Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
ONCOLOGY / CLINICAL RESEARCH
The role of body mass index and tumor necrosis factor α
in breast cancer development: a case-control study
1
Department of Health Toxicology, School of Public Health, China Medical University (Shenbei Campus), Shenbei New District, Shenyang, Liaoning Province, China
2
School of Medicine, Dentistry and Biomedical Sciences, Queen’s University Belfast, Belfast, Northern Ireland, United Kingdom
3
Community Health Management Center, Shenzhen Pingle Orthopedics Hospital, Pingshan District, Shenzhen City, China
4
Department of Epidemiology, School of Public Health, Sun Yat-sen University (North Campus), Yuexiu District, Guangzhou City, Guangdong Province, China
Submission date: 2025-02-13
Final revision date: 2025-04-18
Acceptance date: 2025-04-26
Online publication date: 2025-06-22
Corresponding author
Zefang Ren
Department of Epidemiology School of Public Health Sun Yat-sen University (North Campus) No. 74, Zhongshan 2nd Road Yuexiu District Guangzhou City Guangdong Province 510080, China
Department of Epidemiology School of Public Health Sun Yat-sen University (North Campus) No. 74, Zhongshan 2nd Road Yuexiu District Guangzhou City Guangdong Province 510080, China
KEYWORDS
TOPICS
ABSTRACT
Introduction:
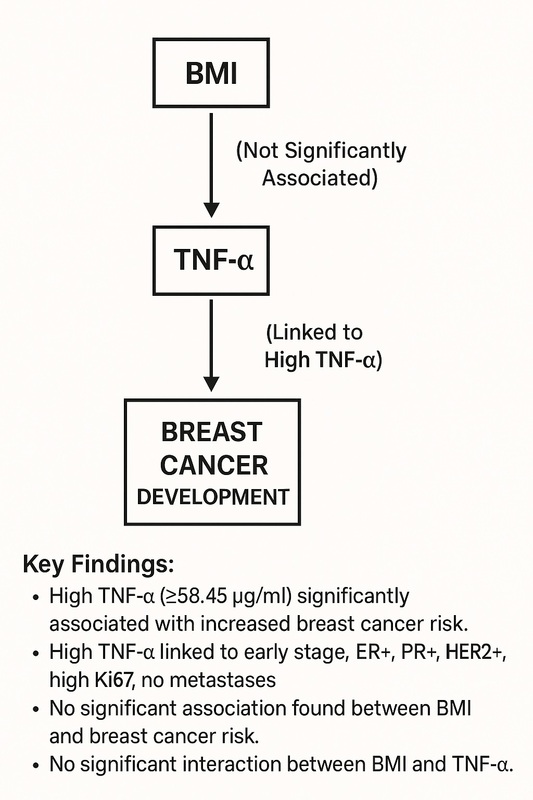
A high body mass index (BMI) is closely associated with increased breast cancer risk. Despite the established associations of BMI and tumor necrosis factor-α (TNF-α) with breast cancer, few studies have explored their combined effects on breast cancer development. The aim of our study was to evaluate the separate and combined associations of BMI and TNF-α with breast cancer risk.
Material and methods:
A case-control study was conducted involving 794 women diagnosed with breast cancer and 268 age-matched healthy controls from Sun Yat-sen University’s affiliated hospitals between October 2008 and March 2018. Data on demographic characteristics, clinical features, and TNF-α levels were collected. Logistic regression models were used to calculate odds ratios (ORs) and 95% confidence intervals (CIs) for the associations between BMI, TNF-α, and breast cancer risk.
Results:
High levels of TNF-α (≥ 58.45 µg/ml) were significantly associated with an increased risk of breast cancer (OR = 1.500; 95% CI: 1.112–2.022). Elevated TNF-α levels were associated with early clinical stage, positivity for ER, PR, and HER2, high Ki67 expression, and the absence of lymphatic and distant metastases. No significant association was found between BMI and breast cancer risk (OR = 0.947; 95% CI: 0.685–1.310), nor was there a significant interaction effect between BMI and TNF-α.
Conclusions:
TNF-α plays a significant role in breast cancer development, particularly in early clinical stages, and in specific pathological features. BMI alone is not a significant predictor of breast cancer risk. These findings underscore the importance of TNF-α as a potential target for breast cancer prevention and treatment strategies.
