Introduction
Non-alcoholic fatty liver disease (NAFLD) is characterized by excessive accumulation of lipids in the liver defining the presence of steatosis in > 5% hepatocytes according to the histological findings, i.e. > 5.6% fat content measured by proton magnetic resonance spectroscopy (1H-MRS) [1]. To establish the diagnosis of NAFLD, it is necessary to exclude other possible causes of liver fat deposition, such as alcohol consumption (> 20 g daily, or > 14 drinks per week in female subjects; 30 g daily, or > 21 drinks per week in male subjects), other chronic liver diseases (viral, autoimmune, infiltrative), and the use of different medications that favour liver steatosis (amiodarone, corticosteroids, cytotoxic agents, members of highly-active antiretroviral therapy, tamoxifen, and numerous other drugs) [1–4]. Fatty liver is presented as NAFLD and/or non-alcoholic steatohepatitis (NASH) as 2 separate entities. In contrast to NAFLD, NASH may further progress to fibrosis, cirrhosis, and hepatocellular carcinoma (HCC) [1]. Thus, the fatty liver may manifest a diverse histological spectrum ranging from simple steatosis to inflammation and fibrosis, which may cause life-threatening liver and systemic complications [5, 6].
Metabolic syndrome (MetS) represents a group of interrelated risk factors that favour the emergence and development of atherosclerotic cardiovascular disease (CVD) and type 2 diabetes mellitus (T2DM) [7, 8]. These factors include perturbation in glucose metabolism (impaired fasting glycaemia (IFG), impaired glucose tolerance (IGT), or T2DM), arterial hypertension, dyslipidaemia (hypertriglyceridaemia and/or decreased level of high-density lipoproteins (HDL)), and central type obesity [9, 10]. The prevalence of MetS is 10–84%, depending on geographic region, rural/urban surroundings, demographic characteristics of a population, and criteria for diagnosis of MetS [11]. Age and sex also influence the prevalence of MetS – an increase in prevalence with age and in the female sex [12, 13]. MetS has become one of the leading public health problems due to the continuous increase in the number of obese individuals [14]. The significance of MetS is more evident through higher morbidity and mortality rates of progressive atherosclerosis diseases accelerated by pro-inflammatory and pro-coagulant components of MetS compared to individuals without MetS [15–17]. Additionally, the presence of NAFLD in lean subjects becomes a diagnostic and treatment challenge and emphasizes the significance of visceral over central obesity [18].
The pathophysiological mechanism that may connect most of the above-described conditions is insulin resistance (IR) [9]. IR is a state in which the normal concentration of insulin is not sufficient to provide the expected response of peripheral tissues, such as the liver, fat, and muscle tissues, as the most important target organs for the action of insulin. Consequently, increased secretion of insulin occurs to overcome the state of hyperglycaemia. Hyperinsulinaemia is a transitory state, and if the stimulus for insulin secretion persists, pancreatic β cells cannot secrete the amount of insulin sufficient for overcoming hyperglycaemia, leading to IGT or T2DM [9, 19]. MetS and NAFLD/NASH are associated with an increased risk of CVD and T2DM [20, 21].
The presented metabolic triad are among the most frequent noncommunicable diseases met today. The health and economic burden of such a disease is extreme. Tailoring the best treatment approach is the mainstay of modern and effective management. By revealing novel agents, more effective regimens arise to manage any experienced component of the metabolic cluster. The pharmacological management of the metabolic triad represents a very active field of interactive research. Mono or combined therapy of novel agents, including insulin treatment and older agents (statins and metformin), needs to be tailored individually.
We review the recent literature data regarding the link between NAFLD, MetS, and T2DM and current treatment options for patients with this pathological condition.
NAFLD in general
The prevalence of NAFLD worldwide is estimated to be 23–25%, with the projection that the incidence will increase in the coming decades [22–25]. The burden of NAFLD differs globally, from the highest prevalence of 32% in the Middle East and 30% in South America, over 24% in North America and Europe, to the lowest prevalence of 13% in Africa [3, 26]. In addition, the prevalence of NASH was confirmed in 20% of subjects with NAFLD [25, 27]. However, there are some inconsistencies between epidemiological studies, such as NAFLD diagnostic (ultrasound-based or serum markers), the number of extensive epidemiological studies from developing countries, etc. Despite some discrepancies between the local and global prevalence of NAFLD, the disease burden is higher in subjects with elevated body mass index (BMI) and among patients with T2DM [23, 24].
