Introduction
Due to the anatomy and physiology of the posterior maxilla, sinus enlargement, and postextraction bone resorption, there is limited residual alveolar bone height. Antral floor bone becomes thin under these circumstances, making it unsuitable for implant placement. This problem has been overcome through various bone augmentation techniques to enhance bone formation in the maxillary sinus. A bony window is created in the lateral wall of the sinus, the sinus membrane is lifted, and a bone grafting material is placed in the window to enhance bone growth. There are two ways to perform this procedure. When residual bone is highly minimal, implants may not be stable; these cases require two stages [1–4]. Medicine and dentistry use bone graft materials extensively. Most manufacturers claim physical, chemical, and biological properties. The goal of regenerative and reconstructive surgery has always been to find high-quality biomaterials. Autogenous bone is often considered a gold standard in bone replacement therapy due to its optimal biological properties [5–12]. Sinus bone augmentation has been performed with autografts, allografts, xenografts, and alloplasts. An autograft can be a superior bone graft material due to its osteoconductive, osteoinductive, and osteogenic properties. Still, the donor site morbidity and low availability of autografts make it an undesirable option. There is also a risk of transmission of disease with allografts and xenografts. To overcome these drawbacks, researchers have searched for alternative biomaterials [1, 13–15]. In a study using organic molecules and polysaccharides from humans, animals, and plants, complementary lectins to cell-surface carbohydrates bind polysaccharides and mediate the cell response. Due to their effect on bone cells and ability to control their structure, plant-derived nanocoatings are potential candidates for medical devices. Indirect and direct adhesion explains the effect on bone cells [16]. There is considerable evidence that osteoporosis abnormally affects implant osseointegration and fixation in animals, according to animal studies. Studies found that implants could osseointegrate into osteoporotic bones, but a longer time is required [6–8]. On joint arthroplasty, osteoporosis has different effects on long and jaw bones than on dental implants. Osteoclasts’ bone resorption and formation are imbalanced by bone, which contributes to osteoporosis [17]. Bone cells adhere directly to the surface due to the direct mechanism. In an indirect mechanism, proteins bind to invading cells’ surfaces and selectively to distinct receptors. In response to binding to the receptors, the cells will produce an extracellular matrix (ECM), increase adhesion, and proliferate. Developing, maturing, and repairing bone requires osteoblast differentiation. Cell growth and differentiation are closely regulated in terms of initiation and progression. As osteoblasts develop, cell growth genes are sequentially regulated. Proliferation, ECM synthesis, development and maturity, and mineralization occur [16]. Topical herbal formulations particularly benefit joint injuries, inflammation, and fractured bones. Chinese herbal medicinal approaches have been shown to boost osteogenesis and minimize extremely unbalanced bone turnover, resulting in increased bone mineral density and minimal microstructural degradation. They also have anabolic and anticatabolic effects [18]. This review discusses herbal materials’ role in bone regeneration following dental implants.
Herbal material in accelerating bone regeneration
Flavonoids are bioactive polyphenolic compounds that can improve bone health and are found in fruits and vegetables. Several studies over the past few decades have shown that flavonoids from plant-based foods benefit bone mineral density (BMD). The results of a large group study examining bone health and energy-adjusted total flavonoid intake in perimenopausal Scottish women showed that flavonoid intake is associated with improved bone health. Women with osteoporosis, characterized by low BMD and increased fracture risk due to low BMD, may benefit from olive polyphenol intake in an 8-month prospective human intervention study [19]. Bone regeneration is effectively treated with herbal medicines. Drynaria fortunei (Gusuibu; GSB) and Carthami flos (Gusuibu) are herbal medicines that affect bone healing. The mechanism of action of GSB is unclear, but it is a popular traditional Chinese medicine (TCM). It has been demonstrated that herbs can stimulate the proliferation of human fibroblasts and periosteal osteoprogenitor cells, as well as fetal rat calvaria osteoblasts, in a regenerative medicine study, as herbs play an essential role in cell differentiation (including epigenetic pathways). Naringin is a compound found in Rhizoma drynariae that inhibits retinoic acid-induced osteoporosis in rats, stimulates bone formation, and increases BMP-2 [20–25]. Radiographic bone density and the area around titanium implants were evaluated after homeopathic treatment with comfrey (6CH) by Sakakura et al. 24 rats were divided into two groups: a control (C) and a test (SO). The tibias of each animal received titanium micro-implants. Drinking water