Introduction
Stroke is a leading cause of mortality and disability worldwide, particularly among older populations [1, 2]. Nearly 75% of the global stroke burden is borne by individuals aged 55 years and older [3, 4]. With an aging global population, reducing the stroke burden in this demographic is crucial for mitigating the disease’s public health impact [2]. Physical inactivity is a major modifiable lifestyle risk factor for stroke [2]. Numerous epidemiological studies and clinical trials have demonstrated strong dose-response relationships between physical activity and stroke risk [5, 6]. The Global Burden of Disease Study 2019 highlighted that the burden of high body mass index (BMI) is rising considerably faster than that of low physical activity and poor diet quality globally. This is critical, as increased BMI is often a result of the complex interplay between physical inactivity, excess caloric intake, and poor diet quality. This interconnectivity of risk factors underscores the need for comprehensive prevention strategies [7].
Recent data from the OECD Report 2024 on physical activity patterns among older adults (> 65 years) further emphasizes the critical gap in physical activity levels in this age group, with substantial variations across countries and socioeconomic contexts [8]. This aligns with the growing body of evidence demonstrating the cardiovascular benefits of even modest increases in daily physical activity, including the recent findings that as few as 4000 steps per day can confer significant health benefits [9]. The International Lipid Expert Panel’s SMILE initiative has highlighted the importance of integrating step-based metrics into cardiovascular prevention strategies, particularly for older adults who may find traditional exercise recommendations challenging to achieve [10]. The relationship between physical inactivity and socioeconomic status is complex and multifaceted. While physical activity itself requires minimal financial resources – walking and basic exercises are essentially free – the opportunity to engage in regular physical activity is significantly influenced by socioeconomic factors. Individuals in lower socioeconomic positions often face multiple barriers: longer working hours in physically demanding but sedentary jobs, limited access to safe recreational spaces, lack of time due to multiple job commitments, and inadequate health education about the importance of regular exercise. Furthermore, regional variations in physical activity patterns reflect not only economic disparities but also cultural attitudes toward exercise, urban planning that affects walkability, availability of public transportation, and climate conditions that influence outdoor activities.
Nevertheless, current research lacks precise data on how insufficient exercise affects stroke occurrence in the elderly population. Understanding the relationship between modifiable lifestyle factors and stroke risk in this vulnerable age group is crucial for developing effective public health responses. Our investigation seeks to measure the health impact of sedentary behavior among individuals over 55, examining both mortality rates and disability-adjusted life years using recent global health metrics. Through this detailed analysis of preventable risk factors in senior populations, we aim to contribute valuable insights that can shape evidence-based strategies for stroke prevention and management.
Material and methods
Data sources and case definitions
Our research utilized the Global Burden of Disease (GBD) 2021 database, with full methodological protocols documented in earlier publications [11]. Ischemic stroke was identified using WHO definitions, characterized by neurological deficits resulting from focal vascular insufficiency affecting the brain, spinal cord, or retina [12]. Cases were classified according to both ICD-10 (G45-G46.8, I63-I63.9, I65-I66.9, I67.2-I67.848, I69.3-I69.4) and ICD-9 diagnostic codes (433-435.9, 437.0-437.1, 437.5-437.8). Physical activity levels were categorized as low when participants accumulated less than 3000 Metabolic Equivalent of Task (MET)-minutes weekly, considering all domains including occupational, household, transportation, and leisure-time activities. The Socio-demographic Index (SDI) was used to assess the link between ischemic stroke burden and regional development [13]. The SDI is a composite average of per capita income, average educational attainment, and total fertility rate, all of which are key indicators of a region’s socioeconomic status. The SDI ranges from 0 (least developed) to 1 (most developed). Based on 2021 metrics, all 204 jurisdictions were sorted into five SDI groups: low, low-middle, middle, high-middle, and high. Statistical precision was evaluated through 95% uncertainty intervals, derived from 500 samples using 2.5th and 97.5th percentile values. To comprehensively assess the stroke burden, this study employed three complementary metrics. First, the absolute number of deaths and DALYs reflect the overall scale of the disease burden and its absolute pressure on the public health system, a metric significantly influenced by population growth and aging. Second, the ASDR and age-standardized DALY rate, by eliminating differences in population age structure, allow for a more accurate comparison of the true disease risk and the effectiveness of healthcare interventions across different regions and time points. Third, by combining these metrics with a stratified analysis by the Socio-Demographic Index, we aimed to unravel the complex interplay between epidemiological trends, healthcare advancements, and demographic shifts, and to elucidate the critical role of socioeconomic development in shaping the stroke burden.
Joinpoint regression analysis
To identify significant shifts in stroke patterns over the 1990–2021 timeframe, we performed segmented regression modeling using the joinpoint methodology. The analysis incorporated logarithmic linear functions to detect critical change points, with optimal positions determined through grid-based error minimization. A Monte Carlo testing approach established the appropriate number of inflection points. We calculated yearly change percentages and their averages, including 95% confidence bounds, to quantify trend variations across global and regional development categories.
