Introduction
Endometriosis is a chronic gynecological disease, and this disease is defined by the presence of endometrial tissue outside the uterine cavity, which can cause inflammation, pain and infertility [1, 2]. The incidence of endometriosis is about 10% of reproductive-aged women worldwide, and it is a significant source of physical and mental health loss [3]. The condition is often associated with menstrual cramps, pain during intercourse, and chronic pelvic pain that significantly interferes with daily activities and well-being [4, 5]. Over the past few years, there has been an increased emphasis on the psychological effects of endometriosis. Research conducted by various authors indicates that this condition elevates the risk of developing depression and anxiety [6, 7].
Endometriosis and mental health relate to different biopsychosocial factors. Pelvic pain caused by endometriosis has a negative impact on both physical well-being and psychological well-being, reducing the ability to cope with stress and increasing feelings of hopelessness [8–10]. Patients with endometriosis are usually diagnosed late, which leads to a longer duration of suffering and frustration [11]. Moreover, due to cultural taboos regarding pain and gynecological problems, women often lack social support for the psychological ramifications of the disease [12]. These challenges highlight the need to explore the mental health aspects of endometriosis in detail to enhance the understanding of management approaches [13].
Endometriosis and mental health issues are intertwined and cannot be easily separated [14]. The pain is often chronic and thus can cause depression and psychological distress; there is often a delay in receiving a diagnosis, and menstrual pain is still viewed as normal by society, which makes women feel unheard and unappreciated [15]. Moreover, it has been proposed that there is a bidirectional relationship between endometriosis and mental health which may be mediated by such common factors as inflammation, hormonal imbalance, and neuroendocrine alterations in response to stress [16]. Despite the increasing awareness of such challenges, however, systematic reviews of the literature examining this relationship are still scarce [17].
This study reviewed and meta-analyzed the literature on the relationship between endometriosis and mental health, hoping to identify the risk factors that can predict the mental health of patients with endometriosis and provide certain recommendations for clinical treatment.
Methods
The present systematic review and meta-analysis adhered to the guidelines set out by the PRISMA statement. This meta-analysis has been registered in PROSPERO, and the PROSPERO ID of this study is 1067012. The following sections describe the methodological approach used in this research.
Search strategy
An effective search plan was designed to identify studies that have examined the link between endometriosis and mental health, concentrating on depressive episodes. These databases included PubMed, Cochrane Library, and Google Scholar. Search terms included combinations of the following keywords: “endometriosis”, “mental health”, “depression”, “anxiety”, “psychological distress”, and “quality of life”. The MeSH terms are “endometriosis” and “mental illness”, and the free words are “mental health”, “depression”, “anxiety”, “psychological distress”, and “quality of life”. MeSH terms + free terms were used for searching. The use of Boolean operators such as AND and OR was used to narrow down the search outcomes. The following limitations were applied while searching: Only articles in the English language were considered, and no year limitations were imposed to ensure comprehensiveness of coverage. It should be noted that the presented search was updated in [specific month and year].
Inclusion and exclusion criteria
Studies were included if they met the following criteria:
Participants were women with a confirmed diagnosis of endometriosis.
The study assessed mental health outcomes, specifically depressive events.
Original research studies utilizing cross-sectional, cohort, case-control, or population-based designs.
Studies reporting quantitative data on depression linked to endometriosis.
Articles published in peer-reviewed journals.
Exclusion criteria included:
Study screening
Selection of studies for the review was done in three steps. First, titles and abstracts of the articles identified through the database searches were reviewed for relevance. Second, the titles and abstracts of the searched publications were screened to determine the applicability of the inclusion and exclusion criteria to the full-text articles. The screening process was conducted in a blinded manner by two authors, and any disagreements were resolved through conferencing or consulting with a third author.
Data extraction
Data extraction was conducted manually by two authors using a data extraction form. Data elements extracted were the study details such as author, year, country, study type, sample size, and diagnostic criteria used, participant characteristics, mental health outcomes such as prevalence of depression, and statistical data such as effect size and confidence intervals. In case of inconsistency in the extracted data, the problem was discussed and resolved among the reviewers.