The origin of NAFLD is a complex and incompletely defined process still in the realm of hypothesis. Firstly, the pathogenesis of NAFLD was explained as a two-hit hypothesis [28]. The first hit applies to hepatic lipid accumulation and IR, while the second hit refers to inflammation, mitochondrial dysfunction, and oxidative stress that promote disease progression and eventually cirrhosis [29]. The multiple-hit hypothesis for NAFLD pathogenesis is widely accepted because it involves a more comprehensive view. This theory emphasized the role of genetic and environmental factors in metabolic dysfunction and disturbing connection between organs, especially the liver, adipose tissue, pancreas, and gut [29–31].
Contemporary understanding of NAFLD as an influential metabolic disease with possible distant consequences has induced the change of the name, from NAFLD to metabolic (dysfunction)-associated fatty liver disease (MAFLD) [32–35]. Metabolic (dysfunction)-associated fatty liver disease is a clinical diagnosis and does not require histology analysis of liver biopsy specimens [36]. It includes the presence of steatosis (detected by imaging or biomarkers or liver specimen histology) and either T2DM or overweight/obesity or 2 of the following: increased waist circumference, arterial hypertension, increased serum triglycerides, decreased HDL-cholesterol lipoproteins, increased C-reactive protein level, the presence of prediabetes, or insulin resistance [34]. The definition of MAFLD emphasizes the metabolic character of the disease and points out preventive measures regarding NAFLD pathophysiology chain interruption transfer from simple steatosis to liver fibrosis and cirrhosis and HCC [33, 34].
Epidemiological and cohort studies indicated inheritance in NAFLD but were insufficient to enable the mapping of certain genes of interest and qualify them as treatment targets [6]. With the development of modern genotypic arrays, genome- and exome-wide association studies (GWAS and EWAS) have become feasible, thus enabling the detection of different exonic variants associated either with full-spectrum or certain categories of NAFLD (steatosis, inflammation or fibrosis) by whole-exome sequencing (WES) [37, 38]. Genetic variants associated with full-spectrum NAFLD are missense SNP in PNPLA3 (rs738409) encoding p.I148M and missense variant rs58542926 encoding p.E167K in TM6SF2 [39, 40]. Additionally, pleiotropic genetic variants, such as GCKR rs 1260326, MBOAT7, and MARC1, are associated with certain categories of NAFLD: steatosis, inflammation, and liver fibrosis/cirrhosis [41–44]. However, some genetic variants are associated with individual NAFLD stages, such as PPP1R3B, PYGO1, APOE, and GPAM with steatosis [41, 44, 45]. Additionally, LEPR and HSD17B13 variants are associated merely with NASH and NASH and cirrhosis, respectively [40, 41]. The bioinformatics analysis identifies a number of pathways, including metabolism and PPAR signalling pathways, which were included in the NAFLD pathogenesis [46].
The connection between NAFLD, MetS, and T2DM
NAFLD is not only liver disease but a multisystem disorder. It is connected with MetS, IFG, IGT, and T2DM, and they have an increased risk of CVD [47, 48]. Such a strong association promotes MAFLD, presented with overweight/obesity, T2DM, or evidence of metabolic dysregulation in subjects with liver steatosis [34]. Recently, it was shown that the blood level of betatrophin, a liver hormone that regulates glucose and lipid metabolism, tends to decline during the progress of NAFLD, which may cause glucose intolerance [49]. In addition, NAFLD is associated with numerous systemic diseases, such as chronic kidney disease (CKD) and colorectal carcinoma [50].
In clinical practice, abdominal ultrasound and liver biopsy are widely used to assess the severity of NAFLD/NASH. Ultrasound diagnosis of NAFLD is the most commonly used method because it is easily applicable with high sensitivity (84.8%) and specificity (93.6%) [51, 52]. A disadvantage of abdominal ultrasound is its limited capacity for diagnostic of degrees of hepatic steatosis, especially in patients with high BMI [53–56]. Liver biopsy is still the gold standard for assessing the severity of NAFLD, but invasiveness is a limiting factor. In addition, screening the potential of extra-hepatic manifestations is an integral part of managing NAFLD patients [50, 57]. NAFLD usually manifests itself asymptomatically or only biochemically as a slightly elevated level of serum transaminases [58]. Therefore, serum transaminases are not sensitive markers of the presence of NAFLD [58, 59]. In the case of advanced disease with NASH, liver fibrosis, and cirrhosis, clinical manifestations are more pronounced than isolated NAFLD. Occasionally, it may present as right upper abdominal pain, nausea, the urge to vomit, gastric or intestinal motility complaints, and jaundice. As chronic liver disease progresses, clinical presentations of decompensated cirrhosis and liver failure occur. The appearance of unexplained fever, weight loss, or haemorrhagic ascites may indicate the most severe complication of NAFLD, HCC, followed by an increase in serum α-fetoprotein [58, 60–63].
