Introduction
Vertebral fractures are the most common fracture associated with low bone mass and skeletal fragility [1, 2]. Variance in clinical presentations of vertebral fractures may contribute partly to the wide variations of their prevalence and incidence in previous studies [3, 4], with the highest rates in North America and Asia [5]. They commonly occur in the elderly [6], and can cause substantial pain, disability, adverse health outcomes, and even mortality [7]. The impacts of sex and gender on orthopedic health, such as the higher rates of bone deformities in females and osteoporosis in postmenopausal women, are also important issues deserving further investigations [8]. Since populations are rapidly aging worldwide [9], vertebral fractures have given rise to a heavy healthcare burden and constitute a serious public health issue [1].
For patients suffering from a vertebral fracture, percutaneous vertebroplasty has been developed to relieve pain and improve their physical function and quality of life [10]. Although vertebroplasty has become a common surgical procedure, its effects on symptoms relief, quality of life, and long-term patient outcomes remain unclear [11–13]. Several patient-reported outcome measures are recommended for assessment of general health quality and function in patients who undergo spine surgery [14]. Among these, the Oswestry Disability Index (ODI) [15] and EuroQol-5D (EQ-5D) [16] have been widely used in clinical studies of patients with vertebral fractures [17–21]. However, whether patient-reported outcome measures were associated with long-term mortality in patients who received vertebroplasty is not yet clear.
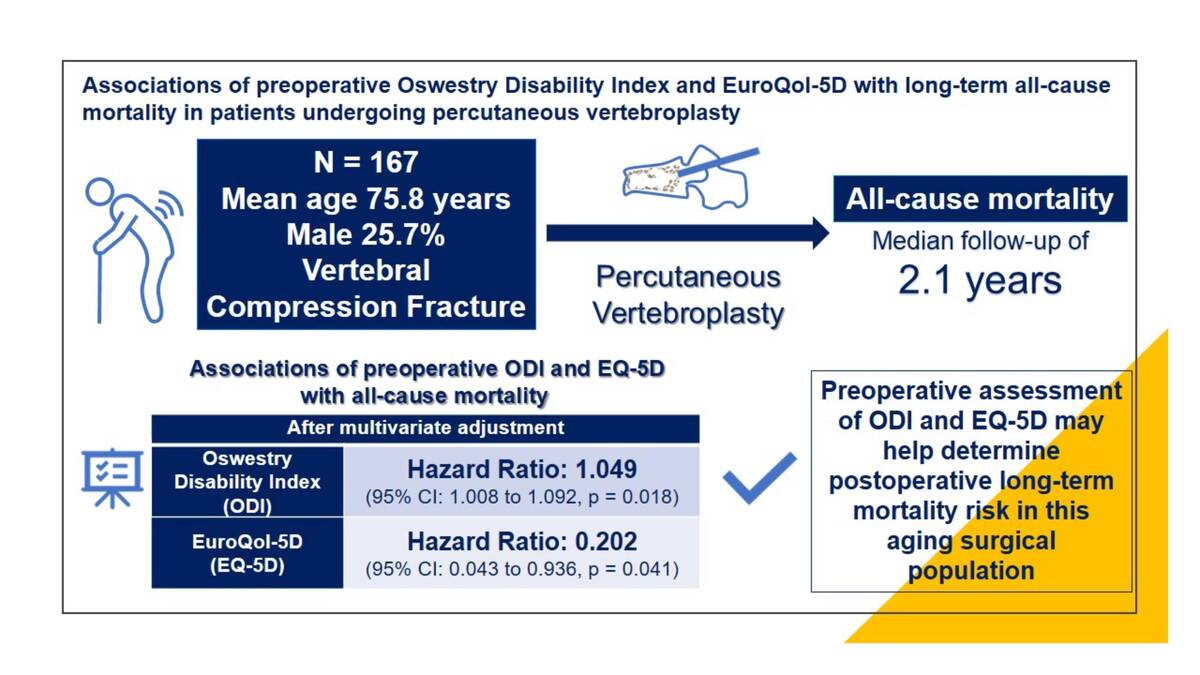
In this study, we aimed to investigate the associations of preoperative ODI and EQ-5D with long-term mortality in patients with vertebral compression fractures who had undergone percutaneous vertebroplasty.