Quality assessment
The quality of the included studies was assessed based on the Newcastle-Ottawa Scale (NOS) for case-control studies. NOS was used to score all the included literature, and the following 8 questions were judged and scored. In addition to the maximum of 2 stars for comparability, there was a maximum of 1 star for other items, and the total possible score was 9 stars – the higher the score, the higher the quality of the study [18]. The NOS assesses three domains: inclusion criteria, matching of the groups, and definition of the outcomes. Both authors separately reviewed each study and resolved any difference in opinion to reach a consensus. Table I shows the quality assessment of the studies involved in the systematic review and meta-analysis.
Table I
Quality assessment of included studies using the Newcastle-Ottawa Scale (NOS)
| Study authors | Selection (max. 4) | Comparability (max. 2) | Outcome/Exposure (max. 3) | Total score (max. 9) |
|---|---|---|---|---|
| Friedl et al., 2015 | 4 Representativeness of sample, selection of controls, definition of exposure, ascertainment of endometriosis | 2 Adjustment for confounders, e.g., age | 3 Adequacy of follow-up, blinded outcome assessment, validated measurement tools | 9 |
| Škegro et al., 2021 | 4 Representativeness of sample, consecutive patients, exposure definition, ascertainment of endometriosis | 2 Adjustment for pain severity, age | 3 Validated tools for mental health, blinded outcome assessment, statistical clarity | 9 |
| Gao et al., 2020 | 4 Population-based registry, validated exposure definition, representativeness, large sample | 2 Adjustment for confounders, e.g., age, comorbidities | 3 Administrative database, blinded outcome data, validated registry | 9 |
| Estes et al., 2021 | 3 Validated exposure definition, representativeness, incomplete description of controls | 2 Adjustment for pain, comorbidities | 3 Validated outcome measurement, large cohort, use of health claims | 8 |
| Chen et al., 2016 [30] | 4 Large sample size, validated exposure, population-based registry, representativeness | 2 Adjustment for demographics, comorbidities | 3 Adequate follow-up, registry-based outcome assessment, statistical robustness | 9 |
| Márki et al., 2017 | 3 Small sample size but well-defined criteria, validated exposure, limited representativeness | 1 Adjustment for demographics only | 3 Validated tools for mental health, appropriate follow-up | 7 |
| Marschall et al., 2021 | 3 Small sample size, well-defined criteria, limited representativeness | 2 Adjustment for narrative identity, pain | 3 Validated mental health tools, robust statistical methods, blinded assessment | 8 |
| Wang et al., 2023 | 4 Population-based registry, large sample, representativeness, validated exposure | 2 Adjustment for demographic and clinical factors | 3 Validated tools for psychiatric assessment, long follow-up | 9 |
| Facchin et al., 2017 | 3 Limited sample, validated exposure definition, representativeness issues | 1 Adjustment for pain only | 3 Validated mental health tools, rigorous statistical analyses | 7 |
Sensitivity/heterogeneity tested by one-by-one elimination method
After eliminating each included study in sequence, a meta-analysis was re-conducted on the remaining studies to observe the changes in the combined effect size and confidence interval. If significant changes occur after excluding one study, it indicates that the original conclusion may have been overinfluenced by that study, is at risk of bias, or lacks robustness.
Heterogeneity of binary categorical variables
The L ‘Abbe plot was used for the meta-analysis heterogeneity test of the binary variable data from RCTs. In this study, the presence or absence of depression and anxiety can be determined, which was applicable to binary categorical variables. The incidence of events in the treatment group was plotted relative to that in the control group for each study. If the study results were homogeneous, all points would be linearly distributed. Significant deviations from this line indicated heterogeneity in the study results.
Meta-regression analysis
A regression model to explore the relationship between research characteristics (covariates) and effect size (relative risk – RR) was established, thereby explaining the heterogeneity among different studies. This study conducted a meta-regression analysis using a random effects model. The random effects model assumes that the studies did not have a common effect scale, but rather each had its own effect scale, which was defined as a random variable that follows a normal distribution.
Data synthesis
Meta-analysis was performed using R software, version 4.2.3. Depressive events concerning endometriosis were evaluated employing random-effects models as a way of managing heterogeneity of the studies. The main measure of interest was the overall pooled prevalence of depressive symptoms in women with endometriosis compared to the control group. The heterogeneity was estimated by the I2 statistic. Stata 17 software was used to plot the heterogeneity shown by the elimination method and the meta-regression analysis graph.