The frequency of liver steatosis is significantly higher in obese individuals and patients with T2DM (observed in ~45% and 70% of subjects, respectively) [64]. On the other hand, there is a significantly higher risk of development of T2DM in patients with NAFLD [65]. Therefore, NAFLD is defined as the hepatic manifestation of MetS [66]. According to meta-analyses, the prevalence of NAFLD, NASH, and severe liver fibrosis (stage F ≥ 3) in patients with T2DM is 57.8%, 65.26%, and 15.05%, respectively [3, 67]. On the other hand, the prevalence of MetS in patients with NAFLD and NASH is 41 and 47%, respectively [3, 68]. Interaction between T2DM and NAFLD/NASH is bi-directional [69]. T2DM is observed in approximately a quarter of patients with NAFLD/NASH, whereas NAFLD occurs in three-quarters of patients with T2DM [70, 71].
Unhealthy and high-calorie food, excessive consumption of saturated fats and refined carbohydrates, sweetened beverages, and fructose, and a lack of physical activity and sedentary lifestyle significantly influence the occurrence of obesity and NAFLD [72]. In a certain number of diseased individuals, it is observed that some genetic factors (such as the presence of PNPLA3I148M and TM6SF2E167K polymorphisms) may determine the severity of NAFLD and influence the course of the disease to more advanced forms [73–75]. Recently, it was found that fibroblast growth factor 21 may be a reliable marker of inflammatory processes in the liver of obese subjects [76].
Due to global epidemics of T2DM and obesity, a significant increase in prevalence is expected for MetS and CVD [9]. Most patients with T2DM also have MetS [77]. Patients with MetS have a doubled risk of CVD occurrence compared to those without MetS [77]. Finally, MetS is associated with a 5-fold higher probability of occurrence of T2DM [78].
Patients with T2DM and NAFLD/NASH have a 2-fold higher risk of development and progression of CVD [48, 79] and 2- to 3-fold higher risk of death caused by chronic liver diseases than patients with T2DM without NAFLD [80]. T2DM is an independent predictor of general mortality and mortality caused by liver disease [81]. The risk of development of T2DM in patients with NAFLD/NASH is 33–55% [82]. Patients with NAFLD/NASH have an almost 2-fold higher risk of developing T2DM in 5 years of monitoring [83]. In addition, the progression of liver disease and increased morbidity and mortality are detected in lean subjects with NAFLD [84, 85].
The quality of glycaemic regulation determines the risk of CVD. Thus, IFG, IGT, and/or increased levels of HbA1c are associated with a higher risk of coronary disease [86]. Even if in the reference range, high normal glycaemic values may predict an increased risk of coronary disease and fatal outcomes independently of traditional risk factors for CVD [87]. Treatment of T2DM decreases the proportion of fat in the liver [88].
Patients with T2DM have a higher chance of developing NASH from NAFLD than those without diabetes [89, 90]. In patients with T2DM, the appearance of fatty liver is registered significantly earlier than diabetes vascular complications [91]. Therefore, early detection of NAFLD/NASH in patients with T2DM is of great importance. Determination of biomarkers of oxidative stress, dyslipidaemia, and inflammation can be beneficial [88]. Also, T2DM [92] and NAFLD [93] are the most important factors of risk for the development of chronic kidney disease (CKD), and the contribution of CKD to the development of CVD is much higher when associated with these conditions [94]. This leads to the development of the so-called “triad disease” consisting of NAFLD/NASH, CKD, and T2DM, which has great significance for public health, primarily because of the increasing incidence of CVD-associated morbidity and mortality [21, 94]. Clinical manifestation of NAFLD-related CVD varies and includes endothelial dysfunction, atherogenic dyslipidaemia, hypertension, altered gastrointestinal (GIT) microbiota, systemic inflammation, and cardiomyopathy [48, 95, 96]. Considering this connection, screening for CV risk factors in patients with NAFLD is strongly recommended [1, 97, 98]. Also, IR and T2DM are significant factors in liver fibrosis occurrence and development in patients with NAFLD [99, 100]. Four entities describe the link between T2DM and liver diseases: incidental and simultaneous existence of entities (which occurs very frequently), diabetic hepatopathy (a liver disease caused by diabetes), hepatogenous diabetes (diabetes caused by chronic liver disease), and liver disease that occurs coincidentally in patients with DM [101]. NAFLD/NASH, NASH-induced liver cirrhosis, and HCC belong to the subgroup of chronic liver diseases worsened by diabetes [62, 102]. Liver diseases that coincide with diabetes com prise haemochromatosis, autoimmune liver disease, and biliary duct diseases [103–105].
