Introduction
Non-communicable diseases (NCDs) have become the leading cause of death and disability worldwide, and cardiovascular disease (CVD) is the leading cause of the burden of NCDs [1]. Among CVDs, ischemic heart disease (IHD) is the most common and a major threat to sustainable development in the 21st century [2, 3]. Population growth and aging have led to an increased global burden of IHD [4]. In 2010, the international number of people with IHD was 7 million, a 35% increase since 1990 [5]. By 2019, the total number of deaths due to IHD had reached 9.14 million globally, accounting for 49.2% of CVD-related deaths [6].
Smoking is the most harmful form of tobacco use [7]. At the same time, smoking is widely recognized as a risk for premature morbidity and mortality, and it has been challenging to adequately detect levels and trends in smoking worldwide [8]. In 2019, there were 1.14 billion current smokers globally. The ten countries with the highest number of smokers (accounting for nearly two-thirds of the global smoking population) were China, India, Indonesia, the United States, Russia, Bangladesh, Japan, Turkey, Vietnam, and the Philippines [9]. Smoking can lead to 36 health consequences, and IHD is the health consequence of smoking that killed the most men and women in 2019 [10].
As the top 5 countries with the highest number of smokers globally, China, India, Indonesia, the United States, and Russia face a higher burden of smoking-induced IHD. However, existing research has focused on a macroscopic perspective or comparison with other countries with similar characteristics, without specifically analyzing the trends and characteristics of ischemic heart disease mortality in high-smoking countries [11–16]. None of the existing studies of IHD mortality due to smoking considered cumulative health risks since birth. None of them comprehensively analyzed the possible reasons behind long-term trends.
Our study utilized data from the Global Burden of Disease (GBD) study 2019 (GBD 2019) to address this knowledge gap, employing a joinpoint regression model and age-period-cohort (APC) analysis. We examined the impact of age, period, and cohort effects on smoking-attributable IHD mortality in the five countries with the highest number of smokers from 1990 to 2019: China, India, Indonesia, the United States, and Russia. Our analysis also allowed us to quantify the individual effects of age, period, and birth cohort. By examining the trends in smoking-induced IHD mortality in these five countries, it is possible to predict the future development of trends under different conditions more accurately. The findings of this research will aid governments in devising targeted strategies to mitigate the burden of preventable smoking-attributable IHD deaths.
Material and methods
Data sources
The data used in this study are from GBD 2019. The GBD 2019 database provides information on deaths and health losses due to 369 diseases, injuries, and defects and 87 risk factors in 204 countries and territories around the globe from 1990 to 2019 [17]. GBD 2019 used population data from the 2012 World Population Prospects Revision (WPPR) for standardization, and the use of age-standardized rates (ASRs) and their 95% uncertainty intervals (UIs) eliminated the effects of variable age distributions across populations and periods, ensuring comparability [18]. Age-standardized rates have been shown to be relatively stable over a given period [19].
Definition of smoking
According to the GBD 2019 Risk Factors Collaborators, to calculate the burden of disease attributable to risk factors, GBD 2019 uses a rule-based synthesis of evidence to provide comparable risk quantification over time and across populations. Cigarette smoking was defined as current or prior use of tobacco products, excluding e-cigarettes and vaporizers. Exposure was estimated using two continuous indicators for current smokers: the number of cigarettes smoked daily and the cumulative number of cigarettes smoked yearly. For those who had quit smoking, exposure was estimated based on the number of years since quitting smoking [10].
Statistical analysis
Joinpoint regression analysis
Determining changes in secular trends is critical to analyzing disease mortality data, and joinpoint regression analysis describes continuous changes in the slope of the overall mortality trend through permutation analysis [20]. Joinpoint regression analysis has been used extensively in previous studies of trends in cardiovascular disease [21]. In our study, using Joinpoint software (version 4.9.1.0) to calculate average percent changes (APCs), average annual percent changes (AAPCs), and the corresponding 95% confidence intervals (CIs) for disease-specific mortality rates, it was possible to analyze the magnitude and direction of difference in IHD mortality attributable to smoking over a 30-year period [22]. All analyses were performed with p < 0.05 as the level of statistical significance.
Age-period-cohort analysis
The age-period-cohort model was developed based on the Poisson distribution to simultaneously estimate the net effect of age, period, and cohort on the trend of IHD deaths [20]. APC analyses to isolate and statistically estimate the differential effects of age, period, and cohort have been widely used to explore social change, disease etiology, aging, and demographic processes and dynamics [23]. The longitudinal age curve represents the age relative risk versus a reference age group in a reference cohort adjusted for period variations. The period (or cohort) rate ratios (RR) indicate the cohort (or period) relative risk adjusted for age and nonlinear period (or cohort) effects in a cohort (or period) versus the reference one [14].