Results
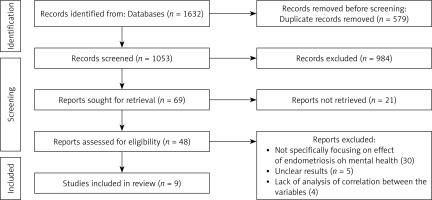
When the databases were searched exhaustively, 1632 articles were found. After excluding the duplicate records and using the inclusion and exclusion criteria, nine articles were included in this systematic review. The PRISMA flow diagram outlining the selection of the included studies is shown in Figure 1. The quality of the included studies was evaluated with the Newcastle-Ottawa Scale (NOS) for selection, comparability, and outcome/exposure. Table I presents the quality assessment of the included studies, where all the selected articles have met the methodological standards. NOS scores of all included documents were greater than or equal to 7, and the documents [19–21] were scored with a full score of 9. The overall quality of the included literature was relatively high.
Study characteristics
The combined studies presented in this review reflect various populations, designs, and geographical areas, providing a broad perspective on the association between endometriosis and mental health. These studies were conducted in countries such as Austria, Croatia, Sweden, United States, Taiwan, Hungary, Denmark, and Italy and were published between 2015 and 2023. The type of studies used in the review were cross sectional, case control, prospective cohort, and population based.
The sample sizes ranged from 62 participants in some research to more than 850,000 women in others. Participants were mainly female endometriosis patients who were diagnosed using histological confirmation, imaging, or through registry diagnostic codes. Table II displays the study characteristics such as diagnostic methods, mental health outcomes, and measurement tools.
Table II
Detailed characteristics of included studies
| Study authors | Year | Country | Study design | Sample size | Population | Diagnostic method | Mental health outcomes | Measurement tools | Key findings | Conclusion |
|---|---|---|---|---|---|---|---|---|---|---|
| Friedl et al., 2015 | 2015 | Austria | Cross-sectional survey | 62 patients, 61 controls | Women aged 18–44 with confirmed endometriosis | Histological confirmation | Anxiety, depression | SF-36, HADS-D, EHP-30 | Moderate to severe anxiety (29%) and depression (14.5%) in patients. SF-36 showed significant impairments in general health and mental health in patients (p < 0.001). | Need for psychosomatic treatment due to elevated mental health burden in patients. |
| Škegro et al., 2021 | 2021 | Croatia | Observational cross-sectional | 79 women | Women with histologically confirmed endometriosis | Histological confirmation | Depression, anxiety, stress | EHP-5, DASS-21, VAS | Depression (44.3%), anxiety (25.3%), stress (31.7%). Moderate correlations between EHP-5 and mental health indicators (r > 0.5). | Multidisciplinary care required to address mental health and physical symptoms in endometriosis. |
| Gao et al., 2020 | 2020 | Sweden | Longitudinal cohort study | 854,361 (14,144 patients) | Women born 1973–1990, aged 14–43 | ICD-9/10 codes in national registry | Depression, anxiety, ADHD, alcohol/drug dependence | National patient register | Women with endometriosis had higher RRs for mental health outcomes: depression (RR = 1.89), anxiety (RR = 1.82), alcohol dependence (RR = 1.93). Bidirectional associations observed between depression/anxiety and endometriosis. | Comorbidity with depression/anxiety suggests shared familial liability. Multidisciplinary care recommended. |
| Estes et al., 2021 | 2021 | USA | Retrospective cohort study | 72,677 patients, 147,251 controls | Women aged 18–50 with endometriosis | ICD-9/10 codes and laparoscopic confirmation | Anxiety, depression, self-directed violence | Claims data from health database | RRs: Anxiety (1.38), depression (1.48), self-directed violence (2.03). Pain-related comorbidities were significant risk factors. | Regular screening and care for mental health outcomes are crucial for women with endometriosis. |
| Chen et al., 2016 [30] | 2016 | Taiwan | Longitudinal cohort study | 10,439 patients, 10,439 controls | Women aged ≥ 18 with no psychiatric history | ICD-9-CM codes, ultrasonography | Major depression, anxiety | NHIRD data | RRs for depression (1.56), anxiety (1.44). Younger women (< 40 years) at higher risk. | Comprehensive care addressing physical and psychological needs is essential. |
| Márki et al., 2017 | 2017 | Hungary | Cross-sectional study | 193 women | Women aged 18–50 years | Gynecological evaluation, imaging | Anxiety, depression, psychological distress | SF-36, HADS, PSS, DERS | Anxiety symptoms (54.79%), depressive symptoms (20.32%). Pain and emotion regulation difficulties significantly reduced HRQoL. | Pain management and emotional regulation interventions can enhance HRQoL. |