The pathophysiological pathway in which T2DM leads to NAFLD/NASH could be partially explained by chronic inflammation associated with IR, increased uptake of free fatty acids (FFA) by the liver, lipotoxicity, and development necroinflammation [106]. Accumulation of products of lipid metabolism (ceramides, diacylglycerol) leads to hepatic IR, increased gluconeogenesis, oxidative stress, and depletion of pancreatic β-cells [107]. On the other hand, NAFLD in patients with T2DM is associated with IR, poor metabolic control [108], and a higher incidence of micro- and macrovascular complications of diabetes [109, 110]. In contrast, improvement of NAFLD decreases the risk of occurrence of T2DM by approximately 70% [111].
Due to the frequent and strong association between T2DM and NAFLD/NASH, it is necessary to screen all patients with T2DM for the presence of NAFLD and vice versa [101, 112, 113]. For diagnostics of perturbations of glucose metabolism in patients with chronic liver diseases, the most reliable is the oral glucose tolerance test (OGTT) [114] because most of these patients have normal values of morning glycaemia [112]. HbA1c can serve as an indicator of the quality of retrograde glycaemic regulation in compensated chronic hepatic liver disease, as opposed to decompensated conditions, where it is advised to determine the level of fructosamine as an alternative marker. To assess the quality of daily glycaemic regulation and efficiency of diabetes therapy, it is helpful to measure glycaemia frequently during the day or optimally to perform continuous monitoring of glycaemia, if available [101, 112, 113].
Management of NAFLD/NASH, MetS, and T2DM
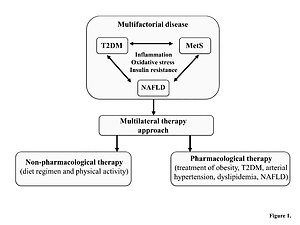
Treatment of NAFLD and MetS, which frequently co-exist in the same patient, requires a multifactorial approach consisting of non-pharmacological measures (such as diet regimen and physical activity) and pharmacological measures (treatment of obesity, arterial hypertension, T2DM, dyslipidaemia) to achieve improvement in the biochemical and histological presentation of NAFLD/NASH and reduction of cardiovascular risk [20, 115] (Figure 1). The primary goal of MetS treatment is to decrease the risk of CVD [9], and therefore the management is directed towards lowering elevated levels of atherogenic lipids and treating arterial hypertension and T2DM [116].
Figure 1
Multilateral therapy approach for the treatment of multifactorial disease
MetS – metabolic syndrome, NAFLD – non-alcoholic fatty liver disease, T2DM – type 2 diabetes mellitus.
If non-pharmacological measures, such as body weight reduction, and change in physical activity do not yield favourable results, it is necessary to introduce pharmacological therapy [9, 117]. Also, no unified diet is recommended for NAFLD management [118]. There is still no single drug that can be used alone to treat MetS [9]. Currently used medications for individual components of MetS, such as arterial hypertension, T2DM, and atherogenic dyslipidaemia, positively reduce inflammation [117, 119].
No guidance recommends treatment with one particular medication for NAFLD/NASH with or without T2DM. Newer antihyperglycaemic agents, such as dipeptidyl peptidase-4 inhibitors (DPP4i) (sitagliptin, saxagliptin, vildagliptin, alogliptin, linagliptin) and glucagon-like peptide-1 receptor agonists (GLP1-RA) (exenatide, lixisenatide, liraglutide, dulaglutide, and semaglutide), or sodium-glucose transport protein 2 inhibitors (SGLT2i) (cana-/empa-/dapagliflozin), may be helpful in the treatment of NAFLD/NASH, decreasing the overall content of fat in the liver, and probably inflammation and fibrosis [120]. Additionally, they decrease the occurrence of CKD, which manifests either independently or in association with NAFLD/NASH, T2DM, or CVD [89]. GLP1-RAs, the structural homologues to the natural incretin glucagon-like peptide-1 (GLP-1), stimulate glucose-dependent pancreatic insulin secretion, reduce glucagon secretion, and slow down gastric emptying [121, 122]. Similarly, gliptins or DPP4i promote an increase in natural incretin levels such as GLP-1 and gastric inhibitory peptide (GIP) by blocking the dipeptidyl peptidase-4 (DPP4) enzyme involved in the degradation of natural incretins. The elevated incretin levels act on a simultaneous increase in glucose-dependent insulin secretion and decrease glucagon secretion [123, 124].