For APC analyses, to avoid overlapping messages in neighboring queues, mortality, and demographic data were categorized into consecutive 5-year age groups, consecutive 5-year periods from 1990 to 2019, and associated consecutive 5-year birth cohorts. The reference groups for all APC analyses were the center age group, period, and birth cohort. Because smoking-attributable deaths in those aged < 30 years were rare in GBD 2019, and individuals > 80 years were recorded as only one group in the GBD database, they were not considered in the APC model. We used the R-based web tool supported by the Division of Cancer Epidemiology and Genetics at the US National Cancer Institute (http://analysistools.nci.nih.gov/apc/) to conduct the APC analysis. To a certain extent, the reduction of confounding factors and biases has been achieved. For the existing limitations of the classic APC model, it is anticipated that more rigorous methods will be employed to address them. The Wald χ2 test was used to test the significance of the estimable function. A two-sided p-value of less than 0.05 was considered significant.
Results
Trends in ASMRs of IHD attributable to smoking
We found an overall downward trend in mortality attributable to smoking globally over more than 30 years, with mortality rates declining from 58.19/100,000 and 16.89/100,000 in 1990 to 35.47/100,000 and 7.41/100,000 in 2019 for both men and women, representing average annual declines of 1.7% and 2.8%, respectively. ASMR for IHD due to smoking declined significantly by 1.1% (95% CI: –1.5%, –0.8%) and 3.5% (95% CI: –3.7%, –3.3%) per year in India and the United States, respectively, with both their male and female mortality due to smoking showing a consistent downward trend. However, significant increases were observed in both China and Indonesia, with substantial increases of 0.4% (95% CI: 0.2%, 0.5%) and 0.8% (95% CI: 0.7%, 0.9%), respectively, and in China, it is noteworthy that the proportionate increase in the number of smoking deaths among females exceeded that of males even. The change in the number of deaths from IHD attributable to smoking in Russia was insignificant. IHD attributable to smoking declined by 0.5% (95% CI: –1.3%, 1.2%) per year in Russian men but maintained an increasing rate of 0.6% per year in women.
Using data on age-standardized rates of GBD in China, India, Indonesia, the United States, Russia, and globally from 1990–2019, the results of the joinpoint regression analyses are shown explicitly in Table I and Figure 1. Only China and Indonesia had AAPCs greater than 0, at 0.5% (95% CI: 0.0%, 1.1%) and 0.8% (95% CI: 0.6%, 1.0%), while India, the United States, and Russia had AAPCs of less than 0, at –0.8% (95% CI: –1.1%, 0.4%), –3.6% (95% CI: –3.8%. –3.4%) and –0.4% (95% CI: –1.4%, 0.6%). Age-standardized mortality rates for IHD attributable to smoking in China, Indonesia, and Russia all showed an increasing and then decreasing trend. In contrast, India and the United States both showed continuing decreasing trends. China had an annual decrease in age-standardized mortality from IHD due to smoking of 0.8% (95% CI: –1.3%, –0.3%) in 2005–2019, and close to this in this period were India, which had an APC of –0.5% in 2004–2019 (95% CI: –0.8%, –0.3%) and Russia 2005–2019 with an APC of –3.4% (95% CI: –4.1%, –2.7%), with Indonesia and the U.S. closer in the last period, Indonesia for 2010–2019 having an APC of –0.2% (95% CI:–0.6%, –0.2%) and the U.S. for 2011–2019 having an APC of –1.5% (95% CI:–2.0%, –1.0%).