Decomposition analysis and BAPC model projection
We utilized the Das Gupta decomposition method to dissect the changes in ischemic stroke burden from 1990 to 2021, breaking down the overall shift into three key components: population aging, growth, and epidemiological shifts. This approach surpasses traditional linear regression by precisely quantifying each factor’s unique impact on disease burden changes, offering deep insights into the demographic and epidemiological drivers affecting global ischemic stroke trends.
We employed Bayesian age-period-cohort (BAPC) analysis to forecast future disease patterns, leveraging its capacity to process complex epidemiological datasets [14]. The BAPC model enhances the conventional generalized linear model with a Bayesian framework, dynamically integrating age, period, and cohort effects as continuous temporal processes smoothed by a second-order random walk. Using the “BAPC” R package, we integrated GBD 2021 data with demographic forecasts to predict future ischemic stroke burdens, accounting for the intricate interplay of age, period, and cohort effects.
Results
Deaths
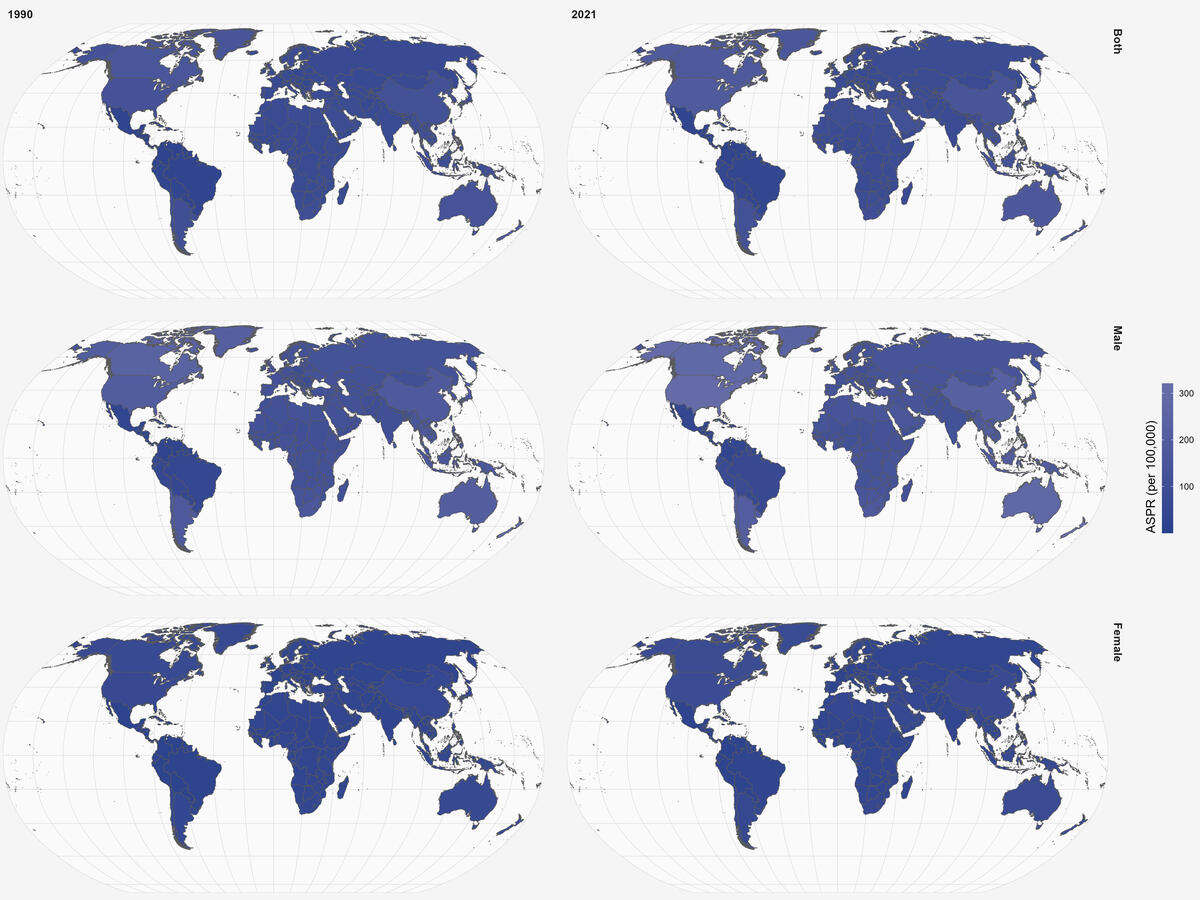
Over a 32-year span from 1990 to 2021, there was a notable shift in the global burden of ischemic stroke attributed to physical inactivity in adults aged 55 and older. Worldwide, the absolute number of deaths rose from 86,434.2 (95% UI: 15,363.7 to 192,041.2) in 1990 to 130,089.1 (95% UI: 40,233.3 to 315,169.4) in 2021 (Table I). However, despite this increase, the age-standardized death rate (ASDR) decreased from 12.9 (95% UI: –2.3 to 28.6) in 1990 to 8.8 (95% UI: –2.7 to 21.2) in 2021, with an EAPC of –1.53 (95% CI: –1.68 to –1.38), indicating a global reduction in ischemic stroke mortality rates after adjustment for population age structure.
