Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
HEPATOLOGY / CLINICAL RESEARCH
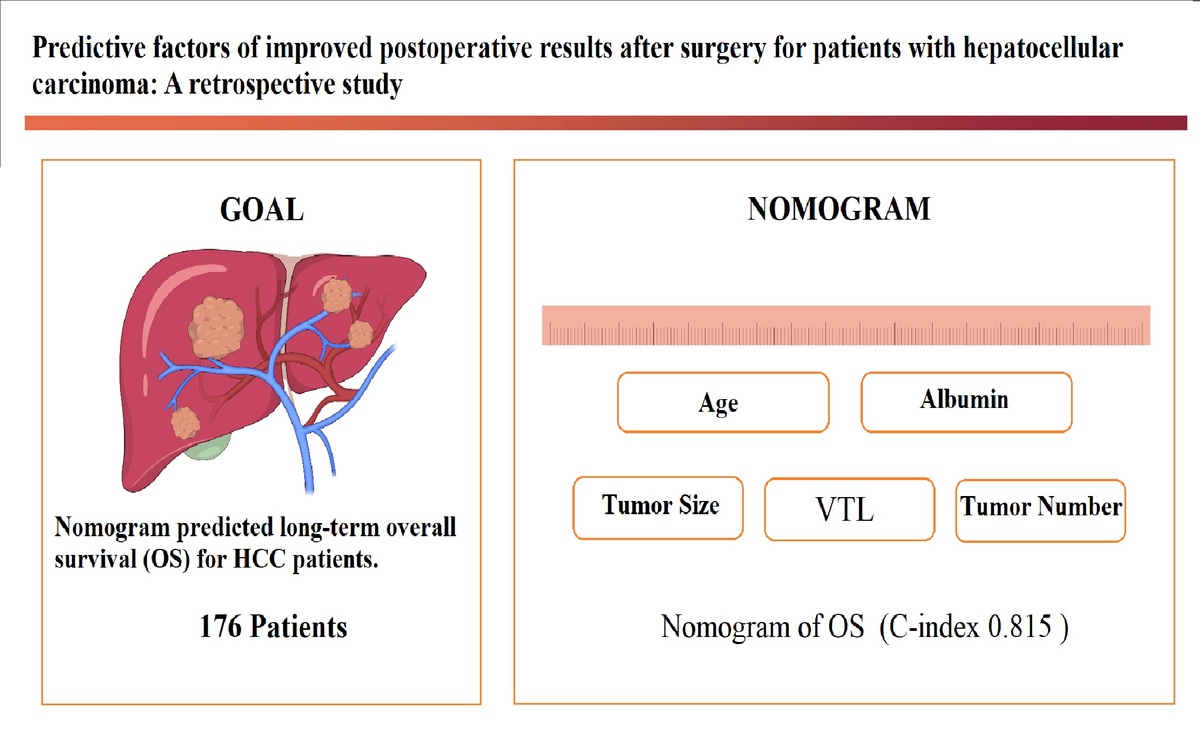
Predictive factors of improved postoperative results after surgery for patients with hepatocellular carcinoma: a retrospective study
1
Department of Surgery, Zhejiang University School of Medicine, Sir Run Run Shaw Hospital, China
Submission date: 2024-11-27
Final revision date: 2025-05-20
Acceptance date: 2025-05-26
Online publication date: 2025-06-25
Corresponding author
Xiu-Jun Cai
Department of General Surgery Zhejiang University School of Medicine Sir Run Run Shaw Hospital No. 3 East Qing-chun Road Hangzhou 310016 Zhejiang Province, China
Department of General Surgery Zhejiang University School of Medicine Sir Run Run Shaw Hospital No. 3 East Qing-chun Road Hangzhou 310016 Zhejiang Province, China
KEYWORDS
TOPICS
ABSTRACT
Introduction:
Several clinical studies have demonstrated the benefits of surgery for patients with hepatocellular carcinoma (HCC). The goal of our study was to identify prognostic factors associated with overall survival (OS) and recurrence-free survival (RFS) in patients with HCC and develop nomograms to predict these factors.
Material and methods:
We retrospectively conducted follow-up evaluations of 176 patients with HCC up to 10 years after their tumors were removed. All of these patients were from a single hospital, and all of the enrolled patients were divided into two groups: those who survived less than 3 years and those who survived more than 3 years. Independent prognostic factors associated with OS and RFS were determined via univariate and multivariate Cox regression model analyses. Two prognostic nomogram models were built on the basis of the data and evaluated via the concordance index (C-index). The calibration curves indicated that the two nomograms performed well over a 5-year period. Additionally, the area under the receiver operating characteristic (ROC) curve and the time-dependent area under the ROC curve (AUC) were determined, and decision curve analyses (DCAs) were conducted.