Material and methods
This retrospective study was conducted in a tertiary medical center. The study protocol was approved by the Institutional Review Board of Taichung Veterans General Hospital, Taichung, Taiwan (approval number CE22167A). Patient informed consent was waived due to the retrospective study design. We identified adult patients who had a single-level vertebral compression fracture and received percutaneous vertebroplasty between 2013 and 2020. In previous studies [22, 23] that examined quality of life for osteoporosis-related conditions (including hip fracture, vertebral fracture, and distal forearm fracture), the follow-up duration was generally 18 months or less. In another study [24] that reported postoperative outcomes including all-cause mortality in patients undergoing thoracolumbar fusion for spinal deformity, 71% of patients were followed up for at least 10 months. Compared with these studies, our study period is sufficient to observe the effects of percutaneous vertebroplasty on patients’ outcomes.
In our patients, surgical intervention was conducted after preoperative assessment including ODI [15] and EQ-5D [16]. Patients with traumatic fractures, burst fractures, and pathologic fractures according to discharge diagnosis, as well as those who had missing information on preoperative assessment of ODI and EQ-5D, were excluded. Pathologic fracture was defined as fractures that occur without an adequate traumatic event due to focal benign or malignant skeletal lesions [25]. For optimal preoperative care in an orthopedic department, nursing leadership and team work are important during the COVID-19 pandemic and post-COVID-19 era [26]. Assessment of ODI [15] and EQ-5D [16] was conducted by a trained nurse with more than 8 years of experience as part of the preoperative evaluation [14] in our hospital. The assessment of ODI [15] contains ten questions (pain intensity, personal care, lifting, walking, sitting, standing, sleeping, sex life if applicable, social life, and traveling) on limitations of activities of daily living. Each item is rated on a 0–5-point scale, and a higher ODI score indicates greater severity of disability. The EQ-5D [16] consists of an assessment of five dimensions (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression), and a higher value indicates a better quality of life. The reliability of ODI and EQ-5D in patients undergoing spinal surgery has been assessed in previous studies [27, 28]. The validity of ODI and EQ-5D to assess the effectiveness of lumbar fusion for degenerative lumbar spondylolisthesis was evaluated in a prospective cohort study [29]. The area under the ROC curve against patient-reported outcomes was 0.94 for ODI and 0.97 for EQ-5D. The specificity and sensitivity for ODI were ~85% and ~95%, respectively. The respective values for EQ-5D were ~100% and ~90% [29]. Baseline demographics, including age (range: 48 to 94 years), sex, and body mass index, and medical history, were collected from electronic medical records. Survival status of the study patients at the end of March 2021 was obtained from the Ministry of Health and Welfare, R.O.C. De-identified data were then used for analyses.
Statistical analysis
A statistician (CH Lin) conducted all statistical analyses independently using de-identified data. Categorical and continuous variables are presented as number (percentage) and mean ± SD, respectively. The outcome of interest was all-cause mortality. The independent variables examined were preoperative ODI and EQ-5D. The associations of preoperative ODI and EQ-5D with all-cause mortality were examined using the Cox proportional hazards model, which is a frequently used approach to investigate relationships between the time to event outcome and a set of explanatory variables. We considered the following variables as potential confounders: age, sex, body mass index, smoking, diabetes, hypertension, chronic kidney disease, osteoporosis, and medical treatment for osteoporosis. These variables were adjusted in the Cox proportional hazards models to examine the independent associations of ODI and EQ-5D with all-cause mortality. A Cox proportional hazards model with restricted cubic splines [30] was used to display the relation between independent variables (preoperative ODI and EQ-5D) and all-cause mortality. All of the statistical analyses were performed using IBM SPSS Statistics version 22.0 (IBM Corp., Armonk, NY, USA). A two-sided p-value of less than 0.05 was considered statistically significant.
Results
We identified 209 adult patients who had a single-level vertebral compression fracture and received percutaneous vertebroplasty. After excluding 18 patients with traumatic fractures (n = 10), burst fractures (n = 2), or pathologic fractures (n = 6), and 24 patients who had missing information on preoperative ODI or EQ-5D, a total of 167 patients were analyzed (Table I). The mean age of the study sample was 75.8 ±9.3 years (range from 48 to 94 years), and 25.7% of them were male. The prevalence rates of diabetes, hypertension, and chronic kidney disease were 19.8%, 53.3%, and 34.1%, respectively. Most of the patients had osteoporosis (74.3%) and received medical treatment (63.5%). Vertebroplasty was performed at the thoracic (T) (42.5%) or lumbar (L) spine (57.5%) level. The distribution of operation level of T spine vertebroplasty was T6 (n = 2), T7 (n = 3), T8 (n = 3), T9 (n = 3), T10 (n = 6), T11 (n = 15), and T12 (n = 39). For the L spine, the distribution was L1 (n = 41), L2 (n = 29), L3 (n = 13), L4 (n = 9), and L5 (n = 4). The mean pre-operative ODI and EQ-5D were 71.3 ±12.4 and 0.25 ±0.22 respectively. There were 28 patients who died during a median follow-up duration of 2.1 years (63.6 per 1000 patient-years). Among the 28 patients who died during the follow-up period, 12 (42.9%) had T spine fracture. None of the 28 patients died during the index hospitalization, while four of them died within 150 days after the surgery (range: 75–119 days). Hence, we inferred that the cause of death was not likely related to vertebroplasty. There was no significant difference regarding the distribution of the levels of spine fracture compared to those who were alive (T spine facture 42.4% [59/139], p = 0.968) by the end of the study period.