Other medications used for the treatment of T2DM, metformin and pioglitazone, lead to improved biochemical, ultrasonographic, and/or histological presentation in patients with NAFLD/NASH [125–133]. Thiazolidinedione, such as pioglitazone, activates the PPARγ receptors and decreases insulin resistance in various tissues, predominantly in skeletal muscles and the liver [134, 135]. Conflicting results exist regarding the use of sitagliptin [136, 137]. In patients with T2DM and NAFLD/NASH, combined therapy consisting of statin and liraglutide with or without SGLT2i is very potent and helpful, especially in reducing hepatic and cardiovascular morbidity and mortality in such patients [89, 138–140]. SGLT-2i reduces proximal tubule glucose reabsorption by binding to the SGLT-2 receptors, thus eliminating glucose urinary. Some studies emphasize the favourable effects of SGLT2i regarding major adverse cardiovascular events and congestive heart failure deterioration [141–143]. Renin-angiotensin blockers and antihypertensive medications are helpful additional therapy for patients with NAFLD/NASH [144]. Treatment with insulin degludec/aspart (IDegAsp) co-formulation improves hypoglycaemia, insulin requirement, and body mass of T2DM patients [145]. Besides novel therapies, statins and metformin have been shown as well-proven treatments for metabolic triad. Statins, as the inhibitors of the hydroxymethylglutaryl-CoA (HMG-CoA) reductase enzyme, inhibit a key step in the sterol biosynthetic pathway [146], while metformin acts on complex I inhibition, leading to AMPK activation, and alters cellular redox balance [147].
Growing evidence supports the effectiveness without adverse effects of various lipid-lowering nutraceuticals [148]. Appropriate therapy with silymarin, vitamin D and E, polyunsaturated fatty acids of the omega-3 series, coenzyme Q10, curcumin, and berberine with concomitant lifestyle changes can beneficially affect subjects with NAFLD [149]. Because CVD is the leading cause of fatal outcome in patients with NAFLD, it is important to use adequate therapy to prevent disease progression. Although a few guidelines for managing NAFLD are recommended by various scientific societies related to hepatology, some important issues remain unclear. The most important doubts are related to the definition of NAFLD, some directions for clinical practice, the need to monitor high-risk patients, and affordable non-invasive tests, including the new biomarkers for NAFLD diagnosis, etc. [150, 151]. One doubt is concerned with systematic screening for NAFLD in diabetic or obese subjects to prevent NASH and advanced fibrosis development, but it is not cost-effective [70, 152, 153]. Furthermore, currently using hepatic biomarkers for NAFLD screening is insufficient, considering false-negative results [153, 154]. In addition, the reason for differences between various guidelines is caused more by population characteristics, including genetics and lifestyle, screening strategies, and primary health care, than the inability to find unique attitudes [150, 151]. Despite some inconsistencies, we strongly recommended using existing Clinical Practice Guidelines, with preference being given to the use of local or institutional guidelines. The Position Paper endorsed by the International Lipid Expert Panel (ILEP) upgrades currently used guidelines on managing lipids in patients with atherosclerotic CVD [155]. Numerous experts from several European countries summarized data and presented draft practice recommendations and strategies for optimal lipid management considering the cost-effectiveness. The ILEP Position Paper explains in more detail practical solutions focusing on immediate combined lipid-medicated therapy in patients with high cardiovascular risk [155]. In addition, lipid-lowering therapy is suggested and the term “extremely high risk” has been proposed for a group of patients with acute coronary syndrome [155].
Conclusions
The timed treatment of NAFLD and MetS contributes to the prevention of T2DM. Non-pharmacological measures carried out in the management of NAFLD and MetS present the non-pharmacological mainstream in T2DM management at the same time. The optimal pharmacological treatment of T2DM is provided by novel antihyperglycaemic drug classes (i.e. SGLT2i, DPPi, GLP1-RA), sometimes combined with insulin sensitizers (metformin and pioglitazone), preventing the occurrence or progression of NAFLD. If all three entities already co-existed in the same patient, the concomitant management and nutraceuticals significantly decreased cardiovascular morbidity and mortality. Experience from everyday clinical practice shows that the treatment of the primarily presented entity of the “metabolic triad” significantly determines the presentation and treatment of another entity.
A more thorough investigation involving different specialities is needed to answer the complex natural history of NAFLD, enabling its more effective management. Connections between NAFLD, MetS, and T2DM lead to a complex multifactorial disease. The proper understanding of these connections and an early diagnosis and monitoring of existing conditions contribute to establishing effective targeted treatment.