was mixed with 10 drops of comfrey 6CH to prepare the animals for sacrifice. Seven days, fourteen days, and twenty-eight days after surgery, animals were sacrificed. Standard digital radiographs were used to obtain baseline and final images. Sakakura et al. evaluated changes in bone density and the implant area using digital subtractions. At 14 days after surgery, group SO showed a significant difference in the mean gray shade compared to group C. Group SO showed a statistically significant difference in bone gain pixels, however. A small study suggests that comfrey administration increases titanium implant radiographic bone density [26]. Cyclosporin A (CsA) is used to assess osseointegration in ozonated plant extracts (herein called ozonated oil). A and B were injected with dental implants into rabbit tibiae. One injection of CsA suppressed the immune system in groups A and B. During 8 weeks, group A received 0.55 ml of ozonated oil applied around dental implants, while group B received none. On the day of sacrifice and during surgery implants were radiographed. The two groups had different bone quality. Scanning electron and light microscopies were used to assess osseointegration radiographically. A light microscopic examination of ozonated group A specimens demonstrated that the maturity of the bone was better organized than in group B. The results suggest that topical ozonated oil and short-term administration of CsA may affect dental implant osseointegration and bone density. Hence, ozonated oil may improve osseointegration surrounding dental implants by topically applying it [27]. Mecsina (herbal extract) was studied by Aydin et al. in combination with xenogeneic graft material (bovine bone graft). As an effective bone formation agent, Mecsina Hemostopper increased cell proliferation. Mecsina was found to be an effective option in the augmentation of critical-size defects in rats when combined with xenogeneic bone grafts. Clinical research needs to be conducted on Mecsina Hemostopper to obtain more qualified bone formation [28]. In 2022, Wang et al. examined effects of aucubin (AU) on osteoblastogenesis, antioxidative stress injury, and bone-fracture regeneration in a rat tibial fracture model live, and AU effects on osteoblastogenesis. AU promotes bone-fracture healing partly via the canonical BMP2/Smads signaling pathway and suppresses oxidative stress indirectly through the Nrf2/HO1 signaling pathway [29].
Icariin
Herba Epimedii is used to treat fractures, joint diseases, and gonadal dysfunction. The naturally isolated form of icariin is increasingly used in osteoporosis treatment. In most research studies, high-performance liquid chromatography is used to extract icariin. A growing body of evidence indicates that icariin simultaneously stimulates bone formation and inhibits bone resorption, making it an ideal osteoinductive candidate for bone tissue engineering. Also, icariin can be released steadily and locally using biomaterials. Evidence indicates that icariin increases angiogenesis by stimulating endothelial cell migration, proliferation, and tubule genesis in vivo. In addition to its estrogen mimetic effect, icariin and its derivatives can encourage osteogenic progenitor cell proliferation, maturation, and matrix mineralization for bone remodeling. Bone marrow-derived mesenchymal stem cells (BMSCs) produce osteoblasts. Osteoblast marker genes are expressed in vitro following icariin treatment of MC3T3-E1 cells. Epigenetic regulation of icariin appears to promote human BMSC differentiation. BMSC differentiation is controlled by ROS (reactive oxygen species), and excessive ROS causes corticosteroid-induced osteonecrosis and promotes adipogenic differentiation. As well as maturing primary osteoblasts, icariin can enhance bone remodeling activity. As a result of the icariin treatment, osteoblasts express collagen type I and alkaline phosphatase and mineralize [30].
Semelil (ANGIPARS)
Melilotus officinalis (sweet yellow clover) is an herb that belongs to the Fabaceae legume family, which is the source of Semelil (ANGIPARS). ANGIPARS is an effective medicine to treat diabetic foot ulcers that has been introduced recently. It reduces recurrence rates, facilitates wound healing, and improves healing tissue quality. Microvascularization of tissues is improved by this product, and wound size decreases. The extract has potent antioxidant and neuroprotective properties due to flavonoids, urea, sodium phosphoglycerol, fructose, and selenium. Bone formation relies on angiogenesis, and ANGIPARS increases oxygenation and blood flow in tissues through angiogenesis [5]. Through BMP-2 signaling pathways, ANGIPARS induces osteogenesis, improving bone remodeling and maturation of defects filled with it. Bio-Oss’ surface porosity facilitates the formation of osteogenic cells [5]. Gao et al. noted that 7-methoxy-8-isopentyl coumarin induces differentiation of mesenchymal stem cells and increases cell proliferation in periodontal ligaments [31]. Flavonoids stimulate preosteoblast proliferation and differentiation, as Xiao et al. demonstrated. Cell proliferation, ALP activation, and osteoprotegerin-mRNA expression (OPG/RANKL) were significantly enhanced by flavonoids [32].