Table I
Age-standardized mortality rates of physical inactivity-attributable ischemic stroke among adults aged 55 and above by global and GBD regions, 1990–2021
The trends across socioeconomic status, as measured by the SDI, reveal notable disparities. High SDI regions experienced a significant reduction in both absolute deaths and ASDR. Deaths decreased from 20,455.6 (95% UI: 12,161.6 to 53,521.3) in 1990 to 14,772.7 (95% UI: –14,770.2 to 45,055.1) in 2021, while ASDR dropped from 11 (95% UI: –6.5 to 28.7) to 4.3 (95% UI: –4.3 to 13.1), with an EAPC of –3.46 (95% CI: –3.65 to –3.26), the sharpest decline among all SDI regions. Similarly, high-middle SDI regions showed a substantial decrease in ASDR, from 18 (95% UI: 4.9 to 41.3) in 1990 to 11.6 (95% UI: 5.3 to 30) in 2021, with an EAPC of –1.87 (95% CI: –2.16 to –1.58), although the absolute number of deaths increased slightly, from 31,135.5 (95% UI: –8,534.6 to 71,255.6) to 40,055.3 (95% UI: –18,208.8 to 103,984) over the same period (Table I). Middle SDI regions experienced a marked increase in the number of deaths, rising from 20,989.3 (95% UI: 2,613.2 to 42,026.7) in 1990 to 46,449.3 (95% UI: –6,736.8 to 106,416.1) in 2021. However, the ASDR showed a modest decline, from 12.1 (95% UI: 1.5 to 24.2) to 9.9 (95% UI: –1.4 to 22.6), with an EAPC of -0.81 (95% CI: –0.93 to –0.69). In low-middle SDI regions, the number of deaths more than doubled, increasing from 10,873.3 (95% UI: 1,791.8 to 21,572.9) to 23,450.3 (95% UI: 768.8 to 49,684.9), while the ASDR decreased slightly, from 10.8 (95% UI: 1.8 to 21.4) in 1990 to 9.7 (95% UI: 0.3 to 20.6) in 2021, with an EAPC of –0.42 (95% CI: –0.52 to –0.32), the smallest reduction among all SDI regions. Similarly, in low SDI regions, the number of deaths almost doubled, from 2,843.2 (95% UI: 604.4 to 5,609.1) in 1990 to 5,224.7 (95% UI: 699.4 to 10,867.1) in 2021, while the ASDR decreased from 7.6 (95% UI: 1.6 to 15) to 6.4 (95% UI: 0.9 to 13.2), with an EAPC of –0.68 (95% CI: –0.77 to -0.59).
Regional variations underscore the disparities in ischemic stroke burden due to physical inactivity. Western Europe saw a significant drop in ASDR, decreasing from 14.1 in 1990 to 4.3 in 2021, with an EAPC of –4.03. Australasia also experienced a notable reduction, with ASDR falling from 9.7 to 3.3 over the same period, and an EAPC of –3.87. Southern Latin America showed a substantial decline in ASDR, from 6.9 to 2.9, with an EAPC of –2.58. Conversely, some regions displayed increasing ASDR trends. In Southern Sub-Saharan Africa, ASDR increased from 10.2 to 12.3, with a positive EAPC of 0.54. Southeast Asia exhibited a slight rise in ASDR, from 13 to 13.6, with an EAPC of 0.06. East Asia, despite a significant increase in deaths, saw a modest decline in ASDR, from 12.8 to 11.4, with an EAPC of –0.49. Overall, six regions had higher mortality rates than the global average, while fifteen regions had lower rates (Supplementary Figure S1).
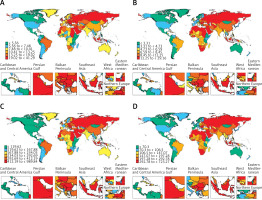
Between 1990 and 2021, ASDR attributed to ischemic stroke caused by physical inactivity decreased significantly in many high-income countries, reflecting advancements in healthcare systems, public health interventions, and lifestyle changes. For example, Austria experienced a substantial reduction in ASDR, from 14.6 per 100,000 in 1990 to 3.1 per 100,000 in 2021, with an EAPC of –5.4 (95% CI: –5.8 to –5.01) (Figures 1 A, B; Supplementary Table SI). Similarly, Germany reduced its ASDR from 13.1 per 100,000 in 1990 to 3.7 per 100,000 in 2021, with an EAPC of –4.0 (95% CI: –4.23 to –3.76) (Figures 1 A, B; Supplementary Table SI). These results suggest effective implementation of preventive measures and increased awareness of physical activity as a modifiable risk factor for ischemic stroke. In contrast, several low- and middle-income countries show slower progress or even increases in ASDR, highlighting persistent disparities in healthcare resources and public health infrastructure. Ethiopia, for instance, experienced a modest decline in ASDR, with an EAPC of –0.87 (95% CI: –0.99 to –0.76), while Indonesia saw an increase in ASDR from 22.1 per 100,000 in 1990 to 26.4 per 100,000 in 2021, with an EAPC of 0.57 (95% CI: 0.26 to 0.88) (Figures 1 A, B; Supplementary Table SI). These trends reflect challenges in addressing physical inactivity and other risk factors in resource-constrained settings, where access to preventive care and public health campaigns may be limited. Regional disparities are further emphasized by countries with minimal or no progress. For instance, Chad’s ASR remained relatively stable, with an EAPC of 0.05 (95% CI: –0.15 to 0.25), while Djibouti saw a slight decline with an EAPC of –0.2 (95% CI: –0.25 to –0.14) (Figures 1 A, B; Supplementary Table SI). These stagnations may be attributed to inadequate healthcare infrastructure, lack of targeted interventions, and competing health priorities in these regions. Overall, the results reveal significant global progress in reducing ischemic stroke mortality due to physical inactivity, particularly in high-income countries. However, the slower reductions and, in some cases, increases in ASDR in low- and middle-income countries highlight the urgent need for equitable health interventions, increased investment in preventive care, and greater emphasis on promoting physical activity in underserved regions. These findings emphasize the importance of addressing regional disparities to further reduce the global burden of ischemic stroke.