| Marschall et al., 2021 | 2021 | Denmark | Cross-sectional study | 120 women | Women aged 18–48 years | MRI, ultrasound, surgery | Depressive symptoms, life satisfaction, psychological impact | BDI-II, SWLS, CES, narrative coding | Centrality of endometriosis to identity correlated with depressive symptoms (r = 0.50) and reduced life satisfaction (r = –0.41). Agency themes linked to improved mental health outcomes. | Importance of narrative identity in understanding mental health in endometriosis patients. |
| Wang et al., 2023 | 2023 | Taiwan | Population-based cohort study | 100,770 (20,154 patients) | Women aged ≥ 18 | ICD-9-CM codes in NHIRD | Anxiety, depression, suicide, all-cause mortality | NHIRD data | RRs: anxiety (2.494), depression (2.773), suicide (1.447), all-cause mortality (2.315). | Psychiatric follow-up and multidisciplinary care are vital to improve outcomes. |
| Facchin et al., 2017 | 2017 | Italy | Cross-sectional study | 210 women | Women aged 19–51 years | Clinical and/or surgical diagnosis | Depression, anxiety, rumination | HADS, RRS, RSES, BES | Pelvic pain severity correlated with poorer mental health. High self-esteem and emotional self-efficacy associated with lower depression and anxiety (p < 0.001). | Multidisciplinary treatments should address both physical and psychological needs, including self-esteem and emotional regulation. |
Mental health outcomes in women with endometriosis
Prevalence of depression and anxiety
Each of the studies included in the systematic review and meta-analysis found that women diagnosed with endometriosis had a significantly higher rate of depression and anxiety, particularly depression and anxiety, compared with the general population. In their study, 27.7% of women with endometriosis had moderate to severe anxiety levels and 14.5% had depressive symptoms [19]. Similarly, high prevalence of depressive symptoms (44.3%), anxiety (25.3%), and stress (31.7%) among the participants was reported [20].
Specifically, pain severity was found to be a significant predictor of mental health disorder prevalence. In their cross-sectional study, higher pain severity was positively associated with higher anxiety and depressive symptoms and lower HRQoL [22]. This was in line with other studies showing that pain has a significant effect on mental health status.
Factors influencing psychological distress
The timing of diagnosis and patient characteristics were found to be significant predictors of psychological distress. It was established that shorter time between the diagnosis and the assessment was linked to increased anxiety levels [23]. In addition to this, greater self-esteem and self-efficacy were found to be protective factors and women with higher scores on both measures indicated lower levels of depression and anxiety. A study showed the psychological consequences of the narrative identity of women with endometriosis [24]. It was found that women who had a high level of endogenous factors related to endometriosis had higher levels of depressive symptoms and lower life satisfaction. On the other hand, higher agency and communion themes in their stories correlated with better psychological well-being.
Association with comorbidities and long-term risks
Several authors have described the presence of comorbid depression in patients with endometriosis. In the study by Gao et al. (2020) [21], the women with endometriosis had 1.89 times higher risk of developing depression and 1.82 times higher risk of developing anxiety. In a different study, endometriosis was associated with a more than twofold elevated risk of SV [25].
Furthermore, it was also possible to identify long-term outcomes including suicidality and all-cause mortality. In one study, women with endometriosis were at a 44.7% higher risk of suicide and a 231.5% higher risk of all-cause mortality, proving the importance of a holistic approach [26].
Quality of life and mental health
In all the studies reviewed, endometriosis was found to be significantly related to decreased HRQoL. There was a statistically significant decrease in the general health, vitality, and mental health aspects of the HRQoL scales [19, 22]. These outcomes were mainly associated with psychological distress, pain severity, and the presence of emotional dysregulation.
Data synthesis
Anxiety outcomes
The meta-analysis revealed a significant association between endometriosis and anxiety (Figure 2), with a pooled relative risk (RR) of 2.82 (95% CI: 1.69–4.68, p < 0.001) under a random-effects model. This finding indicates that women with endometriosis have nearly three times the risk of developing anxiety compared to control groups. The heterogeneity among the studies was substantial, as reflected by an I2 value of 100% and τ2 = 0.6032 (p < 0.001), suggesting variability in study populations, methodologies, and diagnostic criteria.