Figure 1
Trends in ischemic heart disease mortality in China (A), India (B), Indonesia (C), the United States (D), Russia (E) and globally (F), 1990–2019

Table I
Joinpoint regression analysis of trends in mortality from ischemic heart disease due to smoking in China, India, Indonesia, the United States, Russia, and globally, 1990–2019
| Parameter | Total study period | Period 1 | Period 2 | Period 3 | |||
|---|---|---|---|---|---|---|---|
| AAPC (95% CI) | Years | APC (95% CI) | Years | APC (95% CI) | Years | APC (95% CI) | |
| China | 0.5 (0.0, 1.1) | 1990–1998 | 0.2 (−1.1, 1.6) | 1998–2005 | 3.6 (2.0, 5.3)* | 2005–2019 | −0.8 (−1.3, –0.3)* |
| India | −0.8 (−1.1, –0.4)* | 1990–1998 | −0.1 (−0.8, 0.6) | 1998–2004 | −2.2 (−3.5, –1.0)* | 2004–2019 | −0.5 (−0.8, –0.3)* |
| Indonesia | 0.8 (0.6, 1.0)* | 1990–1998 | 0.4 (−0.0, 0.9) | 1998–2010 | 1.9 (1.6, 2.1)* | 2010–2019 | −0.2 (−0.6, 0.2) |
| USA | −3.6 (−3.8, –3.4)* | 1990–2002 | −3.7 (−3.9, –3.5)* | 2002–2011 | −5.4 (−5.8, –5.0)* | 2011–2019 | −1.5 (−2.0, –1.0)* |
| Russia | −0.4 (−1.4, 0.6) | 1990–1993 | 9.5 (0.6, 19.2)* | 1993–2005 | 0.8 (−0.1, 1.7) | 2005–2019 | −3.4 (−4.1, –2.7)* |
| Global | −2.1 (−2.7, –1.5)* | 1990–1993 | −1.0 (−5.8, 4.1) | 1993–2003 | −2.1 (−3.0, –1.2)* | 2003–2019 | −2.3 (−2.8, –1.8)* |
APC analysis
Net drift represents the overall annual percentage change over the entire study period. Local drift represents the annual percentage change in mortality for each age group relative to net drift (Table II). Trends in net and local drift for the five countries and globally are shown in Figure 2. The Wald χ2 test shows that the trends are all statistically significant. Women showed more of an upward trend in local drift compared to men. Specifically, both net and local drift were less than 0 globally throughout the study period, with a net drift of –1.60 % (95% CI: –1.65%, –1.55%) for men globally and –2.81% (95% CI: –2.90%, –2.72%) for women globally. Also with a net drift that was less than 0 was a net drift rate of –3.62% for men in the United States (95% CI: –3.74%, –3.49%), U.S. females with a net drift of –3.05% (95% CI: –3.19%, –2.90%), Russian males with a net drift of –1.42% (95% CI: –1.59%, –1.25%), Russian females with a net drift of 0.008% (95% CI: –0.28%, –0.27%), Indian males with a net drift of 0.27%), Indian male net drift rate of –0.87% (95% CI: –1.04%, –0.71%), and Indian females with a net drift rate of –1.25% (95% CI: –1.57%, –0.92). The net drift rate for Chinese males was 0.20% (95% CI: 0.04%, 0.35%), for Chinese females the net drift rate was –0.62% (95% CI: –0.96%, –0.28%), there was a net drift rate of 0.63% (95% CI: 0.21%, 1.06%) for Indonesian males, and a net drift rate of 0.53% (95% CI: 0.31%, 0.75%) for Indonesian females.
Figure 2
Local and Net drift in ischemic heart disease mortality rates (A), sex differences (male (B), female (C)) in China, India, The United States, Russia and globally, 1990–2019
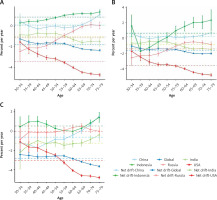
Table II
Local and net drift values for smoking-induced mortality from IHD
Estimates of age, period, and cohort effects on mortality from IHD due to smoking are given in Figure 3. As can be seen from the figure, IHD mortality due to smoking tends to increase with age in all countries. It is also evident from the values in the vertical scale that IHD mortality due to smoking is much higher in males than in females in all age groups. The increase was faster in older participants than younger participants, especially in the male population aged greater than or equal to 65 years (3-D). In contrast, this phenomenon in women occurs in the more youthful group older than or equal to 55 (3-G). For IHD mortality due to smoking, China had the lowest mortality rate in all ages in the interval less than 69 years, and over 69 years, the United States had the lowest. Russia had the highest risk of death at all ages, increasing most rapidly with age.
Figure 3
Parameter estimates of the effect of age, period, and cohort on mortality from smoking-indeuced ischemic heart disease (IHD) in China, India, Indonesia, the United States, and Russia, 1990 to 2019

The period effect of smoking-related IHD mortality has declined globally since 2004. Expressly, period-to-period IHD mortality due to smoking declined globally in the United States, Russia, India, and men, while it increased in China and Indonesia. Although overall, only Indonesian, and Russian females showed increases, after 2014, only Indonesian females showed an increase, while females in the rest of the countries showed a significant decrease.