DALYs
The global picture reveals that middle-SDI and low-SDI regions continue to bear a substantial burden of ischemic stroke attributable to physical inactivity, with slower reductions in DALYs compared to high-income regions. For example, low-SDI regions show a decline in ASR from 182.5 per 100,000 in 1990 to 147.4 per 100,000 in 2021, with an EAPC of –0.84 (95% CI: –0.93 to –0.75) (Supplementary Table SII), while middle-SDI regions experienced a decline from 281.4 per 100,000 in 1990 to 222.7 per 100,000 in 2021, with an EAPC of –0.94 (95% CI: –1.04 to –0.85). These relatively modest reductions contrast sharply with the high-SDI regions, where the decline in ASR is steeper, from 214.7 per 100,000 in 1990 to 90.9 per 100,000 in 2021, with an EAPC of –3.17 (95% CI: –3.36 to –2.98), underscoring the role of socioeconomic development in reducing the burden of ischemic stroke (Supplementary Table SII). A general decline in age-standardized DALY rates is observed globally, with significant reductions in high-income regions, indicating progress in mitigating the burden of physical inactivity as a risk factor for ischemic stroke. For example, Western Europe shows one of the steepest declines, with ASR decreasing from 248.6 per 100,000 in 1990 to 78.4 per 100,000 in 2021, corresponding to an EAPC of –3.93 (95% CI: –4.11 to –3.75) (Supplementary Table SII). Similarly, the High-Income Asia Pacific region shows a significant reduction in ASR from 234.8 per 100,000 in 1990 to 90.7 per 100,000 in 2021, with an EAPC of –3.49 (95% CI: –3.66 to –3.32), reflecting advancements in health systems, targeted public health interventions, and increased awareness of physical activity. In contrast, regions with lower socioeconomic development exhibit slower progress or relatively minor reductions in DALYs. For instance, the South Asia region shows a modest decline in ASR, from 185.6 per 100,000 in 1990 to 153.5 per 100,000 in 2021, with an EAPC of –0.95 (95% CI: –1.10 to –0.80), while Sub-Saharan Africa demonstrates considerable variability across subregions. Eastern Sub-Saharan Africa, for example, experienced a slight reduction in ASR from 106.3 per 100,000 in 1990 to 92.6 per 100,000 in 2021, with an EAPC of –0.56 (95% CI: –0.60 to –0.52), whereas Southern Sub-Saharan Africa saw an increase in ASR from 253 per 100,000 in 1990 to 287.8 per 100,000 in 2021, with an EAPC of 0.3 (95% CI: –0.14 to 0.75), indicating a concerning rise in the burden of ischemic stroke in this subregion (Supplementary Table SII). Regions such as Southeast Asia and Western Sub-Saharan Africa highlight stagnation or very limited progress in reducing age-standardized DALY rates. In Southeast Asia, ASR remained nearly unchanged, with a slight increase from 318.8 per 100,000 in 1990 to 327.5 per 100,000 in 2021, resulting in an EAPC of –0.04 (95% CI: –0.23 to 0.15), emphasizing the persistent burden of physical inactivity as a risk factor for ischemic stroke in this region. Meanwhile, Western Sub-Saharan Africa showed a minor reduction in ASR from 237.8 per 100,000 in 1990 to 195.7 per 100,000 in 2021, with an EAPC of –0.68 (95% CI: –0.77 to –0.59), which reflects the continuing challenges in addressing the underlying determinants of physical inactivity in this subregion. Eight regions had higher DALY rates than the global mean, whereas 13 regions had lower rates than the global mean (Supplementary Figure S2).