Results:
The nomograms successfully discriminated patients with HCC. Prognostic factors for OS and RFS were identified, and nomograms were successfully built. The calibration discrimination was good for both the OS and RFS nomogram prediction models (C-indexes: 0.815 and 0.80, respectively). Our nomograms and calibration curves demonstrated favorable results with strong predictive accuracy and ROC curves, and according to the DCA, our nomogram results showed a greater net clinical benefit. The Kaplan-Meier plots for OS and RFS were generated via the log-rank test, the p-value of which was < 0.001. Ultimately, the nomograms successfully discriminated patients with HCC.
Conclusions:
We established nomogram survival prediction models to predict the prognosis of HCC after invasive treatment and achieved an acceptable level of accuracy in both OS and RFS analyses. These models may be valuable for guiding the selection of clinical treatment strategies and may also facilitate clinical decision making.
Several clinical studies have demonstrated the benefits of surgery for patients with hepatocellular carcinoma (HCC). The goal of our study was to identify prognostic factors associated with overall survival (OS) and recurrence-free survival (RFS) in patients with HCC and develop nomograms to predict these factors.
Material and methods:
We retrospectively conducted follow-up evaluations of 176 patients with HCC up to 10 years after their tumors were removed. All of these patients were from a single hospital, and all of the enrolled patients were divided into two groups: those who survived less than 3 years and those who survived more than 3 years. Independent prognostic factors associated with OS and RFS were determined via univariate and multivariate Cox regression model analyses. Two prognostic nomogram models were built on the basis of the data and evaluated via the concordance index (C-index). The calibration curves indicated that the two nomograms performed well over a 5-year period. Additionally, the area under the receiver operating characteristic (ROC) curve and the time-dependent area under the ROC curve (AUC) were determined, and decision curve analyses (DCAs) were conducted.
Results:
The nomograms successfully discriminated patients with HCC. Prognostic factors for OS and RFS were identified, and nomograms were successfully built. The calibration discrimination was good for both the OS and RFS nomogram prediction models (C-indexes: 0.815 and 0.80, respectively). Our nomograms and calibration curves demonstrated favorable results with strong predictive accuracy and ROC curves, and according to the DCA, our nomogram results showed a greater net clinical benefit. The Kaplan-Meier plots for OS and RFS were generated via the log-rank test, the p-value of which was < 0.001. Ultimately, the nomograms successfully discriminated patients with HCC.
Conclusions:
We established nomogram survival prediction models to predict the prognosis of HCC after invasive treatment and achieved an acceptable level of accuracy in both OS and RFS analyses. These models may be valuable for guiding the selection of clinical treatment strategies and may also facilitate clinical decision making.
REFERENCES (31)
2.
Forner A, Llovet JM, Bruix J. Hepatocellular carcinoma. Lancet 2012; 379: 1245-55.
4.
Liao K, Yang K, Cao L, et al. Laparoscopic anatomical versus non-anatomical hepatectomy in the treatment of hepatocellular carcinoma: a randomised controlled trial. Int J Surg 2022; 102: 106652.
5.
Chapman WC, Klintmalm G, Hemming A, et al. Surgical treatment of hepatocellular carcinoma in North America: can hepatic resection still be justified? J Am Coll Surg 2015; 220: 628-37.
6.
Moazzam Z, Lima HA, Alaimo L, et al. Impact of tumor burden score on timing and patterns of recurrence after curative-intent resection of hepatocellular carcinoma. Surgery 2022; 172: 1448-55.
7.
Shim JH, Jun MJ, Han S, et al. Prognostic nomograms for prediction of recurrence and survival after curative liver resection for hepatocellular carcinoma. Ann Surg 2015; 261: 939-46.
8.
Vogel A, Cervantes A, Chau I, et al. Correction to: “Hepatocellular carcinoma: ESMO clinical practice guidelines for diagnosis, treatment and follow-up”. Ann Oncol 2019; 30: 871-3.
9.
Gandhi S, Khubchandani S, Iyer R. Quality of life and hepatocellular carcinoma. J Gastrointest Oncol 2014; 5: 296-317.
10.
Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2021; 71: 209-49.
11.
Amin MB, Greene FL, Edge SB, et al. The eighth edition AJCC cancer staging manual: continuing to build a bridge from a population-based to a more “personalized” approach to cancer staging. CA Cancer J Clin 2017; 67: 93-9.