Figure 2
Forest plot for anxiety outcomes. The pooled relative risk (RR) of 2.82 (95% CI: 1.69–4.68) indicates a significantly higher risk of anxiety among women with endometriosis
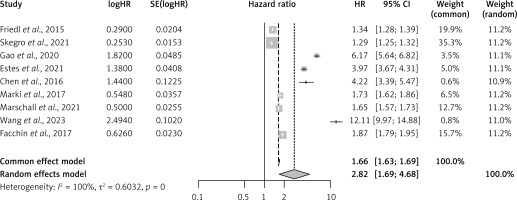
The precision of the pooled effect was supported by the log-transformed RR (logRR = 0.59) and its standard error (SE = 0.12), confirming the robustness of the findings. The 95% confidence interval spanned from moderate (RR = 1.69) to high risk (RR = 4.68), further emphasizing the significant burden of anxiety among women with endometriosis.
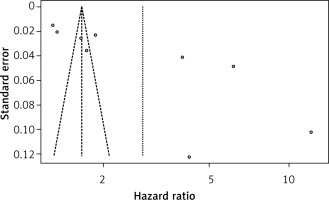
The funnel plot for anxiety outcomes (Figure 3) displayed moderate asymmetry, which may suggest the presence of publication bias or small-study effects. This observation was supported by visual inspection and statistical heterogeneity values. The clustering of smaller studies near higher effect sizes, as evident in the plot, highlights the need for sensitivity analyses to ensure the stability of the pooled estimates.
Depression outcomes
For depression, the meta-analysis demonstrated a pooled relative risk (RR) of 2.93 (95% CI: 1.63–5.25, p < 0.001) using a random-effects model (Figure 4). This result indicates that women with endometriosis have nearly a threefold higher risk of experiencing depressive symptoms or clinical depression compared to controls. The heterogeneity was pronounced, with I2 = 100% and τ2 = 0.794 (p < 0.001), reflecting variability across studies in terms of sample sizes, population characteristics, and measurement tools.
Figure 4
Forest plot for depression outcomes. The pooled relative risk (RR) of 2.93 (95% CI: 1.63–5.25) highlights the elevated risk of depression among women with endometriosis
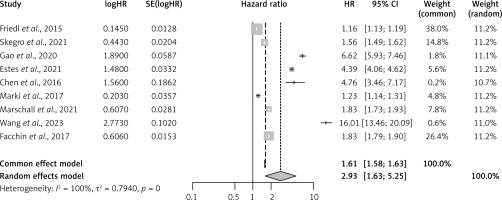
The log-transformed RR for depression outcomes (logRR = 0.61) and its standard error (SE = 0.15) further validated the precision of the pooled effect. The 95% confidence interval showed a wide range, from moderate risk (RR = 1.63) to substantial risk (RR = 5.25), indicating that the impact of endometriosis on depression may vary based on pain severity, disease stage, and psychosocial factors.
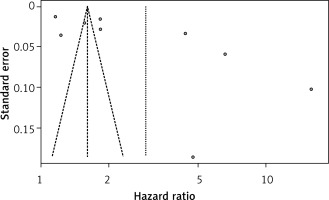
The funnel plot for depression outcomes (Figure 5) revealed some asymmetry, which could be attributed to potential publication bias or methodological differences across studies. Studies with smaller sample sizes tended to show larger effect sizes, as visualized in the plot. The presence of outliers and clustering in specific regions of the plot suggests that further analyses, such as trim-and-fill methods, may be necessary to address potential biases.
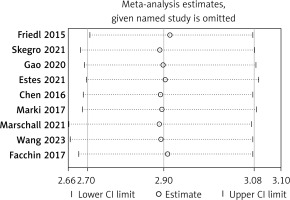
One-by-one elimination method outcomes
The outcomes of this study concerned 9 studies, each study being excluded in turn. The combined results of the remaining 8 studies were not statistically significant (95% CI included 2.82 and 2.93), which was consistent with the original combined results (RR = 2.90, 95% CI = 2.70 to 3.08, p < 0.001) (Figure 6), indicating that the results were relatively stable.
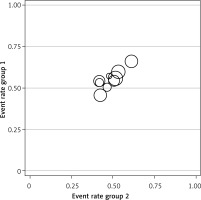
Heterogeneity of binary categorical variables
It can be seen from Figure 7 that some points were far from the reference line, indicating heterogeneity in the study results.