Table I
Baseline characteristics of study population
The associations of preoperative ODI and EQ-5D with all-cause mortality were examined using Cox proportional hazard models with multivariate adjustment (age, sex, body mass index, smoking, and concomitant chronic diseases). As shown in Table II, preoperative ODI was significantly associated with all-cause mortality after vertebroplasty (HR = 1.060, 95% CI: 1.023 to 1.098, p = 0.001). The association remained significant (HR = 1.049, 95% CI: 1.008 to 1.092, p = 0.018) after multivariate adjustment. Most previous studies examined epidemiology of vertebral fractures in aged people (for example, ≥ 65 years) [1]. We examined findings of the multivariate adjusted models in our patients aged ≥ 65 years (n = 146), and similar findings were noted (HR = 1.054, 95% CI: 1.010 to 1.101, p = 0.016). In contrast, preoperative EQ-5D was associated with a lower risk of all-cause mortality after the surgery (HR = 0.102, 95% CI: 0.025 to 0.420, p = 0.002). The association was independent of age, sex, body mass index, and other comorbidities (HR = 0.202, 95% CI: 0.043 to 0.936, p = 0.041). The findings were consistent in patients aged ≥ 65 years (HR = 0.168, 95% CI: 0.035 to 0.808, p = 0.026).
Table II
Associations of preoperative ODI and EQ-5D with all-cause mortality
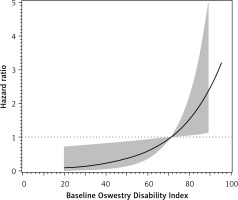
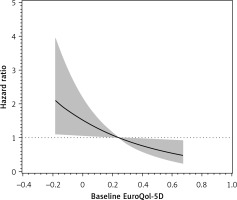
Cubic spline of preoperative ODI and EQ-5D versus risk of all-cause mortality by a Cox proportional hazards model was conducted [30]. Scaled Schoenfeld residuals were used to test the assumption of the Cox proportional hazards model, and no violation of the assumption was detected. Figure 1 shows the cubic spline of preoperative ODI versus risk of all-cause mortality in the study sample. An increase in all-cause mortality risk was observed in patients who had a preoperative ODI higher than 70. Figure 2 shows the cubic spline of preoperative EQ-5D versus risk of all-cause mortality. We observed an increase in all-cause mortality risk in those who had a preoperative EQ-5D lower than 0.2.
Discussion
In this study, we found that preoperative patient-reported outcome measures (ODI and EQ-5D) were associated with long-term all-cause mortality in patients who underwent vertebroplasty for a single-level vertebral compression fracture. Although patient-reported outcome measures have been proposed for assessment of general health quality and function in those who received spine surgery [14], their associations with long-term outcomes are not yet clear. To the best of our knowledge, our study is the first to investigate the associations between preoperative patient-reported outcome measures (ODI and EQ-5D) and long-term mortality in patients who have undergone vertebroplasty for a single-level vertebral compression fracture.
Patients suffering from a vertebral compression fracture are typically aged ≥ 65 years [11–13], and age is a predictor of vertebral fractures [1]. Moreover, vertebral fractures have been associated with progression of kyphosis, which in turn is associated with reduced pulmonary function [31] and physical function [32], and possibly falls [33]. All of these effects may lead to impairment of quality of life and a higher risk of mortality [1, 34, 35]. Vertebroplasty may relieve symptoms and improve functional outcomes in these patients [13]; nevertheless, its effect on long-term mortality is not yet clear [11, 12, 36]. Percutaneous vertebroplasty relieved pain and improved quality of life in patients (mean age: 73.3 ±7.9 years) with osteoporotic compression fractures in a prospective study [10]. These findings were similar to the results of an open-label prospective randomized trial [13], although there have been inconsistent studies [11, 12]. These studies varied in selected populations, assessment of outcomes, and duration of follow-up. In the two randomized trials [11, 12] which reported no beneficial effect of vertebroplasty compared with the control group, the authors included patients with a duration of pain of up to 12 months, and assessed their primary outcome (pain scores) at 1 and 3 months, respectively. In the other randomized study [13], the authors included patients with uncontrolled pain for less than 6 weeks, and the primary outcome (pain score) was assessed at 1 month and 1 year. Some other issues that may contribute to the variability in findings across different studies have been discussed [37].
