]. Large observational studies have shown that each 1 mmol/l LDL-C reduction leads to a 20–25% reduction in overall CV risk and a 20% reduction in coronary mortality [9, 10].
Numerous international studies have been carried out to assess the rate of attainment of target levels based on recommendations [11–13]. Most studies have focused on patients at very high and high CV risk. Some have looked at recommendations’ adherence and guideline patterns in very high-risk patients, such as those who have had a previous MI [14]. The EUROASPIRE study examined primary and secondary prevention practices in patients diagnosed with coronary heart disease in Europe between 1995 and 1996, which had several follow-ups [15]. In EUROASPIRE IV from 2016, only 19.5% of patients with coronary artery disease had LDL-C levels below 1.8 mmol/l (70 mg/dl) [16]. Another study called the Dyslipidemia International Study (DYSIS) evaluated lipid abnormalities in relation to chronic statin therapy [17]. The first international dyslipidaemia study (DYSIS I), similarly to EUROASPIRE, found poor target attainment in very high-risk patients across Europe, ranging from high values of 38.3% for the United Kingdom (UK) to low values of 9.2% for Greece [18]. The DYSIS II study showed that only 29.4% of patients with stable coronary artery disease achieved LDL target values below 1.8 mmol/l (70 mg/dl), and only 18.9% of patients with ACS achieved target LDL values [1]. The most recent survey (EUROASPIRE V) reports that target LDL-C < 1.8 mmol/l (70 mg/dl) was attained in less than 30% of patients surveyed. This percentage was slightly higher among patients on high intensity hypolipaemic therapy [19]. A recent sub-analysis from the EPHESUS study, a cross-sectional Turkish registry that enrolled patients with atherosclerotic disease, showed attainment of LDL-C targets in only 18% of cases [20]. LDL-C target attainment was even lower in a German cohort of patients with recent acute coronary syndrome enrolled in a retrospective registry. In this cohort, only 8.5% of patients with ASCVD achieved target levels [21]. Data from the SAFEHEART registry in Spain showed that only 11.2% of patients with familial hypercholesterolaemia (FH) achieved target LDL-C levels [22]. The DA VINCI study [23] described the success of achieving LDL-C target values and the most used hypolipaemic agents. It was a cross-sectional observational study conducted in 18 countries including Slovakia with patients undergoing hypolipaemic therapy as part of primary or secondary prevention. Only about half (54%) of all patients achieved target values based on the 2016 primary prevention recommendations. For patients with ASCVD, this was only 30%. When applying the 2019 recommendations, only one-third (33%) of patients in primary prevention and only 18% with ASCVD reached target values [23]. The main pillar of CV disease prevention is risk factor modification. Based on the results of the IMPACT model, decreasing cholesterol is the most significant [24–26]. In Slovakia, compared to countries such as Poland, Hungary, the Czech Republic or Austria, this benefit is not fully utilised [27].
This retrospective study aimed to determine the attainment of recommended LDL-C levels in patients at very high risk, where proper management of risk factors is critical for the prevention of first or recurrent CV events. The analysis used data from 2017 to 2019, during which the 2016 ESC/EAS recommendations were in force [27]. Based on these recommendations, patients with documented cardiovascular disease, whether in the form of ACS, coronary revascularization (percutaneous coronary intervention (PCI), coronary artery bypass graft (CABG), or other arterial revascularization procedures), stroke, transient ischaemic attack (TIA), or peripheral arterial disease (PAD), are at very high cardiovascular risk. Previous studies have already pointed to the low degree of attainment of target LDL-C levels. The Dyslipidemia International Study (DYSIS I) Slovakia showed that the situation in attaining target LDL-C values in Slovakia is dire [28, 29]. Among patients at very high CV risk, only 16.7% achieved the LDL-C ≤ 1.80 mmol/l target value (previous guidelines were in effect). Only 44.7% of subjects with documented CV disease had LDL-C between 1.81 and 2.90 mmol/l. Despite the existence of statin therapy and its widespread use, many patients still do not reach the target values. Similar results were obtained in the DYSIS II study, where target levels for very high cardiovascular risk (LDL-C ≤ 1.80 mmol/l, according to previous guidelines) were achieved by only 18.6% of patients [2]. Such a small percentage is alarming, but in line with data from abroad. In the international DYSIS II study only 29.4% of patients achieved the target of ≤ 1.8 mmol/l LDL-C [1].
In our study, the results are even more disturbing. Among patients diagnosed with ACS, only 7–8% of patients achieved target LDL-C levels ≤ 1.80 mmol/l in each year of follow-up. Patients with stroke had similar values, at 8–9%. When we included patients based only on the general ESC/EAS criteria for very high CV risk, these values were even lower, at only 7%. We hypothesized that group 3, that is patients generally at very high CV risk, also included patients with manifested/diagnosed CCS. In these patients, LDL-C levels were not adequately controlled. In contrast, extremely high LDL-C levels above ≥ 4.9 mmol/l were present on average in 6–9% of patients at very high CV risk. The new 2019 ESC/EAS recommendations [5] have brought stricter target values and focused attention on intensified and combination hypolipaemic therapy. An important role was attributed to the results of meta-analyses confirming the dose-dependent reduction in ASCVD with LDL-C-lowering agents; the greater the absolute reduction in LDL-C, the greater the reduction in CV risk [5]. The benefits associated with LDL-C reduction are not specific only to statin therapy [30]. Furthermore, based on recent recommendations no lowest LDL-C level has been identified at which the risk outweighs the benefits. When re-analysing the data based on the latest recommendations, we arrive at an alarmingly low portion of patients (1–3%) who attain LDL-C target values of ≤ 1.40 mmol/l. However, this analysis is limited in part by the fact that older recommendations were still in effect in 2017, 2018, and up to September of 2019, so the data predicting success in achieving the target LDL-C according to the current guidelines need to be considered cautiously. Furthermore, the new recommendations dictate at least 50% reduction in LDL-C levels from baseline in addition to the overall decrease of ≤ 1.40 mmol/l. There has been a long-standing tendency in Slovakia to not prescribe the maximum tolerated dose of statins or combination therapy, especially in the outpatient setting. The need to educate outpatient physicians in proper therapy utilisation, as well as the use of the latest therapeutic approaches, is now even more essential [31]. This tendency was also confirmed in our study, where we monitored whether the changes in LDL-C in individual years were significant. During the follow-up, we found that a significant decrease in LDL-C occurred in the second year of follow-up and this decrease was not significant in the next year. Moreover, group 3 showed a slight increase. This also confirms the hypothesis that patients are initially administered more aggressive therapy in hospital settings or by specialists/cardiologists, but during outpatient management this therapy is subsequently down-titrated.
