Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
CARDIOLOGY / STATE OF THE ART PAPER
Gut microbiota and the pathophysiology of cardiovascular disease
1
University Medical Centre Maribor, Maribor, Slovenia
2
Medical Faculty, University of Maribor, Maribor, Slovenia
3
Diagnostic and Research Institute of Pathology, Graz, Austria
4
Institute of Biomedical Sciences, Medical Faculty, University of Maribor, Maribor, Slovenia
Submission date: 2020-05-16
Final revision date: 2020-08-30
Acceptance date: 2020-09-02
Online publication date: 2021-03-21
Corresponding author
Kristijan Skok
Diagnostic and Research Institute of Pathology Neue Stiftingtalstraße 6 8010, Graz, Austria
Diagnostic and Research Institute of Pathology Neue Stiftingtalstraße 6 8010, Graz, Austria
KEYWORDS
TOPICS
ABSTRACT
In recent years, significant findings have emerged concerning the association between the gut microbiota and various human diseases. The diversity can be explained by a multitude of interactions between intrinsic and environmental factors that are unique to each individual. This uniqueness of the microbiota may explain why some individuals are more prone to develop cardiovascular diseases. Gut dysbiosis plays a significant role in various pathophysiological processes. It can be postulated that health is linked to the homeostasis of the gastrointestinal microbiota. We provide an overview of diagnostic procedures to determine the microbiota’s composition, the mechanisms of microbiota interactions and some effects of the microbiota on the development of cardiovascular diseases.
REFERENCES (83)
1.
Lau K, Srivatsav V, Rizwan A, et al. Bridging the gap between gut microbial dysbiosis and cardiovascular diseases. Nutrients 2017; 9: 859.
2.
Vangay P, Johnson AJ, Ward TL et al. US immigration westernizes the human gut microbiome. Cell 2018; 175: 962-72.e10.
3.
Lauderdale DS, Rathouz PJ. Body mass index in a US national sample of Asian Americans: effects of nativity, years since immigration and socioeconomic status. Int J Obes 2000; 24: 1188-94.
4.
Hills RD, Pontefract BA, Mishcon HR, Black CA, Sutton SC, Theberge CR. Gut microbiome: profound implications for diet and disease. Nutrients 2019; 11: 1613.
5.
Rothschild D, Weissbrod O, Barkan E et al. Environment dominates over host genetics in shaping human gut microbiota. Nature 2018; 555: 210-5.
6.
Szychlinska MA, Di Rosa M, Castorina A, Mobasheri A, Musumeci G. A correlation between intestinal microbiota dysbiosis and osteoarthritis. Heliyon 2019; 5: e01134.
7.
Xu H, Wang X, Feng W, et al. The gut microbiota and its interactions with cardiovascular disease. Microb Biotechnol 2020; 13: 637-56.
8.
Nallu A, Sharma S, Ramezani A, Muralidharan J, Raj D. Gut microbiome in chronic kidney disease: challenges and opportunities. Transl Res 2017; 179: 24-37.
9.
Tang WHW, Wang Z, Levison BS, et al. Intestinal microbial metabolism of phosphatidylcholine and cardiovascular risk. N Engl J Med 2013; 368: 1575-84.
10.
Ismail NA, Ragab SH, ElBaky AA, Shoeib ARS, Alhosary Y, Fekry D. Frequency of Firmicutes and Bacteroidetes in gut microbiota in obese and normal weight Egyptian children and adults. Arch Med Sci 2011; 7: 501-7.
11.
Tang WHW, Kitai T, Hazen SL. Gut microbiota in cardiovascular health and disease. Circ Res 2017; 120: 1183-96.
12.
Sekirov I, Russell SL, Antunes LCM, Finlay BB. Gut microbiota in health and disease. Physiol Rev 2010; 90: 859-904.
13.
Tamburini S, Shen N, Wu HC, Clemente JC. The microbiome in early life: implications for health outcomes. Nat Med 2016; 22: 713.
14.
Šket R, Prevoršek Z, Košeto D, et al. Analitski in konceptualni izzvi pri raziskovanju človeške mikrobiote za potrebe personalizirane večnivojske medicine. Med Razgl 2019; 58: 211-34.
15.
Marchesi JR, Ravel J. The vocabulary of microbiome research: a proposal. Microbiome 2015; 3: 31.
16.
Durack J, Lynch SV. The gut microbiome: relationships with disease and opportunities for therapy. J Exp Med 2019; 216: 20-40.
17.
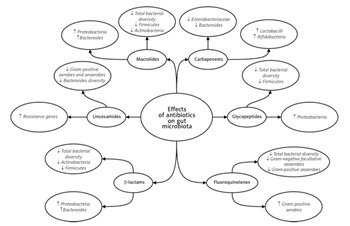
Turnbaugh PJ, Ley RE, Hamady M, et al. The human microbiome project. Nature. 2007; 449: 804-10.