Geographically, significant reductions in ASR were observed in many high-income countries, reflecting the success of public health interventions aimed at promoting physical activity and stroke prevention. For instance, Austria demonstrated a reduction in ASR from 248.4 in 1990 to 69.8 in 2021, with an EAPC of –4.29 (95% CI: –4.64 to –3.94). Similarly, Australia exhibited a decline from 190 in 1990 to 65.1 in 2021, with an EAPC of –3.84 (95% CI: –4.05 to –3.62) (Figures 1 C, D, Supplementary Table SIII). These consistent reductions in high-income regions highlight the effectiveness of widespread awareness campaigns, improved healthcare infrastructure, and advanced stroke prevention strategies. In contrast, many low- and middle-income countries continue to exhibit a high burden of physical inactivity-attributable ischemic stroke. Afghanistan, for example, reported an ASR of 670.5 in 1990, which only marginally decreased to 625.7 in 2021, with a negligible EAPC of –0.14 (95% CI: –0.31 to 0.04) (Figures 1 C, D, Supplementary Table SIII). Similarly, countries such as Cameroon and Lesotho saw increases in the burden, with Cameroon reporting a positive EAPC of 0.38 (95% CI: –0.07 to 0.84). These findings point to challenges in addressing physical inactivity and its associated health consequences in resource-constrained settings. Population size and demographic shifts play a critical role in the absolute burden of DALYs. For instance, China and India, which represent a significant proportion of the global population, reported substantial absolute DALYs in 2021. China recorded 968,272.1 DALYs in 2021, up from 431,776.7 in 1990, despite a decline in ASR from 300.9 to 255.5 (EAPC: –0.65, 95% CI: –0.81 to –0.49). Similarly, India reported an increase in absolute DALYs from 138,427.4 in 1990 to 296,274.8 in 2021, accompanied by a reduction in ASR from 180.6 to 147.4 (EAPC: –1.05, 95% CI: –1.22 to –0.87). These trends highlight the dual challenge of managing population growth and addressing the rising healthcare demands of aging populations in these countries. High-income countries generally demonstrated larger reductions in ASR compared to low-income regions. For example, Germany achieved an EAPC of –3.49 (95% CI: –3.73 to –3.26), while Sub-Saharan African nations such as Burkina Faso and Eritrea showed minimal reductions, with EAPCs of 0.06 (95% CI: –0.03 to 0.15) and –0.37 (95% CI: –0.45 to –0.28), respectively. These discrepancies underscore the need for targeted interventions to reduce the burden of physical inactivity in low-resource settings. Some countries showed unique trends due to specific demographic or healthcare factors. For example, Andorra, a small high-income country, reported a significant decline in ASR from 97.9 in 1990 to 52.6 in 2021, with an EAPC of –1.97 (95% CI: –2.17 to –1.77). Conversely, small island nations such as Fiji and Kiribati maintained high ASRs throughout the period, with EAPCs of –0.8 (95% CI: –0.91 to –0.69) and –0.38 (95% CI: –0.45 to –0.32), respectively. Such trends may reflect limited healthcare resources, unique lifestyle factors, and geographic challenges in these regions.
Globally, the dataset highlights substantial progress in reducing the burden of physical inactivity-attributable ischemic stroke, particularly in high-income regions. However, persistent disparities remain, with slower progress observed in low- and middle-income countries. These findings underscore the importance of tailored public health strategies that address regional differences in healthcare access, promote physical activity, and implement effective stroke prevention programs. Further research is needed to investigate the socio-economic, cultural, and policy-related factors influencing these trends, particularly in regions with stagnating or increasing burdens.
Joinpoint regression analysis
The Joinpoint regression model analysis of ischemic stroke mortality and DALY burden showed varied global and SDI regional patterns (Figure 2, Supplementary Table SIV). Globally, ischemic stroke deaths exhibited a downward trend (AAPC = –1.54), with different phases of decline: a slight decrease from 1990 to 1994 (APC = –0.37), a sharper reduction from 1994 to 2003 (APC = –1.33), and a moderate decline from 2013 to 2021 (APC = –0.98). Across SDI regions, the trend began with a rapid decline, then slowed. High SDI regions had the steepest decline (AAPC = –3.58), with increasingly steep reductions from 1990–1999 (APC = –3.11) to 1999–2012 (APC = –4.97), then a more moderate decline from 2012 to 2021 (APC = –2.01). For DALYs, the global trend has been a consistent downward slope (AAPC = –3.33). The decline was steady from 1990 to 1995 (APC = –2.89), continued through 1995–2004 (APC = –3.36) and 2004–2016 (APC = –2.70), before seeing a significant acceleration from 2016 to 2019 (APC = –4.87) and 2019 to 2021 (APC = –5.65). High-SDI regions have experienced the most notable overall decrease (AAPC = –2.95), with the rate of decline intensifying from 1990–1998 (APC = –2.67) to 1998–2012 (APC = –4.20), and then slowing from 2012 to 2021 (APC = –1.25).