Rasouli-Ghahroudi et al. studied the effects of the herbal selenium medicine Semelil. 16 New Zealand male rabbits with identical bony defects (8 mm) were treated with xenogenic bone substitute (Bio-Oss) and the herbal drug semelil (ANGIPARS). There were four groups including A: ANGIPARS, B: Bio-Oss, AB: ANGIPARS/Bio-Oss, and C: untreated control. Four- and 8-week trials were conducted in two groups of rabbits (n = 8). In terms of bone formation, there were significant differences between groups. The most prominent effects were shown by A, B, and C. The mean percentage of new bone formation varied significantly between 4 and 8 weeks. Bone formation was affected by A and B interactions at 4 and 8 weeks. It promotes new bone formation when used with ANGIPARS and Bio-Oss. None of the groups showed foreign body reaction (FBR). Combining ANGIPARS with Bio-Oss increased bone formation and maturation, proving that it works synergistically. Providing osteogenic properties to osteoconductive and space-maintaining materials like Bio-Oss may be possible. ANGIPARS’ clinical efficacy must be assessed in future clinical trials alone or in conjunction with traditional bone graft substitutes such as Bio-Oss [5]. According to Chen et al., flavonoids enhance bone cell proliferation, bone cell differentiation, and bone strength [33]. Using BMP-2, mesenchymal stem cell proliferation and differentiation, as well as bone regeneration, were observed by Lin et al. [34].
Aloe vera
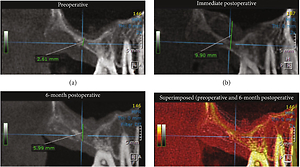
Aloe vera heals wounds. The aloe vera polysaccharide acemannan has been used in bone regeneration biomaterials. The osteoinductive properties of acemannan increase the density of tooth extraction sockets. The radiographic and histological effects of acemannan have not been assessed. An analysis of fresh Aloe vera pulp gel was performed using 13C- and 1H-nuclear magnetic resonance spectroscopy. 150 mg of acemannan was dissolved in sterile distilled water, frozen overnight at –80°C, then lyophilized [1]. Trinh et al. investigated acemannan’s effect on bone formation after sinus lift surgery. An acemannan sponge was used to lift the left posterior maxilla of a 57-year-old patient with an atrophic left posterior maxilla. An acemannan sponge inserted the elevated sinus membrane through the bony window. Postoperative and six-month CBCTs were performed to evaluate the results. On CBCT, the left maxillary sinus was pneumatized and 2.61 mm thick in the edentulous region underneath the edentulous sinus (Figure 1) [1].
Figure 1
A CBCT image of the patient’s left posterior edentulous maxillary region is shown in the sagittal view (A), immediately postoperatively (B), 6 months after augmentation (C), and superimposed between preoperation and 6 months after augmentation (D) [1]
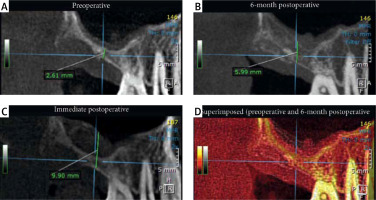
Two stages of lateral sinus lift were planned according to these findings. A clot retraction time assay and bleeding time assay were performed. The implant placement also involved the analysis of a bone core specimen. In CBCT images, after 6 months, new bone was detected, and alveolar bone height was increased. No inflammation was observed in the sections. New bone formed. Newly formed bone had active osteoblasts around it. Several osteocytes in lacunae showed the specimen’s vitality (Figures 2 A, B). The mineralization process was confirmed by calcification. The trabeculae shown in Figure 2 C were thick. Induction of bone formation in sinus lift surgery could be achieved with an acemannan sponge [1].
Figure 2
A – Image of the six-month postoperative bone core specimen stained with H & E at low magnification. B – In lacunae, osteoblasts and osteoclasts (Ob/Ocy) are visible at high magnification. C – Trabeculae (Tb), bone lacunae, and the calcification zone (Calc) are shown in high magnification [1]
Buguzhi (Psoralea corylifolia fruit)
Traditional Chinese medicine uses buguzhi to strengthen bones. This dried fruit is Psoralea corylifolia L, antibacterial, antitumor, and estrogen-like. Also, osteoclasts’ reabsorption of bone in vitro was inhibited. Increasing inorganic phosphorus levels and bone calcification were promoted by crude acetone extracts of Psoralea corylifolia seeds in rats [35]. Wong et al. compared the manufacture of bone in vitro and in vivo using buguzhi (Psoralea corylifolia fruit) extracts in a collagen matrix. The defects measured 5 mm by 10 mm in 9 New Zealand white rabbits. Six defects were grafted with Buguzhi extract. Negative controls left six empty defects and positive controls grafted collagen matrix alone. Histological assessments and dissections were performed after 14 days. Bone cell and new bone formation were quantified in 100 sections (50 per group). More new bone was grafted to implants infused with Buguzhi extract compared to implants in the collagen matrix. Bones did not form in a negative control group. A significant increase in bone cells was observed in the buguzhi group. By injecting buguzhi extract into the collagen matrix, new bone was formed in vivo. Extracts from buguzhi and collagen can be used as bone grafts [35].