18.
Qin J, Li R, Raes J, et al. A human gut microbial gene catalogue established by metagenomic sequencing. Nature 2010; 464: 59-65.
19.
Yamashiro K, Tanaka R, Urabe T et al. Gut dysbiosis is associated with metabolism and systemic inflammation in patients with ischemic stroke. PLoS One 2017; 12: e0171521.
20.
Qi Y, Aranda JM, Rodriguez V, Raizada MK, Pepine CJ. Impact of antibiotics on arterial blood pressure in a patient with resistant hypertension – a case report. Int J Cardiol 2015; 201: 157-8.
21.
Niebauer J, Volk H-D, Kemp M, et al. Endotoxin and immune activation in chronic heart failure: a prospective cohort study. Lancet 1999; 353: 1838-42.
22.
Gomez-Arango LF, Barrett HL, McIntyre HD, et al. Increased systolic and diastolic blood pressure is associated with altered gut microbiota composition and butyrate production in early pregnancy. Hypertension 2016; 68: 974-81.
23.
Cani PD, Amar J, Iglesias MA, et al. Metabolic Endotoxemia Initiates Obesity and Insulin Resistance. Diabetes 2007; 56: 1761-72.
24.
Brown JM, Hazen SL. The gut microbial endocrine organ: bacterially derived signals driving cardiometabolic diseases. Annu Rev Med 2015; 66: 343-59.
25.
Koren O, Spor A, Felin J et al. Human oral, gut, and plaque microbiota in patients with atherosclerosis. Proc Natl Acad Sci USA 2011; 108 (Suppl. 1): 4592-8.
26.
Ott SJ, El Mokhtari NE, Musfeldt M et al. Detection of diverse bacterial signatures in atherosclerotic lesions of patients with coronary heart disease. Circulation 2006; 113: 929-37.
27.
Lam V, Su J, Hsu A, Gross GJ, Salzman NH, Baker JE. Intestinal microbial metabolites are linked to severity of myocardial infarction in rats. PLoS One 2016; 11: e0160840.
28.
Gan XT, Ettinger G, Huang CX, et al. Probiotic administration attenuates myocardial hypertrophy and heart failure after myocardial infarction in the rat. Circ Hear Fail 2014; 7: 491-9.
29.
Abdelsalam L, Ibrahim AA, Shalaby A et al. Expression of miRNAs-122, -192 and -499 in end stage renal disease associated with acute myocardial infarction. Arch Med Sci 2019; 15: 1247-53.
30.
Gansevoort RT, Correa-Rotter R, Hemmelgarn BR, et al. Chronic kidney disease and cardiovascular risk: epidemiology, mechanisms, and prevention. Lancet 2013; 382: 339-52.
31.
Shi K, Wang F, Jiang H et al. Gut bacterial translocation may aggravate microinflammation in hemodialysis patients. Dig Dis Sci 2014; 59: 2109-17.
32.
Lin C-J, Chen H-H, Pan C-F et al. p-Cresylsulfate and indoxyl sulfate level at different stages of chronic kidney disease. J Clin Lab Anal 2011; 25: 191-7.
33.
Tang WHW, Wang Z, Kennedy DJ, et al. Gut microbiota-dependent trimethylamine N-oxide (TMAO) pathway contributes to both development of renal insufficiency and mortality risk in chronic kidney disease. Circ Res 2015; 116: 448-55.
34.
Tang WHW, Wang Z, Fan Y, et al. Prognostic value of elevated levels of intestinal microbe-generated metabolite trimethylamine-N-oxide in patients with heart failure: refining the gut hypothesis. J Am Coll Cardiol 2014; 64: 1908-14.
35.
Rhee EP, Clish CB, Ghorbani A, et al. A combined epidemiologic and metabolomic approach improves CKD prediction. J Am Soc Nephrol 2013; 24: 1330-8.
36.
Zhu Q, Gao R, Zhang Y, et al. Dysbiosis signatures of gut microbiota in coronary artery disease. Physiol Genomics 2018; 50: 893-903.
37.
Zhernakova A, Kurilshikov A, Bonder MJ, et al. Population-based metagenomics analysis reveals markers for gut microbiome composition and diversity. Science 2016; 352: 565-9.
38.
Belizário JE, Faintuch J. Microbiome and gut dysbiosis. I Exp Suppl 2018; 109: 459-76.
39.
Kriss M, Hazleton KZ, Nusbacher NM, Martin CG, Lozupone CA. Low diversity gut microbiota dysbiosis: drivers, functional implications and recovery. Curr Opin Microbiol 2018; 44: 34-40.