A high body mass index (BMI) is closely associated with increased breast cancer risk. Despite the established associations of BMI and tumor necrosis factor-α (TNF-α) with breast cancer, few studies have explored their combined effects on breast cancer development. The aim of our study was to evaluate the separate and combined associations of BMI and TNF-α with breast cancer risk.
Material and methods:
A case-control study was conducted involving 794 women diagnosed with breast cancer and 268 age-matched healthy controls from Sun Yat-sen University’s affiliated hospitals between October 2008 and March 2018. Data on demographic characteristics, clinical features, and TNF-α levels were collected. Logistic regression models were used to calculate odds ratios (ORs) and 95% confidence intervals (CIs) for the associations between BMI, TNF-α, and breast cancer risk.
Results:
High levels of TNF-α (≥ 58.45 µg/ml) were significantly associated with an increased risk of breast cancer (OR = 1.500; 95% CI: 1.112–2.022). Elevated TNF-α levels were associated with early clinical stage, positivity for ER, PR, and HER2, high Ki67 expression, and the absence of lymphatic and distant metastases. No significant association was found between BMI and breast cancer risk (OR = 0.947; 95% CI: 0.685–1.310), nor was there a significant interaction effect between BMI and TNF-α.
Conclusions:
TNF-α plays a significant role in breast cancer development, particularly in early clinical stages, and in specific pathological features. BMI alone is not a significant predictor of breast cancer risk. These findings underscore the importance of TNF-α as a potential target for breast cancer prevention and treatment strategies.
REFERENCES (74)
1.
Raziani Y, Raziani S. Investigating the predictors of overweight and obesity in children. Int J Adv Stud Humanit Soc Sci 2020; 9: 262-80.
2.
Nuttall FQ. Body mass index: obesity, BMI, and health: a critical review. Nutrition Today 2015; 50: 117-28.
3.
Lisevick A, Cartmel B, Harrigan M, et al. Effect of the lifestyle, exercise, and nutrition (Lean) study on long-term weight loss maintenance in women with breast cancer. Nutrients 2021; 13: 3265.
4.
Chandrasekaran P, Weiskirchen R. The signaling pathways in obesity-related complications. J Cell Commun Signal 2024; 18: e12039.
5.
Vitale E, Rizzo A, Santa K, Jirillo E. Associations between “Cancer Risk”,“Inflammation” and “Metabolic Syndrome”: a scoping review. Biology 2024; 13: 352.
6.
Esser N, Legrand-Poels S, Piette J, Scheen AJ, Paquot N. Inflammation as a link between obesity, metabolic syndrome and type 2 diabetes. Diabetes Res Clin Pract 2014; 105: 141-50.
7.
Morrione A, Belfiore A. Obesity, diabetes, and cancer: the role of the insulin/IGF axis; mechanisms and clinical implications. Biomoleculas 2022; 12: 612.
8.
Booth A, Magnuson A, Fouts J, Foster M. Adipose tissue, obesity and adipokines: role in cancer promotion. Hormone Mol Biol Clin Investig 2015; 21: 57-74.
9.
Fan P, Siwak DR, Abderrahman B, Agboke FA, Yerrum S, Jordan VC. Suppression of nuclear factor-B by glucocorticoid receptor blocks estrogen-induced apoptosis in estrogen-deprived breast cancer cells. Mol Cancer Ther 2019; 18: 1684-95.
10.
Dibaba DT, Judd SE, Gilchrist SC, et al. Association between obesity and biomarkers of inflammation and metabolism with cancer mortality in a prospective cohort study. Metabolism 2019; 94: 69-76.
11.
King J, Mir H, Singh S. Association of cytokines and chemokines in pathogenesis of breast cancer. Progress Mol Biol Transl Sci 2017; 151: 113-36.
12.
Mubtasim N, Moustaid-Moussa N, Gollahon L. The complex biology of the obesity-induced, metastasis-promoting tumor microenvironment in breast cancer. Int J Mol Sci 2022; 23: 2480.
13.
Wen Y, Xiong X, Harris J, Zaytseva Y, Gao T. Abstract 4088: Adipocytes-mediated autophagy activation and metabolic reprogramming promotes colon cancer survival. Cancer Res 2016; 76 (14 Suppl): 4088.