12.
Reig M, Forner A, Rimola J, et al. BCLC strategy for prognosis prediction and treatment recommendation: the 2022 update. J Hepatol 2022; 76: 681-93.
13.
Kudo M, Chung H, Osaki Y. Prognostic staging system for hepatocellular carcinoma (CLIP score): Its value and limitations, and a proposal for a new staging system, the Japan Integrated Staging Score (JIS score). J Gastroenterol 2003; 38: 207-15.
14.
Xu XF, Xing H, Han J, et al. Risk factors, patterns, and outcomes of late recurrence after liver resection for hepatocellular carcinoma: a multicenter study from China. JAMA Surg 2019; 154: 209-17.
15.
Tranchart H, Chirica M, Sepulveda A, et al. Long-term outcomes following aggressive management of recurrent hepatocellular carcinoma after upfront liver resection. World J Surg 2012; 36: 2684-91.
16.
Li Y, Xia Y, Li J, et al. Prognostic nomograms for pre- and postoperative predictions of long-term survival for patients who underwent liver resection for huge hepatocellular carcinoma. J Am Coll Surg 2015; 221: 962-74.
17.
Zhang XP, Chen ZH, Zhou TF, et al. A nomogram to predict early postoperative recurrence of hepatocellular carcinoma with portal vein tumour thrombus after R0 liver resection: a large-scale, multicenter study. Eur J Surg Oncol 2019; 45: 1644-51.
18.
Takuma Y, Shota I, Miyatake H, et al. Nomograms to predict the disease-free survival and overall survival after radiofrequency ablation for hepatocellular carcinoma. Intern Med 2018; 57: 457-68.
19.
Cho CS, Gonen M, Shia J, et al. A novel prognostic nomogram is more accurate than conventional staging systems for predicting survival after resection of hepatocellular carcinoma. J Am Coll Surg 2008; 206: 281-91.
20.
Troisi RI, Berardi G, Morise Z, et al. Laparoscopic and open liver resection for hepatocellular carcinoma with Child-Pugh B cirrhosis: multicentre propensity score-matched study. Br J Surg 2021; 108: 196-204.
21.
Nguyen-Khac V, Brustia R, Rhaiem R, et al. Liver resection for single large hepatocellular carcinoma: a prognostic factors study. Ann Hepatol 2022; 27: 100739.
22.
Rodríguez-Perálvarez M, Luong TV, Andreana L, Meyer T, Dhillon AP, Burroughs AK. A systematic review of microvascular invasion in hepatocellular carcinoma: diagnostic and prognostic variability. Ann Surg Oncol 2012; 20: 325-39.
23.
Endo Y, Lima HA, Alaimo L, et al. Preoperative risk score (PreopScore) to predict overall survival after resection for hepatocellular carcinoma. HPB 2023; 25: 353-62.
24.
Lei Z, Li J, Wu D, et al. Nomogram for preoperative estimation of microvascular invasion risk in hepatitis B virus–related hepatocellular carcinoma within the Milan criteria. JAMA Surg 2016; 151: 356-63.
25.
Xiao YB, Zhang B, Wu Y.L. Radiofrequency ablation versus hepatic resection for breast cancer liver metastasis: a systematic review and meta-analysis. J Zhejiang Univ Sci B 2018; 19: 829-43.
26.
Chan AWH, Zhong J, Berhane S, et al. Development of pre and post-operative models to predict early recurrence of hepatocellular carcinoma after surgical resection. J Hepatol 2018; 69: 1284-93.
27.
Zhang LX, Luo PQ, Chen L, et al. Model to predict overall survival in patients with hepatocellular carcinoma after curative hepatectomy. Front Oncol 2020; 10: 537526.
28.
Chen WT, Chau GY, Lui WY, et al. Recurrent hepatocellular carcinoma after hepatic resection: prognostic factors and long-term outcome. Eur J Surg Oncol 2004; 30: 414-20.
29.
Choe WH. Is multidisciplinary treatment effective for hepatocellular carcinoma with portal vein tumor thrombus? J Liver Cancer 2022; 22: 1-3.
30.
Zhang F, Lu CD, Zhang XP, et al. The impact of portal vein tumor thrombus on long-term survival after liver resection for primary hepatic malignancy. HPB 2020; 22: 1025-33.
31.
Mähringer-Kunz A, Steinle V, Düber C, et al. Extent of portal vein tumour thrombosis in patients with hepatocellular carcinoma: the more, the worse? Liver Int 2019; 39: 324-31.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.