Introduction
Prevalence of constipation in the worldwide general population is very variable. It is estimated that between 0.7% and 29.6% of children suffer from constipation [1]. Functional constipation is constipation with no specific anatomical, medical or pharmaceutical causes, and is more common in children [2]. Functional constipation in children is multifactorial and two factors – inadequate dietary fiber intake and delayed bowel movements – often lead to progression of constipation [3]. Much effort has been made to standardize the terminology of children’s constipation and several international guidelines have been accepted for its definition, including NASPGHAN [4], PACCT [5], and ROME III [6], but none of them have been widely used in clinical practice or research work. Attention deficit hyperactivity disorder (ADHD) is one of the common behavioral problems in children [7, 8]. ADHD is defined as a sustained pattern of low attention or low attention with hyperactivity and impulsive behavior that is more than expected due to the age and level of development of the child [9]. The reported incidence of this disorder in school age children is between 3% and 8% [7, 10, 11]. It is more common in males than females (3 in 1 to 5 in 1) and the symptoms of the disease usually present by 3 years old [7]. Children with ADHD are at increased risk of other problems such as antisocial behavior, anxiety disorders, mood disorders, learning disorders, drug abuse and communication problems [12–14].
Experts have experimentally found that in children’s constipation, the importance of managing constipation-related behaviors is not less than that of a dietary or therapy regime [15].
Considering the higher prevalence of constipation and fecal incontinence among children with ADHD and the hypotheses explaining this relationship including behavioral problems, neurobiological disorders, defects in the relationship between the nervous system of the digestive system and the central nervous system, and the delay in maturation of the gastrointestinal tract [16], the aim of this study was to determine the frequency of ADHD in children with functional constipation and the effect of ADHD treatment on their constipation.
Material and methods
In this study, 2,090 children aged 4 to 12 years with constipation referred to the pediatric gastroenterology clinic of Besat Hospital in Hamadan City, Iran, during the years 2016 and 2017, after confirmation of the diagnosis of functional constipation by a pediatric gastroenterologist (based on the criteria of 2006 ROME III [6]), were evaluated to determine simultaneous existence of ADHD using the Conners Questionnaire. If the patient had a total score of 34 points, he/she was referred to a psychiatrist, and if ADHD was approved by a psychiatrist, he was entered into the study.
Patients with organic causes of constipation including Hirschsprung’s disease, hypothyroidism, spina bifida occulta, anorectal abnormalities, non-retentive fecal incontinency, chronic intestinal pseudo-obstruction, history of anorectal/colon surgery, and taking medications which could modify bowel habit, were excluded from the study.
This study was conducted with the approval of the Ethics Committee of Hamadan University of Medical Sciences (with the ethics code, Deputy of Research and Technology IR.UMSHA.REC.1395.535). All parents gave written informed consent and the parents took the oral assent of the children.
Eighty patients out of 290 patients with simultaneous ADHD and functional constipation were selected by simple randomization and then randomly divided by random blocks into two equal groups.
Non-treated group: They were only treated for ADHD by a standard method [17].
Treated group: At the same time, they were treated for ADHD and functional constipation including a dietary regimen and PEG without electrolyte at a maximum dose (0.7 g/kg/day, 13.8–40.0 g/daily), twice a day. For children with rectal impaction, disimpaction was initially performed with bisacodyl suppositories for 3–5 days (5 mg/daily > 4 years). No further treatment was allowed for constipation during the study.
Patients’ data were collected by a questionnaire including name, sex, age, duration of constipation, consistency/size/frequency of stool, number of painful defecations, fecal incontinence per week, and stool mass in the abdomen or rectum.
Parents were given dose regulation training to record the number and consistency of stools, frequency of stomach incontinence, abdominal pain, and pain relief.
Patients were examined and re-visited at 1, 3, 6 and 12 months after starting treatment, and drug dosage was adjusted.
To evaluate the response to treatment of ADHD, the Conners Questionnaire was used again, which would have been considered as improvement if the patient’s score was less than 34.
The definition of response to constipation treatment was ≥ 3 bowel movements weekly, ≤ 2 episodes of fecal incontinence per month and absence of abdominal pain.
Statistical analysis
In this study, quantitative variables were presented as mean and standard deviation, and qualitative variables were reported as percentages. The χ2 test was used to evaluate the association between functional constipation improvement and sex/type of treatment. The Kolmogorov-Smirnov one sample test was used for normality detection. To compare disease duration between improved and non-improved patients, the Mann-Whitney U test was used, because distribution of disease duration was not normal. Data were analyzed using SPSS16 software. P-value < 0.05 was considered statistically significant.
Results
Eighty children with simultaneous ADHD and functional constipation were enrolled. Forty were in the non-treated group and forty in the treated group.
The percentage of male and female subjects in the non-treated group and treated group was respectively 55%, 45%, 57.5% and 42.5% (p = 0.822), with mean age 8.02 ±1.9 and 8.07 ±2.3 years (p = 0.458).
There were no significant differences regarding demographic data and duration of ADHD and constipation between the two groups (Table I).