Meta-regression analysis
Meta-regression analysis was conducted on 9 included studies. As shown in Table III, I2 = 76.37% (I2 > 50%), indicating that this meta-analysis has certain heterogeneity. However, the p-value > 0.05 suggests that there was no need for subgroup analysis.
Discussion
This systematic review focuses on understanding the association between endometriosis and mental health, providing a detailed analysis of the interconnection between the two. The results support the hypothesis that women with endometriosis have significantly elevated prevalence of depression, anxiety, and psychological distress compared to the general population. This review offers a more complex view of the contributing factors, which include pain severity, diagnostic latency, and patient-level factors such as self-esteem and emotional self-efficacy, which supports a biopsychosocial model of treatment.
The burden of endometriosis on mental health
Endometriosis is defined as a chronic and severe disease that has negative impacts on the mental state of women. In line with previous research, the current review shows that women with endometriosis experience high levels of depression and anxiety, indicating that the psychological toll of the disease remains high. The high prevalence of these mental health conditions should be attributed to the pain and uncertainty the patients experienced as well as the burden of the disease on their overall functioning.
Pain was identified as an important factor that affected mental health. It was confirmed that severe pelvic pain, dysmenorrhea, and chronic pain were associated with depressive and anxious symptoms [22]. Chronic pain not only impacts physical performance but also leads to emotional fatigue, decreased ability to cope with stress, and increased risk of psychological distress. This finding supports the biopsychosocial model of pain, which holds that pain is not only a physical phenomenon, but its perception and experience are influenced by biological, psychological, and social factors. An observational case-control study included 344 patients with endometriosis and found that among them, 119 patients had mental disorders and 70 patients had depression. Patients with depression (EM-D) or mental state (EM-P) dyspareunia and dyschezia occurred more frequently. A total of 27,840 women from six European countries were included in the study by Becker et al. (2021) [27]. The most common symptoms related to endometriosis are dysmenorrhea (61.8%), massive/irregular bleeding (50.8%), and pelvic pain (37.2%). Women reported that endometriosis affected their emotions; 55.6% of people felt “frustrated”, depressed or desperate, and 53.2% felt defeated or disappointed with their family/friends [28]. These research results are consistent with the conclusion of this study. Endometriosis can cause both physical pain and mental distress for patients. Medical staff and society should pay attention to the mental condition of patients with endometriosis. From January 2019 to March 2020, 104 women were included in a prospective observational study, and their anxiety levels decreased after assessment (STAI-Y6 60.0 ±15.0 vs. 40.8 ±14.2). Patients with a higher baseline anxiety level (test. change –24.3; 95% confidence interval: –29.2 to –19.5) experienced a decrease in anxiety level after the physical examination [29, 30].
Diagnostic delays and psychological implications
One of the significant trends identified in the reviewed research is the psychological impact of diagnostic delays. Endometriosis is often diagnosed only after years of enduring symptoms, during which time women may experience chronic pain, mistreatment, and a lack of acknowledgment from healthcare providers. This protracted diagnostic journey, characterized by frustration and uncertainty, can exacerbate emotional distress [23]. The fact that a shorter time from the diagnosis is related to increased anxiety also points to the difficulties that women experience in dealing with the first stage of accepting an illness that is chronic and cannot be cured.
The diagnostic delay carries significant social and cultural implications. The tendency to postpone or avoid seeking care, coupled with the stigma surrounding menstrual and pelvic pain, contributes to these delays, leaving many women feeling isolated and unheard. Addressing these systemic issues requires enhanced education for both medical professionals and the public, as well as improved diagnostic practices aimed at identifying endometriosis more promptly and accurately.
Individual characteristics and protective factors
In addition to the physical and diagnostic approaches to endometriosis, this article explores the influence of personality traits on mental health. Higher self-esteem, enhanced emotional self-efficacy, and supportive intimate relationships are associated with improved psychological outcomes [23, 24]. These findings have significant implications for endometriosis, indicating that individual resilience and social support can prevent a significant amount of the mental health burden. Women with higher disease centrality are more likely to report depressive symptoms and lower levels of life satisfaction [24]. On the other hand, the narratives of control are related to improved mental health, implying that the interventions designed to alter the narrative might be beneficial.
