Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
CLINICAL RESEARCH
The impact of magnesium sulfate administration on
the prognosis of septic patients with hypomagnesemia:
a retrospective propensity score-matched cohort study
based on MIMIC-IV
1
The Xuzhou Clinical College of Xuzhou Medical University, Jiangsu Xuzhou, China
2
Department of Critical Care Medicine, Xuzhou Central Hospital, Jiangsu Xuzhou, China
3
Department of Critical Care Medicine, Sishui County People’s Hospital, Shandong Jining, China
Submission date: 2024-12-01
Final revision date: 2025-03-03
Acceptance date: 2025-03-29
Online publication date: 2025-05-05
Corresponding author
Jiaqiong Li
The Xuzhou Clinical College Xuzhou Medical University Department of Critical Care Medicine Xuzhou Central Hospital Jiangsu Xuzhou 221009 China
The Xuzhou Clinical College Xuzhou Medical University Department of Critical Care Medicine Xuzhou Central Hospital Jiangsu Xuzhou 221009 China
KEYWORDS
TOPICS
ABSTRACT
Introduction:
This study aimed to provide a basis for optimizing clinical treatment by retrospectively analyzing the clinical characteristics of hypomagnesemia in sepsis patients and the impact of magnesium sulfate administration on their prognosis.
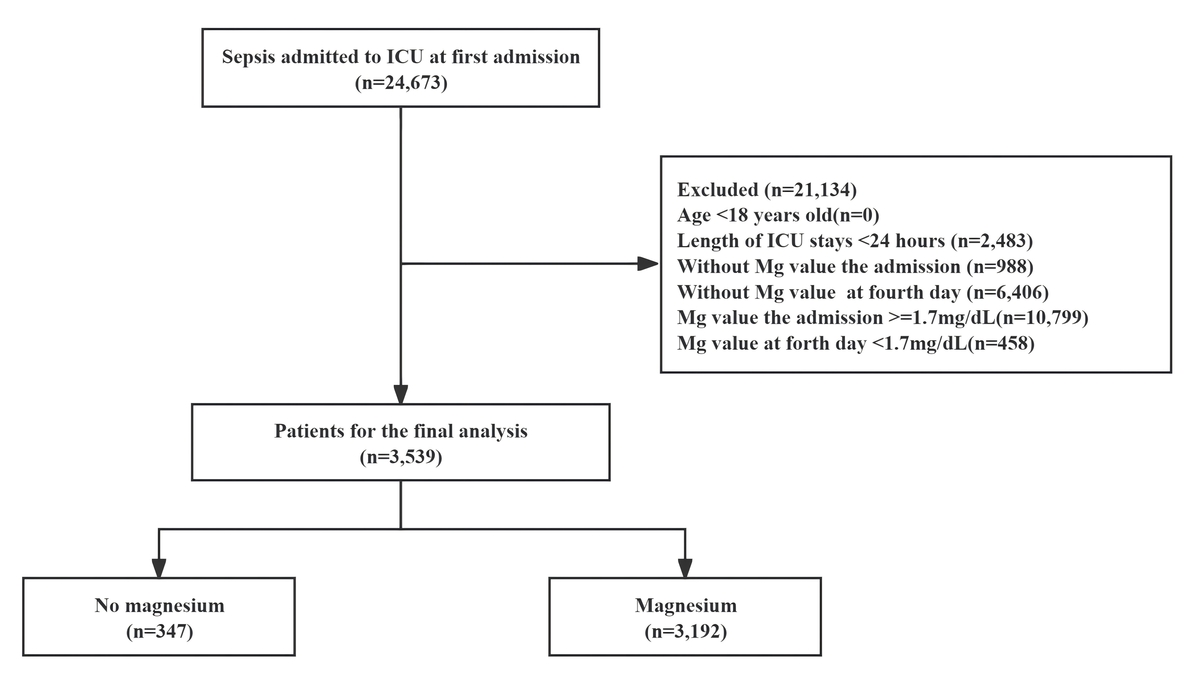
Material and methods:
Based on inclusion and exclusion criteria, we included adult individuals diagnosed with sepsis and concurrent hypomagnesemia. Exposure was defined as administration of magnesium sulfate on the first day of ICU admission. The primary outcome assessed was the 28-day mortality rate. Secondary outcomes encompassed mortality rates at 90 and 365 days, the duration of mechanical ventilation, requirement for continuous renal replacement therapy (CRRT), hospital stay duration, intensive care unit (ICU) stay duration, hospital mortality, and ICU mortality. A multivariable Cox regression analysis was conducted to evaluate the relationship between sepsis with hypomagnesemia and 28-day mortality. Propensity score matching (PSM) was performed at a 1 : 1 ratio. Multivariable analysis was used to adjust for confounding factors.