Table I
Comparison of demographic and clinical characteristic between treated and non-treated groups
| Variable | Non-treated groupa | Treated groupb | P-value |
|---|---|---|---|
| Male sex, n (%) | 22 (55.0) | 23 (57.5) | 0.822* |
| Age [years], mean (SD) | 8.02 (1.9) | 8.07 (2.3) | 0.458** |
| Duration of having constipation [months], mean (SD) | 11.52 (2.89) | 11.37 (2.78) | 0.594** |
| Duration of having ADHD [months], mean (SD) | 13.47 (4.78) | 13.14 (4.46) | 0.624** |
The frequency of constipation recovery in the non-treated group was 5% (2) while it was 97.5% (39) in the treated group; the difference was statistically significant (p < 0.001).
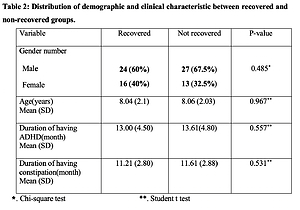
There was no statistically significant relationship between functional constipation recovery in children with ADHD and age, sex, and duration of having functional constipation and ADHD (Table II).
Table II
Comparison of demographic and clinical characteristics between recovered and non-recovered groups
| Variable | Recovered | Not recovered | P-value |
|---|---|---|---|
| Gender, n (%): | |||
| Male | 24 (60.0) | 27 (67.5) | 0.485* |
| Female | 16 (40.0) | 13 (32.5) | |
| Age [years], mean (SD) | 8.04 (2.1) | 8.06 (2.03) | 0.967** |
| Duration of having ADHD [months], mean (SD) | 13.00 (4.50) | 13.61 (4.80) | **0.557** |
| Duration of having constipation [months], mean (SD) | 11.21 (2.80) | 11.61 (2.88) | **0.531 |
The frequency of ADHD recovery in the non-treated group and treated group was 100%.
Discussion
In the present study, 13.87% of children with functional constipation had ADHD. The recovery of functional constipation in patients with ADHD who were simultaneously treated for constipation was higher than in patients who only received ADHD treatment. This means that treatment of ADHD has no effect on the treatment of constipation. There was no significant correlation between the recovery of functional constipation in children treated for ADHD and constipation with duration of having ADHD and functional constipation and patient’ age and sex.
Also the treatment of constipation did not significantly affect the frequency of ADHD recovery.
In a study by McKeown et al. in the United States between 2005 and 2007 in children aged 4 to 12 years old, the prevalence of ADHD was 4.4%, and the incidence of functional constipation in children with ADHD was 4.1%, while in children without ADHD it was 1.5%. Based on the findings of this study, although the risk of ADHD may increase the risk of functional constipation, ADHD treatment has no significant effect on the increase or decrease of constipation [18].
In the present study, similar to McKeown et al.’ findings, treatment of ADHD did not influence the functional constipation recovery.
In a study by Duel et al. in the United States whose results were published in 2003, in 28 patients with ADHD in comparison with 22 healthy persons with voiding dysfunction, measured by the Dysfunctional Voiding Symptom Survey (DVSS) questionnaire, the mean total score of the DVSS questionnaire in male subjects with ADHD and the control group was respectively 14.83 ±3.68 and 6.6 ±5.74, and in female subjects with ADHD and the control group it was respectively 19.0 ±5.3 and 5.83. The results of this study showed that in patients with ADHD, the mean score of the DVSS questionnaire (symptoms of fecal dysfunction) was significantly higher than in the control group in both males and females [19].
According to the results of the Benninga et al. study on children aged 5 to 17 years, due to problems with defecation of stool and abdominal and behavioral problems, it seems there is no relationship between colonic/anorectal function and behavioral profiles. However, children with gastrointestinal disorders had more behavioral problems than the control group [20].
The results of research by Becker et al. on the neural process of excitement and fecal incontinence in 14 children with fecal incontinence and constipation showed that in children with fecal incontinence, the response process to emotions and excitement was increased and could be considered as neurocognitive vulnerability due to the relation of the enteric nervous system with the central nervous system [16].
In a study by Niemczyk et al. in children aged 7 to 17 years with ADHD, delayed bowel control was significantly more prevalent than in children in the control group but treatment of ADHD, especially medication, can improve the treatment outcome of incontinence [21], which is different from the findings of the present study.
In our study, the treatment of constipation did not significantly affect the frequency of ADHD recovery. Unfortunately, no similar study was found for comparison.
Although functional constipation may be more prevalent in children with ADHD [18], or children with gastrointestinal disorders may have more behavioral disorders and neurobiological disorders, including deficiencies in the nervous and central nervous system, and delayed maturation of gastrointestinal motility may have a relation with functional constipation [16], according to our research, the treatment of ADHD or constipation has no significant effect on the recovery of the other condition. On the contrary, each disorder requires separate treatment.
In conclusion, in patients with functional constipation, ADHD is a common association and treatment of ADHD is not effective in the recovery of functional constipation. Also, treatment of constipation has no effect on the recovery of ADHD.