Patients with compression fractures are at a higher risk of mortality. In a cohort study [38] of patients older than 60 years, the risk of long-term mortality doubled in those who had osteoporotic vertebral fractures. The increase in mortality risk after vertebral fractures might be partly attributed to functional disability, physical inactivity, and impairment of quality of life [31–33], all of which have been associated with mortality risk in elderly populations [39–43]. Nevertheless, the effects of surgical intervention on these measures and mortality outcome in patients with vertebral fractures are not yet clear. Findings from previous reports [36, 44, 45] on the risk of mortality after surgical interventions for vertebral fractures are inconsistent. In a large retrospective cohort study of more than 850,000 patients with vertebral compression fractures and up to 4 years of follow-up [44], the surgically treated cohort (kyphoplasty or vertebroplasty) had a significantly lower risk of mortality (adjusted relative risk 0.63, 95% CI: 0.62 to 0.64, p < 0.001) compared with the cohort not surgically treated. In contrast, surgical treatment (kyphoplasty or vertebroplasty) for osteoporotic vertebral fractures had no significant difference in 1-year mortality risk (hazard ratio = 0.92, 95% CI: 0.81 to 1.04, p = 0.18) compared with the propensity score matched control group [36]. In another retrospective cohort study [45], vertebroplasty for vertebral compression fractures had a non-significantly higher risk of mortality after multivariate adjustment (adjusted hazard ratio = 1.17, 95% CI: 0.96 to 1.42), compared with the control group after a mean follow-up period of nearly 4 years. All these reports are retrospective cohort studies, and there may be confounding factors that cannot be addressed due to the retrospective study design. Moreover, patient-reported outcome measures (such as ODI and EQ-5D) were not included in these analyses. In our study, we investigated the association between preoperative assessment of ODI and EQ-5D with postoperative long-term mortality in patients undergoing vertebroplasty. Preoperative assessment of patient-reported outcome measures [14] may represent the baseline condition of disability and quality of life and help predict long-term outcomes in this aging population. Based on our findings, a higher preoperative ODI and a lower preoperative EQ-5D were independently associated with a higher risk of mortality in patients undergoing vertebroplasty for a single-level vertebral compression fracture during a median follow-up period of 2.1 years. Our results are in line with a recent retrospective study [46] which revealed that preoperative EQ-5D was negatively associated with postoperative mortality during a mean follow-up period of 7.5 years in patients undergoing total hip arthroplasty and knee arthroplasty. Taken together, we suggest that preoperative assessment of ODI and EQ-5D, both of which are recommended patient-reported outcome measures in spine surgery [14], may help determine postoperative long-term mortality risk in patients undergoing vertebroplasty for vertebral compression fractures.
The strength of this study is that the ODI and EQ-5D were assessed by a trained nurse at baseline. The reliability and validity of ODI and EQ-5D in patients undergoing spinal surgery have been reported [27–29]. Moreover, the survival status was examined after a median follow-up duration of more than 2 years. In contrast, the follow-up period of most previous studies was usually less than 18 months [22–24]. However, there were several limitations of this study. First, the retrospective study design might have led to patient selection bias. Moreover, the size of the study sample was relatively small. Second, although we had adjusted for some concomitant chronic diseases (such as diabetes and hypertension) in the analyses to determine the associations of baseline ODI and EQ-5D with all-cause mortality, we did not assess disease control status (such as blood glucose and blood pressure levels), which might have confounded our results. Third, the use of complex and lengthy questionnaires (ODI and EQ-5D) may have posed challenges in terms of patient comprehension and completion, possibly leading to incomplete or inaccurate data collection. Despite these limitations, we report for the first time that preoperative assessment of ODI and EQ-5D was associated with long-term all-cause mortality in patients undergoing percutaneous vertebroplasty. Our findings need to be confirmed in future studies with a larger sample size.
In conclusion, a higher preoperative ODI and a lower preoperative EQ-5D were independently associated with a higher risk of long-term all-cause mortality in patients undergoing vertebroplasty for a single-level vertebral compression fracture. Preoperative assessment of ODI and EQ-5D may help determine postoperative long-term mortality risk in this aging population. We suggest that careful consideration is required before performing vertebroplasty in elderly patients with a high ODI or a low EQ-5D.