Results:
In the PSM analysis, the 28-day mortality rate appeared reduced in the magnesium sulfate treatment group relative to the untreated group (10.15% [33/3192] vs. 16.31% [53/347]). Magnesium sulfate use correlated with a decreased 28-day mortality rate (hazard ratio [HR] = 0.61; 95% CI: 0.39–0.94; p = 0.026). Magnesium sulfate administration also reduced the 90-day mortality rate (p = 0.039). Statistical analysis revealed no significant differences between magnesium sulfate administration and the use of CRRT, mechanical ventilation duration, hospital and ICU lengths of stay, or mortality rates at 365 days.
Conclusions:
The administration of magnesium sulfate is associated with a reduced mortality rate in individuals diagnosed with sepsis and hypomagnesemia, providing theoretical support for clinical practice.
This study aimed to provide a basis for optimizing clinical treatment by retrospectively analyzing the clinical characteristics of hypomagnesemia in sepsis patients and the impact of magnesium sulfate administration on their prognosis.
Material and methods:
Based on inclusion and exclusion criteria, we included adult individuals diagnosed with sepsis and concurrent hypomagnesemia. Exposure was defined as administration of magnesium sulfate on the first day of ICU admission. The primary outcome assessed was the 28-day mortality rate. Secondary outcomes encompassed mortality rates at 90 and 365 days, the duration of mechanical ventilation, requirement for continuous renal replacement therapy (CRRT), hospital stay duration, intensive care unit (ICU) stay duration, hospital mortality, and ICU mortality. A multivariable Cox regression analysis was conducted to evaluate the relationship between sepsis with hypomagnesemia and 28-day mortality. Propensity score matching (PSM) was performed at a 1 : 1 ratio. Multivariable analysis was used to adjust for confounding factors.
Results:
In the PSM analysis, the 28-day mortality rate appeared reduced in the magnesium sulfate treatment group relative to the untreated group (10.15% [33/3192] vs. 16.31% [53/347]). Magnesium sulfate use correlated with a decreased 28-day mortality rate (hazard ratio [HR] = 0.61; 95% CI: 0.39–0.94; p = 0.026). Magnesium sulfate administration also reduced the 90-day mortality rate (p = 0.039). Statistical analysis revealed no significant differences between magnesium sulfate administration and the use of CRRT, mechanical ventilation duration, hospital and ICU lengths of stay, or mortality rates at 365 days.
Conclusions:
The administration of magnesium sulfate is associated with a reduced mortality rate in individuals diagnosed with sepsis and hypomagnesemia, providing theoretical support for clinical practice.
REFERENCES (32)
1.
Singer M, Deutschman CS, Seymour CW, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016; 315: 801-10.
2.
Hu X, Qin X, Gu X, Wang H, Zhou W. Effect of lymphocyte-to-monocyte ratio on survival in septic patients: an observational cohort study. Arch Med Sci 2020; 20: 790-7.
3.
Cecconi M, Evans L, Levy M, Rhodes A. Sepsis and septic shock. Lancet 2018; 392: 75-87.
4.
Tiru B, DiNino EK, Orenstein A, et al. The economic and humanistic burden of severe sepsis. Pharmacoeconomics 2015; 33: 925-37.
5.
Martín-Rodríguez F, López-Izquierdo R, Castro Villamor M, et al. Head-to-head comparison of pre-hospital qSOFA and lactate-qSOFA for predicting sepsis in patients with and without suspected infection. A multicenter prospective cohort study. Arch Med Sci 2020; 20: 1547-55.
6.
Rudd KE, Johnson SC, Agesa KM, et al. Global, regional, and national sepsis incidence and mortality, 1990-2017: analysis for the Global Burden of Disease Study. Lancet 2020; 395: 200-11.
7.
Lee JW. Fluid and electrolyte disturbances in critically ill patients. Electrolyte Blood Press 2010; 8: 72-81.
8.
Touyz RM, de Baaij JHF, Hoenderop JGJ. Magnesium disorders. N Engl J Med 2024; 390: 1998-2009.
9.
Gries A, Bode C, Gross S, Peter K, Bohrer H, Martin E. The effect of intravenously administered magnesium on platelet function in patients after cardiac surgery. Anesth Analg 1999; 88: 1213-9.
10.
Hansen BA, Bruserud O. Hypomagnesemia in critically ill patients. J Intensive Care 2018; 6: 21.
11.
Magnesium supplementation in the treatment of diabetes. American Diabetes Association. Diabetes Care 1992; 15: 1065-7.
12.