40.
Mahnic A, Rupnik M. Different host factors are associated with patterns in bacterial and fungal gut microbiota in Slovenian healthy cohort. PLoS One 2018; 13: e0209209.
41.
Mahnic A, Breskvar M, Dzeroski S, Skok P, Pintar S, Rupnik M. Distinct types of gut microbiota dysbiosis in hospitalized gastroenterological patients are disease non-related and characterized with the predominance of either Enterobacteriaceae or Enterococcus. Front Microbiol 2020; 11: 120.
42.
Kazemian N, Mahmoudi M, Halperin F, Wu JC, Pakpour S. Gut microbiota and cardiovascular disease: opportunities and challenges. Microbiome 2020; 8: 36.
43.
Threapleton DE, Greenwood DC, Evans CEL, et al. Dietary fibre intake and risk of cardiovascular disease: systematic review and meta-analysis. BMJ 2013; 347: f6879.
44.
Aljuraiban GS, Griep LMO, Chan Q et al. Total, insoluble and soluble dietary fibre intake in relation to blood pressure: the INTERMAP Study. Br J Nutr 2015; 114: 1480-6.
45.
Ghosh TS, Rampelli S, Jeffery IB, et al. Mediterranean diet intervention alters the gut microbiome in older people reducing frailty and improving health status: the NU-AGE 1-year dietary intervention across five European countries. Gut 2020; 69: 1218-28.
46.
Marques FZ, Nelson E, Chu PY, et al. High-fiber diet and acetate supplementation change the gut microbiota and prevent the development of hypertension and heart failure in hypertensive mice. Circulation 2017; 135: 964-77.
47.
Cerasi M, Ammendola S, Battistoni A. Competition for zinc binding in the host-pathogen interaction. Front Cell Infect Microbiol 2013; 3: 108.
48.
Leeming ER, Johnson AJ, Spector TD, Le Roy CI. Effect of diet on the gut microbiota: rethinking intervention duration. Nutrients 2019; 11: 2862.
49.
Tebani A, Bekri S. Paving the way to precision nutrition through metabolomics. Front Nutr 2019; 6: 41.
50.
Ontiveros N, Rodríguez-Bellegarrigue CI, Galicia-Rodríguez G, et al. Prevalence of self-reported gluten-related disorders and adherence to a gluten-free diet in Salvadoran adult population. Int J Environ Res Public Health 2018; 15: 786.
51.
Moszak M, Szulińska M, Bogdański P. You are what you eat-the relationship between diet, microbiota, and metabolic disorders – a review. Nutrients 2020; 12: 1096.
52.
Bonder MJ, Tigchelaar EF, Cai X et al. The influence of a short-term gluten-free diet on the human gut microbiome. Genome Med 2016; 8: 45.
53.
Garcia-Mazcorro JF, Noratto G, Remes-Troche JM. The Effect of gluten-free diet on health and the gut microbiota cannot be extrapolated from one population to others. Nutrients 2018; 10: 1421.
54.
Hansen LBS, Roager HM, Søndertoft NB, et al. A low-gluten diet induces changes in the intestinal microbiome of healthy Danish adults. Nat Commun 2018; 9: 4630.
55.
Caio G, Lungaro L, Segata N, et al. Effect of gluten-free diet on gut microbiota composition in patients with celiac disease and non-celiac gluten/wheat sensitivity. Nutrients 2020; 12: 1832.
56.
Nistal E, Caminero A, Vivas S, et al. Differences in faecal bacteria populations and faecal bacteria metabolism in healthy adults and celiac disease patients. Biochimie 2012; 94: 1724-9.
57.
Lebwohl B, Cao Y, Zong G, et al. Long term gluten consumption in adults without celiac disease and risk of coronary heart disease: prospective cohort study. BMJ 2017; 357: j1892.
58.
Pasolli E, Asnicar F, Manara S, et al. Extensive unexplored human microbiome diversity revealed by over 150,000 genomes from metagenomes spanning age, geography, and lifestyle. Cell 2019; 176: 649-62.e20.
59.
Lopez-Minguez J, Gómez-Abellán P, Garaulet M. Timing of breakfast, lunch, and dinner. Effects on obesity and metabolic risk. Nutrients 2019; 11: 2624.
60.
Orimoloye OA, Kambhampati S, Hicks AJ, et al. Higher cardiorespiratory fitness predicts long-term survival in patients with heart failure and preserved ejection fraction: The Henry Ford exercise Testing (FIT) project. Arch Med Sci 2019; 15: 350-8.
61.