The cohort effect on IHD mortality due to smoking showed a decreasing pattern in the United States, India, Russia, and globally, and an increasing trend in Indonesia and China. The same trend was observed in both males and females. However, the cohort effect of smoking-caused IHD mortality among males in Indonesia showed a clear downward trend from 1955 to 1984 and an apparent and substantial increase after 1985. Globally, the cohort effect of smoking-related IHD mortality was higher for females than males (Figure 3).
Discussion
This study explored the temporal trends in smoking-attributable IHD mortality in China, India, Indonesia, the United States, and Russia from 1990 to 2019 with the help of joinpoint regression analysis and APC analysis. Against the backdrop of a worldwide decline in mortality from smoking-attributable IHD, more than half of the five countries have experienced an upward trend, even among females in four countries, suggesting that actions taken by the five countries to combat smoking have been less than adequate and that there is room for improvement.
Age effects
The longitudinal age profile of IHD mortality due to smoking increased with age, especially in participants aged 65 years or older. The increase was much higher in Russia than in the other countries studied, with the highest mortality rates for all ages. Russia has one of the highest proportions of smokers among its inhabitants worldwide. Also, it has many passive smokers due to socially tolerant attitudes toward smoking [24]. China and Indonesia also have high mortality rates, especially in the older age groups. China has the lowest mortality rates until age 65 but shows a significant and sudden increase after age 65, with the most significant increase occurring at ages greater than or equal to 75 years. This may be because the fertility peaks of the 1950s and 1970s exacerbated China’s aging process [25]. The increase in IHD deaths attributable to smoking among people aged ≥ 65 years in the United States and India, which are also populous countries and have the most significant number of elderly people, was smaller and lower than the global mortality rate, which may be related to the initiatives of both countries to prohibit smoking in public places strictly. The results of the present study may be due to two reasons: firstly, long-term smoking behavior leads to cardiovascular damage, which increases the risk of IHD deaths, and secondly, the body’s resistance also decreases with age. Therefore, it is necessary to implement strict smoking control measures and encourage smoking cessation as early as possible. By reducing the proportion of smokers, the implementation of smoking bans in public places can significantly reduce the intake of secondhand smoke. Relevant studies have found that age is an important predictor of smoking cessation rates in Japan. The 50–60 age group in Japan has the slowest decline in mortality rates due to smoking, while the mortality rates of young and elderly people have declined more rapidly. This is related to the changing health perceptions and smoking cessation behaviors among elderly people in Japan. According to the United Nations’ World Ageing 2019, greater emphasis should be placed on controlling smoking, aiming to reduce premature deaths caused by non-communicable diseases by one-third through prevention and treatment [14].
Period effects
Our findings show that the period effect of mortality from IHD due to smoking declined over time, except in Indonesia. This phenomenon has been attributed to improvements in health care, health policy announcements, economic influences, increased life expectancy, and improvements in lifestyle and metabolic factor profiles among younger populations. The downward trend is most pronounced in the United States, partly due to its well-developed health care and somewhat because it has been fighting tobacco control for half a century since the White Paper on the Harmful Effects of Tobacco in 1964 [26]. The downward trend is more pronounced in India, where the Global Adult Tobacco Survey also found that tobacco consumption was relatively low in 2009–2010 and 2016–2017. The type of residence and occupation mainly influenced the decline in tobacco consumption. The expected inverse relationship between educational attainment and smoking was also found in existing studies; as the level of education increases, the level of smoking decreases, and the effect of education on smoking was more substantial in 2016–2017 than in 2009–2010. India, meanwhile, was the first of the five countries to take effective tobacco control measures, except for the U.S. In addition to high penalties, India has made it mandatory to print 85 percent of graphic health warnings on all tobacco product packaging [27]. China’s period effect has shown an upward trend since 1990, probably due to the rapid economic development that has changed people’s lifestyles. Still, there has also been a significant decline following a slight increase after 2009. 2012 saw the release of China’s first authoritative report issued by the government that systematically described the health risks of smoking, the China Smoking Hazardous to Health Report, which the World Health Organization hailed as “an important milestone in the history of public health in China.” [28]. Russia has also seen significant declines, with the implementation of an effective tobacco control strategy since 2008 that has resulted in a steady, high-level decline in smoking prevalence among men and women with relatively high levels of education over several decades [29]. Indonesia is the only country with a significant upward trend. It also has one of the highest smoking prevalence rates in the world. Although the Indonesian government has implemented some tobacco control policies since 2007, there is less effective evidence of the positive impact of such policies. Instead, studies have found that cigarette consumption in Indonesia has