Quamme GA, de Rouffignac C. Epithelial magnesium transport and regulation by the kidney. Front Biosci 2000; 5: D694-711.
13.
Martin BJ, Milligan K. Diuretic-associated hypomagnesemia in the elderly. Arch Intern Med 1987; 147: 1768-71.
14.
Volpe SL. Magnesium in disease prevention and overall health. Adv Nutr 2013; 4: 378S-83S.
15.
Del Gobbo LC, Imamura F, Wu JH, de Oliveira Otto MC, Chiuve SE, Mozaffarian D. Circulating and dietary magnesium and risk of cardiovascular disease: a systematic review and meta-analysis of prospective studies. Am J Clin Nutr 2013; 98: 160-73.
16.
Jiang P, Lv Q, Lai T, Xu F. Does hypomagnesemia impact on the outcome of patients admitted to the intensive care unit? A systematic review and meta-analysis. Shock 2017; 47: 288-95.
17.
Khalili H, Rahmani H, Mohammadi M, Salehi M, Mostafavi Z. Intravenous magnesium sulfate for prevention of vancomycin plus piperacillin-tazobactam induced acute kidney injury in critically ill patients: an open-label, placebo-controlled, randomized clinical trial. Daru 2021; 29: 341-51.
18.
Velissaris D, Karamouzos V, Pierrakos C, Aretha D, Karanikolas M. Hypomagnesemia in critically ill sepsis patients. J Clin Med Res 2015; 7: 911-8.
19.
Gu WJ, Duan XJ, Liu XZ, et al. Association of magnesium sulfate use with mortality in critically ill patients with sepsis: a retrospective propensity score-matched cohort study. Br J Anaesth 2023; 131: 861-70.
20.
Noormandi A, Khalili H, Mohammadi M, Abdollahi A. Effect of magnesium supplementation on lactate clearance in critically ill patients with severe sepsis: a randomized clinical trial. Eur J Clin Pharmacol 2020; 76: 175-84.
21.
Barbosa EB, Tomasi CD, de Castro Damasio D, et al. Effects of magnesium supplementation on the incidence of acute kidney injury in critically ill patients presenting with hypomagnesemia. Intensive Care Med 2016; 42: 1084-5.
22.
Li L, Li L, Zhao Q, et al. High serum magnesium level is associated with increased mortality in patients with sepsis: an international, multicenter retrospective study. MedComm (2020) 2024; 5: e713.
23.
Alswat K. Type 2 diabetes control and complications and it relation to the serum magnesium level. Arch Med Sci 2021; 18: 307-13.
24.
Aryana P, Rajaei S, Bagheri A, Karimi F, Dabbagh A. Acute effect of intravenous administration of magnesium sulfate on serum levels of interleukin-6 and tumor necrosis factor-alpha in patients undergoing elective coronary bypass graft with cardiopulmonary bypass. Anesth Pain Med 2014; 4: e16316.
25.
de Baaij JH, Hoenderop JG, Bindels RJ. Magnesium in man: implications for health and disease. Physiol Rev 2015; 95: 1-46.
26.
Lin CY, Tsai PS, Hung YC, Huang CJ. L-type calcium channels are involved in mediating the anti-inflammatory effects of magnesium sulphate. Br J Anaesth 2010; 104: 44-51.
27.
Lee CY, Jan WC, Tsai PS, Huang CJ. Magnesium sulfate mitigates acute lung injury in endotoxemia rats. J Trauma 2011; 70: 1177-85; discussion 85.
28.
Ahmed LA. Protective effects of magnesium supplementation on metabolic energy derangements in lipopolysaccharide-induced cardiotoxicity in mice. Eur J Pharmacol 2012; 694: 75-81.
29.
Zhou X, Li X, Yi K, et al. Magnesium isoglycyrrhizinate ameliorates lipopolysaccharide-induced liver injury by upregulating autophagy and inhibiting inflammation via IL-22 expression. Bioorg Chem 2022; 128: 106034.
30.
Bai YX, Wang ZH, Lv Y, et al. Association between frailty and acute kidney injury after cardiac surgery: unraveling the moderation effect of body fat through an international, retrospective, multi-cohort study. Int J Surg 2025; 111: 761-70.
31.
Zhong T, Zhang J, Chen S, et al. Magnesium sulfate ameliorates histone-induced coagulation dysfunction and lung damage in mice. Shock 2024; 61: 132-41.
32.
Vankrunkelsven W, Gunst J, Amrein K, et al. Monitoring and parenteral administration of micronutrients, phosphate and magnesium in critically ill patients: the VITA-TRACE survey. Clin Nutr 2021; 40: 590-9.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.