Fiuza-Luces C, Santos-Lozano A, Joyner M, et al. Exercise benefits in cardiovascular disease: beyond attenuation of traditional risk factors. Nat Rev Cardiol 2018; 15: 731-43.
62.
Petriz BA, Castro AP, Almeida JA, et al. Exercise induction of gut microbiota modifications in obese, non-obese and hypertensive rats. BMC Genomics 2014; 15: 511.
63.
Lambert JE, Myslicki JP, Bomhof MR, Belke DD, Shearer J, Reimer RA. Exercise training modifies gut microbiota in normal and diabetic mice. Appl Physiol Nutr Metab 2015; 40: 749-52.
64.
Bressa C, Bailén-Andrino M, Pérez-Santiago J, et al. Differences in gut microbiota profile between women with active lifestyle and sedentary women. PLoS One 2017; 12: e0171352.
65.
Allen JM, Mailing LJ, Niemiro GM et al. Exercise Alters Gut Microbiota Composition and Function in Lean and Obese Humans. Med Sci Sports Exerc 2018; 50: 747-57.
66.
Nobili V, Putignani L, Mosca A et al. Bifidobacteria and lactobacilli in the gut microbiome of children with non-alcoholic fatty liver disease: which strains act as health players? Arch Med Sci 2018; 14: 81-7.
67.
Fong W, Li Q, Yu J. Gut microbiota modulation: a novel strategy for prevention and treatment of colorectal cancer. Oncogene 2020; 39: 4925-43.
68.
Markowiak P, Ślizewska K. Effects of probiotics, prebiotics, and synbiotics on human health. Nutrients 2017; 9: 1021.
69.
Costanza AC, Moscavitch SD, Faria Neto HCC, Mesquita ET. Probiotic therapy with Saccharomyces boulardii for heart failure patients: a randomized, double-blind, placebo-controlled pilot trial. Int J Cardiol 2015; 179: 348-50.
70.
Korcz E, Kerényi Z, Varga L. Dietary fibers, prebiotics, and exopolysaccharides produced by lactic acid bacteria: potential health benefits with special regard to cholesterol-lowering effects. Food Funct 2018; 9: 3057-68.
71.
Francino MP. Antibiotics and the human gut microbiome: dysbioses and accumulation of resistances. Front Microbiol 2016; 6: 1543.
72.
Bhalodi AA, van Engelen TSR, Virk HS, Wiersinga WJ. Impact of antimicrobial therapy on the gut microbiome. J Antimicrob Chemother 2019; 74 (Suppl. 1): i6-15.
73.
Ianiro G, Tilg H, Gasbarrini A. Antibiotics as deep modulators of gut microbiota: between good and evil. Gut 2016; 65: 1906-15.
74.
Cox LM, Blaser MJ. Antibiotics in early life and obesity. Nat Rev Endocrinol 2015; 11: 182-90.
75.
Cho I, Yamanishi S, Cox L, et al. Antibiotics in early life alter the murine colonic microbiome and adiposity. Nature 2012; 488: 621-6.
76.
Murphy EF, Cotter PD, Hogan A, et al. Divergent metabolic outcomes arising from targeted manipulation of the gut microbiota in diet-induced obesity. Gut 2013; 62: 220-6.
77.
Hwang I, Park YJ, Kim Y-R, et al. Alteration of gut microbiota by vancomycin and bacitracin improves insulin resistance via glucagon-like peptide 1 in diet-induced obesity. FASEB J 2015; 29: 2397-411.
78.
Dao MC, Everard A, Aron-Wisnewsky J, et al. Akkermansia muciniphila and improved metabolic health during a dietary intervention in obesity: Relationship with gut microbiome richness and ecology. Gut 2016; 65: 426-36.
79.
Bailey LC, Forrest CB, Zhang P, Richards TM, Livshits A, DeRusso PA. Association of antibiotics in infancy with early childhood obesity. JAMA Pediatr 2014; 168: 1063-9.
80.
Isanaka S, Langendorf C, Berthé F, et al. Routine amoxicillin for uncomplicated severe acute malnutrition in children. N Engl J Med 2016; 374: 444-53.
81.
Eiseman B, Silen W, Bascom GS, Kauvar AJ. Fecal enema as an adjunct in the treatment of pseudomembranous enterocolitis. Surgery 1958; 44: 854-9.
82.
Vrieze A, Out C, Fuentes S, et al. Impact of oral vancomycin on gut microbiota, bile acid metabolism, and insulin sensitivity. J Hepatol 2014; 60: 824-31.
83.
Chen K, Zheng X, Feng M, Li D, Zhang H. Gut microbiota-dependent metabolite trimethylamine n-oxide contributes to cardiac dysfunction in western diet-induced obese mice. Front Physiol 2017; 8: 139.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.