increased differentially among different socio-demographic groups [30]. In addition, we observed that the period effect is more pronounced for women than men. In particular, smoking prevalence among women in low- and middle-income countries is increasing alarmingly [31]. The increase in the number of female smokers is recognized as a global health challenge [32]. From a global perspective, between 1990 and 2019, the prevalence of smoking among males aged 15 and above significantly decreased in 135 countries (33%), while for females, this decrease was observed in only 68 countries (33%) [10]. As attitudes change with the times, smoking is considered a sign of individuality and group identity [33, 34]. The number of women living alone is increasing and without the influence of family, their willingness to quit smoking is lower [35]. In addition, smoking reduces hunger, which makes more women continue to smoke to control their weight [36]. Also being in a social environment that is more susceptible to anxiety and depression is a barrier to quitting [37]. A study in China found that in 1990, the focus of female tobacco control was passive smoking, but in 2017, smoking and passive smoking became equally crucial for female tobacco control [38]. There is less research on risk factors for female-specific IHD, and related studies have found that passive smokers are more likely to develop IHD, so public health interventions and policy development targeting the female population are necessary [39, 40]. We have observed that with the improvement of living conditions, modern individuals are more focused on present feelings, overlooking the various serious health consequences that smoking may bring. The government should actively promote smoking ban policies; in addition to increasing tax efforts and health promotion education, it should expand into more media, such as the Internet and the implementation of anti-smoking activities, to enhance people’s awareness of the harmful effects of smoking. A study conducted in South Korea revealed that individuals who were exposed to anti-smoking advertisements both online and offline were found to be more willing to quit smoking compared to those who had not attempted to quit [41].
Cohort effects
Cohort RRs reflect the impact of changes in socioeconomic status or risk factors on people born in different years. In our study, most countries reported a downward trend, suggesting a reduced risk of IHD deaths attributable to smoking among younger generations. The downward trend was most pronounced in the United States, whereas China had an upward trend after 1975. In the 1915–1989 birth cohort, India’s cohort RRs declined significantly, while Russia’s cohort RRs maintained a declining trend except for the 1925–1945 cohort RRs, which rose or carried relatively high values. A study in Russia found no correlation between economic indicators and the probability of smoking but between deteriorating social conditions and more northern and colder geography, where females with less education or qualifications and older people were more likely to smoke [42]. A related study examined European countries. A related study examining persistent smoking behavior among older adults in European countries found that women, particularly those with low levels of education, were more likely to be persistent smokers [43]. The same results were obtained in Indonesia, where the overall upward trend was most pronounced, where the cohort RRs maintained a steady upward trend from 1910 to 1982 but showed a downward trend from 1985 to 1989, and where, as the world’s worst tobacco-using country, about 51.3% of adults and 66.2% of adolescents aged 13–15 years are regularly exposed to secondhand smoke [44]. Considering Indonesia’s high exposure to secondhand smoke, passive smokers support more rigorous tobacco control [45], which could also serve as an essential basis for effective tobacco control in Indonesia. An Indian study concluded that it was necessary to raise taxes on tobacco products to reduce their use [46]. It would be more efficient to tailor cessation strategies to the distinctive characteristics of the smoking population. The dissemination of knowledge about the dangerous consequences of smoking should be strengthened for people with low levels of education. Family and school-based education should be strengthened for adolescents, as early exposure to smoking increases the likelihood of smoking and addiction in adulthood, with serious adverse effects. From a global public health perspective, increasing the depth and breadth of compulsory education and emphasizing early preventive and control measures for youth tobacco use would have a profound impact on reducing the global burden of premature deaths caused by tobacco use.
Our study also has some limitations. First, although period and cohort effects were estimated, our age, period, and cohort analyses were based on established data based on GBD 2019, not self-calculated data. Second, data on smoking were self-reported, which may have led to underestimation in countries with lower social acceptance of smoking, particularly among Asian women. Changes in diagnostic criteria and reporting standards during the study period could also have biased our results. Third, the scope of this study focused on smoking tobacco and did not include other forms of harm caused. Fourth, this study is based on country/region-level data from the GBD website and lacks individual data for further detailed analysis [47]. Fifth, our study has limitations as described in GBD 2019.
In conclusion, we found that the mortality trends in these five countries differed significantly and that aggressive anti-smoking policies were necessary. It is also important to consider the increased mortality from IHD among women due to smoking. Given the crucial role of women in the family and society, it is more beneficial to society to pay attention to their physical and mental health needs.