Salvia miltiorrhiza Burge (danshen)
Angiogenic disorders, including angina pectoris, heart attacks, and atherosclerosis, are treated with Salvia miltiorrhiza Burge, also known as danshen. Danshen is considered a highly safe TCM. Danshen is mainly composed of hydrophilic compounds containing phenolic acid [36]. Wong et al. compared collagen matrix alone and collagen matrix with danshen extract for bone formation. The parietal bones of New Zealand White rabbits measured 5 mm by 10 mm. The experimental group had six defects grafted with collagen matrix and danshen extract. The collagen matrix alone was used for passive control and the collagen matrix alone for active control. A hematological examination of defects was performed on the 14th day. Each defect was serially cut. Quantitative analysis was done on 100 sections (50 each). Five times more new bone was grafted into defects with danshen extract alone than defects with collagen matrix. In passive controls, no new bone formed. Bone grafts can be performed using danshen extract incorporated into the collagen matrix [37].
Drynaria fortunei (Gusuibu – GSB)
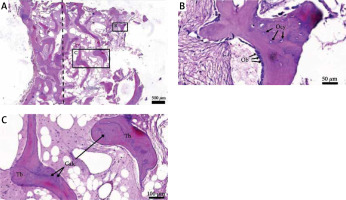
Bone repair is made easier with traditional Chinese medicine. By GSB, BMSCs differentiate into osteogenic cells. The effects of GSB on osteogenic differentiation have been reported in many studies. ALP activity was upregulated by GSB and its marker compound naringin, which confirmed enhanced osteogenesis. While naringin enhances ALP activity, the mechanism by which it binds to receptors remains a mystery. Differentiation of osteoblasts requires BMP. BMP receptor (BMPR) binding triggers BMPR signaling, resulting in cell proliferation and differentiation [38, 39]. Gusuibu has been applied to bone tissue engineering techniques to repair significant bone defects by Dong et al. Surface plasmon resonance (SPR) experiments demonstrated that GSB, naringin, and BMP affect binding. BMP-2 is inhibited by GSB, while BMPR-1B is enhanced by its inhibition. BMP-2 cannot bind to BMPR-1A when naringin is present. An in-vitro study showed that GSB and naringin inhibited BMPR-1A signaling by phosphorylating downstream signals of BMPR and Smad. Through osteoinduction, naringin promoted bone formation via slow and gradual release from GSB scaffolds. Moreover, naringin scaffolds significantly enhanced bone regeneration in rabbit calvarial defects 4 weeks after the implantation. The bone repair can be seen in Figure 3 A, and osteogenesis can be seen to be improved in Figure 3 B. BMP-2 and BMPR-1A can be inhibited by GSB and its marker compound (naringin) by blocking BMPR-1A signaling and enhancing BMPR-1B signaling. Natural BMP regulators such as GSB and naringin may be helpful [20].