14.
Mohammed AK. Comparison of TNF- and IL-19 concentrations at different stages of breast cancer. J Med Life 2022; 15: 845-9.
15.
Mallick R, Basak S, Das RK, et al. Fatty acids and their proteins in adipose tissue inflammation. Cell Biochem Biophys 2024; 82: 35-51.
16.
Valjevac A. The endocrine function of adipose tissue. In: Meta-Inflammation and Obesity. Valjevac A. 2020: 23.
17.
Gilbert CA, Slingerland JM. Cytokines, obesity, and cancer: new insights on mechanisms linking obesity to cancer risk and progression. Annu Rev Med 2013; 64: 45-57.
18.
Bima A, Eldakhakhny B, Alamoudi AA, et al. Molecular study of the protective effect of a low-carbohydrate, high-fat diet against brain insulin resistance in an animal model of metabolic syndrome. Brain Sci 2023; 13: 1383.
19.
Witkowska-Sedek E, Pyrzak B. Chronic inflammation and the growth hormone/insulin-like growth factor-1 axis. Cent Eur J Immunol 2020; 45: 469-75.
20.
Kim HS, Ali O, Shim M, et al. Insulin-like growth factor binding protein-3 induces insulin resistance in adipocytes in vitro and in rats in vivo. Pediatr Res 2007; 61: 159-64.
21.
Boyd NF, Martin LJ, Sun L, et al. Body size, mammographic density, and breast cancer risk. Cancer Epidemiol Biomarkers Prev 2006; 15: 2086-92.
22.
Lukanova A, Bjor O, Kaaks R, et al. Body mass index and cancer: results from the Northern Sweden Health and Disease Cohort. Int J Cancer 2006; 118: 458-66.
23.
Zhao D, Wang X, Beeraka NM, et al. High body mass index was associated with human epidermal growth factor receptor 2-positivity, histological grade and disease progression differently by age. World J Oncol 2023; 14: 75-83.
24.
To SQ, Knower KC, Clyne CD. Origins and actions of tumor necrosis factor alpha in postmenopausal breast cancer. J Interferon Cytokine Res 2013; 33: 335-45.
25.
Lee HM, Lee HJ, Chang JE. Inflammatory cytokine: an attractive target for cancer treatment. Biomedicines 2022; 10: 2116.
26.
Creighton CJ, Casa A, Lazard Z, et al. Insulin-like growth factor-I activates gene transcription programs strongly associated with poor breast cancer prognosis. J Clin Oncol 2008; 26: 4078-85.
27.
Giuliano AE, Connolly JL, Edge SB, et al. Breast cancer – major changes in the American Joint Committee on Cancer eighth edition cancer staging manual. CA Cancer J Clin 2017; 67: 290-303.
29.
Devericks EN, Carson MS, McCullough LE, Coleman MF, Hursting SD. The obesity-breast cancer link: a multidisciplinary perspective. Cancer Metastasis Rev 2022; 41: 607-25.
30.
Kolb R, Zhang W. Obesity and breast cancer: a case of inflamed adipose tissue. Cancers 2020; 12: 1686.
31.
Summer M, Sajjad A, Ali S, Hussain T. Exploring the underlying correlation between microbiota, immune system, hormones, and inflammation with breast cancer and the role of probiotics, prebiotics and postbiotics. Arch Microbiol 2024; 206: 145.
32.
Harrison S, Tilling K, Turner EL, et al. Systematic review and meta-analysis of the associations between body mass index, prostate cancer, advanced prostate cancer, and prostate-specific antigen. Cancer Causes Control 2020; 31: 431-49.
33.
Xu P, Tao Z, Yang H, Zhang C. Obesity and early-onset colorectal cancer risk: emerging clinical evidence and biological mechanisms. Front Oncol 2024; 14: 1366544.
34.
Ellis PE, Barron GA, Bermano G. Adipocytokines and their relationship to endometrial cancer risk: a systematic review and meta-analysis. Gynecol Oncol 2020; 158: 507-16.
35.
Baczewska M, Bojczuk K, Kołakowski A, Dobroch J, Guzik P, Knapp P. Obesity and energy substrate transporters in ovarian cancer. Molecules 2021; 26: 1659.