Decomposition analysis
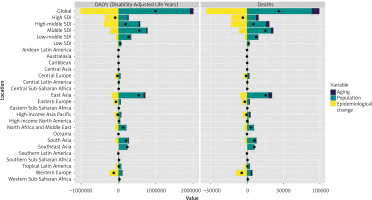
Using decomposition methods, we analyzed how aging demographics, population dynamics, and epidemiological shifts influenced stroke patterns from 1990 to 2021 (Figure 3). For DALYs, the global analysis indicated that population growth and aging significantly increased the disease burden, contributing 192.85% and 9.41%, respectively. These impacts varied across SDI regions. In high SDI regions, aging (–34.79%) and population growth (–281.97%) had negative contributions, whereas other SDI regions showed positive contributions from both factors. Population growth was the main driver in most regions, while epidemiological changes helped reduce the disease burden. Similar patterns were observed for mortality, with global population growth and aging contributing 203.33% and 23.9%, respectively, to the increase in disease-related deaths. Except for high SDI regions, all SDI regions showed positive contributions from both population growth and aging to the disease mortality burden, aligning with the DALY analysis.
Figure 3
Population-level determinant analysis of ischemic stroke burden attributable to physical inactivity among adults aged 55 and above, 1990–2021. Contributions of aging, population growth, and epidemiological changes are shown, with black dots representing the total net change. Positive values indicate increases in disease burden, while negative values represent decreases
Age and sex patterns
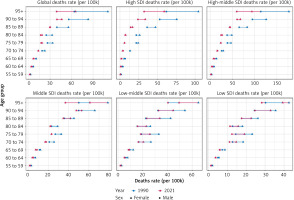
In 2021, death rates exhibited distinct patterns across different SDI regions and age groups, with notable gender disparities (Figure 4). Globally, death rates increased progressively with age (Figure 4). The gender disparity was particularly pronounced in the 95+ age groups. In high SDI regions, death rates were generally lower compared to other SDI categories, though following a similar age-related increasing trend. In low-middle and low SDI regions, while the age-related increase in death rates persisted, the gender disparity was more pronounced compared to higher SDI regions. Between 1990 and 2021, death rates generally decreased across all SDI regions, with the most notable reductions observed in the high and high-middle SDI regions. This temporal improvement was more evident in the younger age groups (55–69 years) compared to the older age brackets (80+ years). Following the mortality patterns, DALY rates also showed significant variations across SDI regions and age groups, with distinct temporal trends between 1990 and 2021 (Supplementary Figure S3). The global DALY burden demonstrated a consistent age-related increase, with females generally experiencing higher rates than males, particularly pronounced in the 90+ age groups. High SDI regions exhibited lower overall DALY rates compared to other SDI categories, though maintaining the gender disparity pattern, with the gap most notable in the 90+ age brackets. Middle SDI regions displayed similar age-related progression but with comparatively moderate gender differences. In low-middle and low SDI regions, while the overall DALY rates were higher than in high SDI regions, the gender gap was more pronounced, suggesting a less equitable distribution of disease burden between males and females. Notably, there was a considerable reduction in DALY rates from 1990 to 2021 across all SDI regions, with the most substantial improvements observed in high and high-middle SDI regions, particularly among the younger age groups (55–69 years).
BAPC model
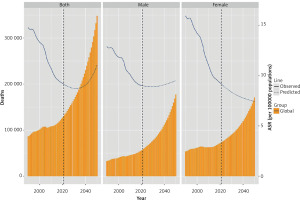
Using the BAPC model to predict the disease burden of ischemic stroke attributable to physical inactivity from 2021 to 2050, our analysis revealed significant trends in mortality and DALYs. The global death toll is projected to reach 348,153 by 2050, with 177,148 males and 171,005 females. The global ASDR is expected to demonstrate a U-shaped trend, initially decreasing before rising to 11 per 100,000 by 2050, while the female ASDR shows a consistent declining trend, reaching 7 per 100,000 by 2050 (Figure 5). Regarding the disability burden, the global age-standardized DALY rates are projected to reach 249 per 100,000 by 2050, with notable gender differences: males are expected to experience higher rates at 211 per 100,000 compared to females at 185 per 100,000 (Supplementary Figure S4).
Discussion
This study revealed a complex and profound relationship between the burden of ischemic stroke attributable to physical inactivity and socioeconomic development. A core finding of our research is the divergent trend between the absolute burden (e.g., total number of deaths) and age-standardized rates (e.g., ASDR), a disparity that highlights the critical interplay between demographic shifts and epidemiological factors. Specifically, as confirmed by our decomposition analysis, the growing global population and its progressive aging are the primary drivers behind the increase in the absolute number of deaths and DALYs. However, the general downward trend in global ASDR indicates that, after controlling for demographic factors, substantial progress has indeed been made in stroke prevention and medical care worldwide.