Psychiatric comorbidities and long-term risks
The significant association between endometriosis and depression found in this review provokes questions regarding the common mechanisms of pathogenesis. Women with endometriosis were at a higher risk of developing depressive and anxiety than those without the disease, and the women who already had depression and anxiety had a higher likelihood of developing endometriosis [21]. Some of these mechanisms include inflammation, hormonal changes, and hypothalamic-pituitary-adrenal axis abnormalities, which need to be explored in future studies.
Furthermore, the increased odds of self-harmed/suicide and all-cause mortality supported the potentially lethal consequences of untreated psychological symptoms in women with endometriosis [25, 26]. These results underscore the need to include mental health assessment and treatment as part of standard care for individuals with endometriosis.
Implications for clinical practice
The outcomes of this review also have important implications for the medical treatment of endometriosis. First, there is a need for mental health interventions to be incorporated into the treatment of endometriosis. Depression, anxiety, and other psychological symptoms should be screened as part of routine practice, and patients should be guided on where to access psychological support. Second, the management of pain should be comprehensive, encompassing not only a physical perception of pain, but also psychological and emotional. Other methods may include cognitive behavioral therapy, mindfulness practices, and narrative therapy to support medical and surgical management.
Third, this systematic review on the mental health burden of endometriosis has implications for training of healthcare providers. The nature of the disease requires that the providers acknowledge the psychosocial aspects of the illness and manage to reassure patients about their feelings. Finally, patient education and involvement should be prioritized. Women should be empowered with resources that will improve their self-esteem, emotional self-efficacy, and coping mechanisms to improve their mental health.
Heterogeneity analysis
The sample size of the included literature was in line with the efficacy analysis. The results of the one-by-one elimination analysis to test the heterogeneity of this study showed that after all the included studies were eliminated one by one, the confidence interval and total RR were still within the fluctuation range calculated by the forest plot, indicating that the bias of all the included studies was controllable and stable. The L ‘Abbe plot was used to conduct heterogeneity analysis on binary variables. Basically, all the included studies showed a linear relationship, and the research results were basically homogeneous, which was of certain significance. The results of the meta-regression analysis indicated that the included literature could already yield meaningful results and there was no need for subgroup analysis. Heterogeneity analysis indicates that there was a certain degree of heterogeneity in this study, but the analysis results were still significant.
Strengths, limitations, and future directions
One of the major strengths of this review is the broad coverage of the studies, originating from various geographic and cultural backgrounds, which increases the external validity of the findings. Furthermore, the application of standardized assessment instruments throughout the studies enhances the credibility of the documented results.
However, there were also some limitations. Many publications were horizontal, which means it was difficult to establish a causal relationship between endometriosis and mental health. More longitudinal studies are needed to conduct longitudinal investigations into this relationship, with a focus on diagnosing the consequences of delays and the outcomes of intervention measures. Furthermore, the variability of research types, participants, and measured mental health impacts complicated the analysis and comparison. Only 9 studies were included in this analysis. The number was too small, which leads to certain heterogeneity in the meta-analysis, and the results lacked certain persuasiveness. In future research, we will search as many databases as possible and include as many studies as possible in the meta-analysis. Additionally, we will extend our search to Embase, Scopus, and gray literature to minimize publication bias and improve the completeness of evidence. Meanwhile, we will also conduct subgroup analyses on the research design of the included literature, the family economic income of patients with endometriosis, marital status, etc., so that the obtained results are meaningful for the actual treatment. It is also necessary to consider how other aspects such as race, economic status, and cultural customs affect endometriosis and its treatment. Exploring the connection between endometriosis and depression/anxiety is helpful for formulating intervention and treatment plans.
In conclusion, this systematic review focuses on the high mental health cost that has been reported among women with endometriosis, with increased depression, anxiety, and psychological distress recorded. Many factors were found to be associated with these outcomes. They included pain severity, diagnostic delay, and presence of comorbid conditions. In the same vein, self-esteem, emotional self-efficacy, and social support were revealed as moderators that could buffer the effects of the disease.
These conclusions stress the necessity for an interdisciplinary approach to the treatment of endometriosis, in which the evaluation and treatment of mental health issues should be included in addition to pain relief and pharmacological treatment. The study highlighted that early diagnosis and effective care management models for endometriosis are vital to enhance both somatic and psychiatric recovery for affected females. Future studies should aim to identify the long-term outcomes of these interventions and the underlying common pathways between endometriosis and depression and anxiety. As highlighted in this review, various interrelated factors need to be addressed with a view to improving the quality of life of millions of affected women.