36.
Yoon YS, Kwon AR, Lee YK, Oh SW. Circulating adipokines and risk of obesity related cancers: a systematic review and meta-analysis. Obesity Res Clin Pract 2019; 13: 329-39.
37.
Li J, Tang Y, Lin TC, Zeng H, Mason JB, Liu Z. Tumor necrosis factor- knockout mitigates intestinal inflammation and tumorigenesis in obese Apc1638N mice. J Nutr Biochem 2023; 117: 109355.
38.
Agnoli C, Grioni S, Pala V, et al. Biomarkers of inflammation and breast cancer risk: a case-control study nested in the EPIC-Varese cohort. Sci Rep 2017; 7: 12708.
39.
Dias JA, Fredrikson GN, Ericson U, et al. Low-grade inflammation, oxidative stress and risk of invasive postmenopausal breast cancer-a nested case‒control study from the malmö diet and cancer cohort. PLoS One 2016; 11: e0158959.
40.
Dewald JH, Cavdarli S, Steenackers A, et al. TNF differentially regulates ganglioside biosynthesis and expression in breast cancer cell lines. PLoS One 2018; 13: e0196369.
41.
Schairer C, Li Y, Frawley P, et al. Risk factors for inflammatory breast cancer and other invasive breast cancers. J Natl Cancer Inst 2013; 105: 1373-84.
42.
Li H, Sun X, Miller E, et al. BMI, reproductive factors, and breast cancer molecular subtypes: a case-control study and meta-analysis. J Epidemiol 2017; 27: 143-51.
43.
Chen H, Qian X, Tao Y, et al. Impact of body mass index and its change on survival outcomes in patients with early breast cancer: a pooled analysis of individual-level data from BCIRG-001 and BCIRG-005 trials. Breast 2023; 71: 1-12.
44.
Daraz FG, Windarti I, Ayu Sangging PR. The role of obesity in breast cancer metastasis. Med Profession J Lampung 2023; 13: 172-8.
45.
Bhardwaj P, Iyengar NM, Zahid H, et al. Obesity promotes breast epithelium DNA damage in women carrying a germline mutation in BRCA1 or BRCA2. Sci Transl Med 2023; 15: eade1857.
46.
Chen Y, Liu L, Zhou Q, et al. Body mass index had different effects on premenopausal and postmenopausal breast cancer risks: a dose-response meta-analysis with 3,318,796 subjects from 31 cohort studies. BMC Public Health 2017; 17: 936.
47.
Fontvieille E, Viallon V, Recalde M, et al. Body mass index and cancer risk among adults with and without cardiometabolic diseases: evidence from the EPIC and UK Biobank prospective cohort studies. BMC Med 2023; 21: 418.
48.
Simone V, D’avenia M, Argentiero A, et al. Obesity and breast cancer: molecular interconnections and potential clinical applications. Oncologist 2016; 21: 404-17.
49.
Quiroga-Morales LA, Sat-Muñoz D, Martínez-Herrera BE, et al. Obesity and adipocytokines in breast cancer and benign breast disease. Rev Méd Inst Mex Seguro Soc 2018; 56: 246-54.
50.
Purohit A, Newman SP, Reed MJ. The role of cytokines in regulating estrogen synthesis: implications for the etiology of breast cancer. Breast Cancer Res 2002; 4: 65-9.
51.
Subbaramaiah K, Howe LR, Bhardwaj P, et al. Obesity is associated with inflammation and elevated aromatase expression in the mouse mammary gland. Cancer Prev Res 2011; 4: 329-46.
52.
Gunter MJ, Wang T, Cushman M, et al. Circulating adipokines and inflammatory markers and postmenopausal breast cancer risk. J Natl Cancer Inst 2015; 107: djv169.
53.
To SQ, Knower KC, Clyne CD. Origins and actions of tumor necrosis factor in postmenopausal breast cancer. J Interferon Cytokine Res 2013; 33: 335-45.
54.
Ajabnoor GM. The molecular and genetic interactions between obesity and breast cancer risk. Medicina 2023; 59: 1338.
55.