Crucially, this progress has been unevenly distributed across SDI regions. High-SDI regions have achieved the most significant success in reducing ASDR, where the positive effects of public health interventions and medical advancements have even outweighed the pressures of population aging. In stark contrast, progress in low- and low-middle-SDI regions has been much slower. Their limited medical advancements are far from sufficient to counteract the immense challenges posed by population growth, leading to a persistently increasing overall disease burden. This discussion will further dissect these findings, exploring the disparities across SDI regions, the temporal trends, and their implications for future public health policy [15]. The observed decline in global ASDR from 12.9 per 100,000 in 1990 to 8.8 per 100,000 in 2021 represents a noteworthy achievement in public health, reflecting the cumulative impact of improved healthcare systems, enhanced awareness of physical activity benefits, and successful implementation of preventive strategies [16]. The striking disparities between high- and low-SDI regions merit particular attention, as they reflect broader inequalities in healthcare access and resources [17]. High-SDI regions have demonstrated remarkable success in reducing both mortality and DALYs, with some areas achieving EAPC values exceeding –3.0, indicating substantial and consistent improvements over the study period. This success can be attributed to multiple factors, including well-developed healthcare infrastructure, robust public health systems, effective health education programs, and widespread access to preventive services. The experience of countries such as Austria and Germany, which achieved impressive reductions in ASDR, provides valuable insights into successful approaches to addressing physical inactivity and its associated stroke burden. In contrast, the slower progress or, in some cases, increasing burden observed in low- and middle-SDI regions points to persistent challenges in addressing physical inactivity and its health consequences [18, 19]. The situation in regions such as Southern Sub-Saharan Africa and Southeast Asia, where ASDR have either increased or remained relatively stable, highlights the complex interplay of factors hampering progress. These regions often face multiple challenges, including limited healthcare resources, inadequate public health infrastructure, competing health priorities, and socioeconomic constraints that may limit individuals’ ability to engage in regular physical activity [20].
The Joinpoint regression analysis revealed distinct temporal trends in ischemic stroke deaths and DALY burden. The overall declining trend, with variations in the rate of decline over time, suggests the influence of evolving healthcare practices, technological advancements, and shifts in lifestyle behaviors. The more substantial declines observed in high-SDI regions may be attributed to better access to preventive care, advanced stroke management, and effective health promotion strategies.
Decomposition analysis revealed that population growth and aging have significantly contributed to the rising ischemic stroke burden, particularly in low- and middle-SDI regions. The impact of demographic transitions in shaping the burden of ischemic stroke attributable to physical inactivity is profound and cannot be overstated [21]. This finding emphasizes the need for health systems to adapt and scale up services to meet the growing demands of aging populations. The beneficial impact of epidemiological changes in reducing disease burden across most regions suggests the effectiveness of interventions targeting modifiable risk factors, such as physical inactivity. The experience of countries such as China and India, which have seen significant increases in absolute DALYs despite modest improvements in age-standardized rates, illustrates the complex challenges faced by nations experiencing rapid demographic transitions [22].
The analysis reveals important patterns in the relationship between socioeconomic development and health outcomes. The consistent gradient observed across SDI quintiles, with high-SDI regions achieving the most substantial improvements and low-SDI regions showing the least progress, suggests that economic development plays a crucial role in determining health outcomes. It is crucial to deconstruct what “regional development”, as measured by SDI, means for an individual’s health. The SDI is built on three pillars: income, education, and fertility rates (as a proxy for overall health system development). From an individual’s perspective, these are not abstract numbers. Higher income translates into better access to preventive healthcare, more nutritious food choices, and safer environments for physical activity, such as well-lit parks and affordable gyms. Higher educational attainment fosters greater health literacy, enabling individuals to better understand and act upon public health recommendations regarding diet and exercise. Finally, a developed health system (indicated by lower fertility rates) means better access to organized stroke prevention programs, rapid-response emergency care, and comprehensive post-stroke rehabilitation. Therefore, the disparities in stroke burden we observe across SDI quintiles are a direct reflection of these tangible inequalities in resources, knowledge, and infrastructure. Addressing the burden of inactivity-related stroke, especially in low- and middle-SDI regions, requires policies that go beyond health education to tackle these fundamental socioeconomic determinants of health.
To address how healthcare resources and public health infrastructure concretely affect an individual’s daily physical activity, it is useful to consider the connection from two perspectives. First, there are direct interactions with the healthcare system. In a high-resource setting, a routine check-up is more likely to include personalized physical activity counseling, where a doctor not only recommends exercise but might also provide a specific plan or a referral to an affordable community program. For a person recovering from a minor stroke, a well-funded system provides access to comprehensive rehabilitation that includes structured, supervised exercise, which is crucial for building confidence and safely regaining mobility.
Second, and perhaps more pervasively, public health infrastructure shapes the everyday environment. This extends beyond the hospital walls. For an ordinary person, this translates into having access to safe, well-lit parks and public recreational spaces for walking or jogging. It means the availability of community-based wellness programs, such as free Tai Chi classes for seniors or organized walking groups. Furthermore, robust public health infrastructure promotes health literacy through widespread, accessible campaigns that build a societal culture where physical activity is valued and encouraged. In contrast, in lower-resource settings, these supportive systems are often absent, leaving individuals to navigate barriers such as unsafe neighborhoods, lack of public spaces, and limited access to professional health guidance on their own.