Figure 3
Image of implanted Nar scaffold on calvarial bone. A Cont was implanted in calvarial rabbit bone (A) and a Nar scaffold for 4 weeks (B), mCT was used for the radiographs [20]
Grape seed extract (GSE)
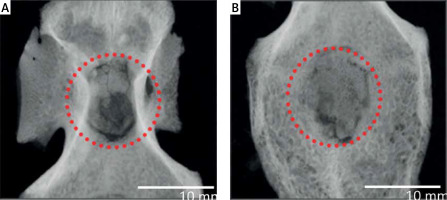
Grape seed extract may also benefit women with estrogen deficiency in orthopedics and dentistry. Implants and bone tissue are connected via osseointegration. The number one choice for orthopedic implants has been titanium and titanium-based alloys. The success of implants depends on osseointegration. The performance of pedicle screws in spinal surgery is affected by the quality of the bone. Titanium implants may adversely affect osseointegration in patients with diseases affecting bone metabolism, such as osteoporosis [19, 40–42]. A study examined the effects of proanthocyanidin-rich grape seed extract (GSE) on bone health in ovariectomized (OVX) rats. Histological and histomorphometric analyses showed that GSE inhibited OVX-induced osteoclastogenesis in the lumbar spine bone of OVX mice. The GSE overcomes the OVX impairment in calvaria healing in rats. GSE promoted bone healing in rats following OVX-induced poor osseointegration by preventing imbalanced bone turnover. OVX + PW (pure water) resulted in a mean implant removal torque of 3.34 N/cm, OVX + GSE resulted in 3.26 N × cm, and Sham with PW was 2.23 N × cm. Sham + PW was significantly different from OVX + PW, but not from Sham + PW + GSE. Figure 4 show the results of histology. All three groups formed new bones between the threads, and the titanium screw directly touched the bone. Compared to the other two groups, the new bone formed in the OVX + PW group contacted the implant less frequently when observed at high magnification. The BIC percentages for the Sham + PW, OVX + PW, and OVX + GSE groups were found to be 68.8%, 45.0%, and 63.8%, respectively, based on the histological images (Figure 4 C). Significant differences were observed between Sham + PW and OVX + PW Sham + PW did not represent any significant differences compared to OVX + GSE, while OVX + PW significantly differed from OVX + GSE. Ovariectomized, a model of estrogen deficiency in the bone, improved implant osseointegration when GSE was administered orally [19].
Figure 4
Effects of grape seed extract (GSE) on ovariectomized (OVX) rats’ implant osseointegration. Installation torque of titanium screw-shaped implants in the tibia (A). When GSE was administered in OVX rats, the implant removal torque was significantly higher than when PW was administered, whereas GSE had no significant effect in sham rats (B). In each group, bone-to-implant contact (BIC) was quantified. C – OVX + PW, OVX + GSE, and Sham + PW histological images at low and high magnifications. White triangles indicate an implant surface without direct bone contact in high magnification images. Images with low and high magnifications are scaled by 100 and 500 μm [19]

Pectin
Because osteoblast activity is essential to osseointegration, it is crucial to investigate and understand how the nanocoating interacts with the cells. Several studies have shown that pectin nanocoatings modulate osteoblast response. Cell adhesion is biospecific thanks to pectin’s chemical structure imitating mammals’ ECM [43]. Enzymatic modification of pectin RG-I (rhamnogalacturonan-I) can control its structure. It is possible to produce a variety of pectin structures by changing the side chains (galactose and arabinose) or the main chains (galacturonic acid and rhamnose). To identify the RG-I regions that are important for bone cells and mineralized matrix formation, multiple RG-I molecules must be screened. As part of their assessment of the osteogenic response of osteoblasts, Folkert et al. coated polystyrene surfaces with potato pectin RG-I that had been enzymatically modified (enriched with galactose side chains). Implant nanocoatings with modified RG-I benefit osteogenesis and osseointegration, making them candidates for nanocoating of bones [16].
Dipterocarpus tuberculatus
Dipterocarpus tuberculatus is a plant in the Dipterocarpaceae family. In Southeast Asia, particularly Cambodia, Thailand, Laos, and Vietnam, it is prescribed for various diseases. Traditionally, this plant is used to treat skin inflammation, asthma, colitis, and anxiety, as well as having leishmanicidal and anti-septic properties. This plant’s heartwood contains several quinone analogs that are considered antioxidants. Several studies have reported that this plant reduces NF-mediated inflammation [44]. Jung et al. coated Ti implants with MED, a natural plant extract. An MED-coated titanium plate and fixture were tested against non-treated and ozone-treated titanium. The MED-coated Ti remained hydrophilic for 20 days, while the ozone-treated Ti turned hydrophobic quickly. Computed tomography and histopathological analysis revealed enhanced bone regeneration with the MED coating. Ti treated with ozone exhibited significantly higher gene expression levels for integrin, a bone cell adhesion receptor. Through MED-mediated cell signaling pathways, MED may be an effective coating agent for Ti implantation [45].
Conclusions
Herbal materials and combinations for bone regeneration have shown great potential in this focused review. However, most results are preliminary, and more systematic in vivo studies are required to determine the fundamental interactions between the materials and plant extracts. Further research is needed on herbal extracts’ biological effects, especially concerning their effectiveness, optimal dosage, and side effects. Combining ancient knowledge with modern biomedical science and engineered biomaterials is possible by using herbal extracts as drug delivery candidates. Although the studies presented in this review show that herbal drugs have great potential for bone and soft tissue repair, many of these studies provide great hope. Herbal materials’ safety, potency, and accuracy must be confirmed before their therapeutic potential can be fully understood. To provide additional evidence of the efficacy and non-toxicity of these traditional remedies, high-excellence clinical trials are needed.