Chang SL, Tchernof A, Durocher F, Diorio C. Associations of biomarkers of inflammation and breast cancer in the breast adipose tissue of women with combined measures of adiposity. J Obes 2021; 2021: 3620147.
56.
Schindler EA, Takita C, Collado-Mesa F, et al. The interrelationship between obesity and race in breast cancer prognosis: a prospective cohort study. BMC Women’s Health 2024; 24: 312.
57.
Il’yasova D, Colbert LH, Harris TB, et al. Circulating levels of inflammatory markers and cancer risk in the health aging and body composition cohort. Cancer Epidemiol Biomarkers Prev 2005; 14: 2413-8.
58.
Manta L, Suciu N, Toader O, Purcărea R, Constantin A, Popa F. The etiopathogenesis of uterine fibromatosis. J Med Life 2016; 9: 39.
59.
Zhou XL, Fan W, Yang G, Yu MX. The clinical significance of PR, ER, NF-B, and TNF- in breast cancer. Dis Markers 2014; 2014: 494581.
60.
Howlader N, Altekruse SF, Li CI, et al. US incidence of breast cancer subtypes defined by joint hormone receptor and HER2 status. J Natl Cancer Inst 2014; 106: dju055.
61.
Weng Y, Liang W, Ji Y, et al. Key genes and prognostic analysis in HER2+ breast cancer. Technol Cancer Res Treat 2021; 20: 1533033820983298.
62.
Iwase T, Harano K, Masuda H, et al. Quantitative hormone receptor (HR) expression and gene expression analysis in HR+ inflammatory breast cancer (IBC) vs non-IBC. BMC Cancer 2020; 20: 430.
63.
Diaz-Santana MV, O’Brien KM, D’Aloisio AA, Regalado G, Sandler DP, Weinberg CR. Perinatal and postnatal exposures and risk of young-onset breast cancer. Breast Cancer Res 2020; 22: 88.
64.
Lin D, Liu Y, Tobias DK, Sturgeon K. Physical activity from menarche-to-first pregnancy and risk of breast cancer: the California teachers study. Cancer Causes Control 2022; 33: 1343-53.
65.
Khalis M, Charbotel B, Chajès V, et al. Menstrual and reproductive factors and risk of breast cancer: a case‒control study in the Fez region, Morocco. PLoS One 2018; 13: e0191333.
66.
Chakor G, Deshpande R, Morane D. Overview of menarche, menstruation and menstrual hygiene. Innov J Nurs Healthc 2022; 8: 18-21.
67.
Collaborative Group on Hormonal Factors in Breast Cancer. Menarche, menopause, and breast cancer risk: individual participant meta-analysis, including 118 964 women with breast cancer from 117 epidemiological studies. Lancet Oncol 2012; 13: 1141-51.
68.
Mustafa M, Sarfraz S, Saleem G, et al. Beyond milk and nurture: breastfeeding’s powerful impact on breast cancer. Geburtshilfe Frauenheilkd 2024; 84: 541-54.
69.
Islami F, Liu Y, Jemal A, et al. Breastfeeding and breast cancer risk by receptor status – a systematic review and meta-analysis. Ann Oncol 2015; 26: 2398-407.
70.
Ahmadinejad N, Movahedinia S, Movahedinia S, Naieni KH, Nedjat S. Distribution of breast density in Iranian women and its association with breast cancer risk factors. Iranian Red Crescent Med J 2013; 15: e16615.
71.
Bothou A, Zervoudis S, Iliadou M, et al. Breastfeeding and breast cancer risk: our experience and mini-review of the literature. Materia Sociomed 2022; 34: 28.
72.
Xu Z, Yan S, Wu H, et al. The influence of TNF- and Ang II on the proliferation, migration and invasion of HepG2 cells by regulating the expression of GRK2. Cancer Chemother Pharmacol 2017; 79: 747-58.
73.
Wolczyk D, Zaremba-Czogalla M, Hryniewicz-Jankowska A, et al. TNF- promotes breast cancer cell migration and enhances the concentration of membrane-associated proteases in lipid rafts. Cell Oncol 2016; 39: 353-63.
74.
Gravena AAF, Lopes TCR, de Oliveira Demitto M, et al. The obesity and the risk of breast cancer among pre and postmenopausal women. Asian Pac J Cancer Prev 2018; 19: 2429-36.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.