Extracting data from the DA VINCI study for Central and Eastern Europe, we find that countries in this region have 60% target attainment in primary prevention based on the 2016 recommendations, 31% in secondary prevention, and 44% overall. Based on the 2019 recommendations, this is 24% overall, 37% in primary prevention and 13% in secondary prevention [32].
These differences between our study and the DA VINCI study [32] may have several explanations. The first is that our study was based on a retrospective analysis of a large data set based on International Classification of Diseases (ICD) diagnoses. The benefit, in this case, is the large number of patients included. The DA VINCI study included 5 888 patients, compared to 72 039 patients in our study. This difference may significantly affect the attainment of target LDL-C levels, as our data are from the whole country, without regional specificity, and without participating centre specificity. Therefore, bias which could be caused by using data from only specialised centres where dyslipidaemia therapy tends to be optimal, and not from outpatient clinics, where dyslipidaemia management may not be ideal, is not present in our dataset.
Our data are more consistent with the results of the recent large Santorini study [33], where it was found that up to 80% of high and very high-risk patients did not reach the target values from the 2019 ESC/EAS guidelines. Contributory factors may include CV risk underestimation and underutilization of combination therapies. Although our study was not aimed at monitoring the types of lipid-lowering therapies, it is generally known that the combined therapy of high-intensity statin and ezetimibe can decrease LDL-C by up to 65%, while the addition of the PCSK9 inhibitor can induce further reduction of up to 85%. Our data suggest that most patients did have optimal medical therapy, but had extremely ineffective lipid-lowering therapy. In regular clinical practice, a patient is discharged after an acute cardiovascular event with a statin in the maximum dose, but a large percentage of patients require subsequent titration, which may be delayed in the outpatient setting, or patients are poorly monitored, and combined therapy is not used [34, 35].
We should follow the general rules highlighted in a recent article [36], stating that earlier and longer therapy is key to better outcomes for patients, and that combination therapy should be used wherever possible. A recent study compared the stepwise approach and upfront combination therapy. Studies have shown that statin and ezetimibe combination therapy is superior to statin monotherapy in terms of significant reduction of all-cause mortality, with an absolute risk reduction of 4.7% after 3 years [35]. Similar results were highlighted in the RACING study, which showed that moderate-intensity statin with ezetimibe combination therapy was not inferior to high-intensity statin monotherapy among patients with ASCVD [37] and had a higher degree of adherence compared to high-dose monotherapy. A certain benefit of early combined and intensified therapy could also be the achievement of LDL-C target values despite delayed visits to an outpatient cardiologist (which is not rare) in the early phases after the initial cardiovascular event.
This study has some limitations which need to be acknowledged. Patients were classified based on their ICD diagnoses, which was the only method whereby patients were classified in the highrisk CV disease group. It is possible that some high-risk patients were not included, or high-risk patients were wrongly classified in the very high-risk group. Also, our study monitors the situation only in Slovakia, which may differ considerably from other central or east European countries. Another limitation of this study is that the data were collected at the time when the 2016 guideline recommendations were in place, and the implementation of the 2019 guidelines is only illustrative, as the data are mostly from the period before September 2019.
Attainment of target LDL-C levels in Slovakia has been previously understudied despite having the highest CVD mortality and high CV risk factor rates compared with the rest of Europe. This study created a large dataset focused only on Slovakia and clearly illustrated the gap between recommended LDL-C goals and LDL-C levels in practice. The latest ESC/EAS recommendations and the results of DYSIS I, II, and our study demonstrate the evident need for new therapeutic approaches and patient management recommendations in preventive cardiology. New and affordable hypolipaemic agents with more favourable administration regimens would significantly improve patient adherence to therapy, improve outpatient management, and thus achieve better control and attainment of target LDL-C levels, reducing the incidence of new CV events.
In conclusion, based on the results of this study, we concluded that patients at very high CV disease risk in Slovakia have poorly controlled atherogenic lipid levels and have LDL-C levels significantly higher than the recommended 1.8 mmol/l LDL-C for protection against adverse CV events, as per the ESC/EAS 2016 recommendations. Fewer than 5–10% of patients achieved the target levels in each risk group, which is significantly lower than the average in other countries globally (29.4%). These patients, despite adequate in-hospital management of ACS, stroke, and other CV diagnoses, remain at high risk and are vulnerable to secondary CV events associated with inadequately controlled hyperlipidaemia. We hypothesize that patients at very high and high CV disease risk would benefit the most from intensified hypolipaemic therapy.