However, this relationship is not purely deterministic, as evidenced by variations in performance among countries within the same SDI category. Based on our findings, several evidence-based strategies should be implemented to increase physical activity levels among older adults. The International Lipid Expert Panel (ILEP) recently provided comprehensive recommendations through the SMILE initiative, emphasizing a holistic approach to cardiovascular prevention that includes structured physical activity programs. Healthcare systems should prioritize community-based exercise programs tailored for older adults, particularly in low-SDI regions where the burden remains high, while integrating physical activity counseling into routine clinical care. The development of age-appropriate infrastructure and culturally sensitive interventions that address region-specific barriers is essential for promoting sustainable behavior change. Importantly, recent evidence suggests that cardiovascular benefits can be achieved at more attainable thresholds, with as few as 4000 steps per day conferring significant health benefits, making physical activity goals more accessible for older adults. The marked reductions in stroke burden observed in high-SDI regions demonstrate that systematic approaches combining policy interventions, healthcare system engagement, and community programs can effectively address physical inactivity and its associated health consequences.
Gender disparities in the burden of ischemic stroke attributable to physical inactivity represent another important dimension of the analysis. These differences, which are particularly pronounced in older age groups and low-SDI regions, reflect complex interactions between biological factors, sociocultural norms, and healthcare access. The more pronounced gender disparities in low- and middle-SDI regions may be attributed to socio-cultural factors, limited access to healthcare, and gender-based inequalities in health-seeking behaviors [23]. Understanding and addressing these gender-specific patterns requires careful consideration of cultural contexts and the development of targeted interventions that account for gender-specific barriers to physical activity and healthcare access [24, 25].
The success of high-income regions in reducing stroke burden provides valuable lessons for global health policy, while also highlighting the challenges of translating these successes to different contexts. The dramatic reductions achieved in regions such as Western Europe and Australasia demonstrate the potential impact of well-designed and adequately resourced public health interventions. However, the minimal progress observed in many low- and middle-income regions suggests that simply transplanting successful interventions from high-income contexts may not be sufficient.
Furthermore, as astute commentary on our initial submission pointed out, it is crucial to recognize that physical inactivity does not exist in a vacuum. Our findings, which focus on this single risk factor, should be contextualized within a broader web of interconnected lifestyle behaviors. The GBD 2019 study, for instance, emphasizes that the burden of high BMI is escalating rapidly, driven by a combination of physical inactivity, excess caloric intake, and poor diet quality [7]. This is particularly relevant to the disparities we observed across SDI regions. In low- and middle-SDI regions, promoting physical activity alone may be insufficient if not coupled with strategies to address the ‘nutrition transition’ – the increasing availability of inexpensive, high-calorie, nutrient-poor foods. Therefore, future public health initiatives must adopt a holistic approach, integrating physical activity promotion with nutritional education and policies that improve the food environment to effectively reduce the stroke burden.
The pronounced gender disparities observed in our study, particularly among older age groups and in low-SDI regions, warrant deeper consideration as they intersect with policy and future research. These differences likely stem from a complex interplay of biological, sociocultural, and healthcare system factors. Biologically, post-menopausal hormonal changes in women may alter cardiovascular risk profiles. Socioculturally, traditional gender roles, caregiving responsibilities, and disparities in economic autonomy can create different patterns of and barriers to physical activity. Acknowledging these multifaceted drivers is essential for developing effective interventions, which leads to clear implications for future work and policy making. For future research, it is crucial to move beyond large-scale data to conduct longitudinal and qualitative studies in low-SDI regions, exploring these gender-specific barriers and testing the cost-effectiveness of culturally-adapted interventions, such as those delivered via community health workers or mHealth platforms. For health policy, our findings underscore the need for a multi-pronged approach. Governments should not only integrate “Physical Activity as a Vital Sign” into primary care but also invest in safe, senior-friendly public infrastructure. Crucially, public health initiatives must be gender-sensitive – for instance, by creating women-only exercise groups to address cultural barriers – and embedded within a broader “Health in All Policies” framework that aligns urban planning and social welfare to support active aging for all.
Several limitations of our study warrant consideration. First, our analysis relied on data from the GBD 2021 study, which, despite its comprehensive nature, may have inherent data quality variations across different regions and time periods. The accuracy of stroke burden estimates could be affected by differences in diagnostic capabilities and reporting systems across countries. Second, the definitions of low physical activity used in this study may not fully capture the complexity of these risk factors. The threshold for low physical activity (< 3000 MET minutes per week) may not be equally applicable across different populations and cultures, particularly considering ethnic variations in body composition and physical activity patterns. Third, the projections for future burden rely on current trends and patterns, which may not accurately reflect future changes in healthcare systems, intervention strategies, or population behaviors. Unforeseen factors such as technological advances or changes in healthcare policies could significantly impact these projections.
In conclusion, the global burden of ischemic stroke attributable to physical inactivity among adults aged 55+ showed mixed trends from 1990 to 2021. While absolute deaths increased from 86,434 to 130,089, ASDR declined globally, particularly in high-SDI regions. Significant disparities exist between regions, with high-income countries showing substantial improvements while low- and middle-income countries experienced slower progress or even increases in burden. Population growth and aging were major contributors to increased disease burden in most regions, though epidemiological changes helped reduce the overall burden. These findings highlight the need for targeted interventions in resource-limited settings and emphasize the importance of addressing regional disparities in healthcare access and physical activity promotion.