Introduction
Peripheral artery disease (PAD) is associated with significant morbidity, mortality and quality of life impairment [1−3]. The ankle-brachial index (ABI) is a noninvasive, safe, simple and quick to perform test for lower extremity PAD [2, 4]. The critical evidence gaps and future research directions for PAD-related research include advancement in diagnostics, and technologies for highly accurate measurement of ABI [1].
The ABI is the ratio of the systolic blood pressure (SBP) measured at the ankle to that measured at the brachial artery [5, 6]. In a clinical setting, many factors influence the ABI measurements, including method of measurement, repeated measures, as well as demographic parameters including height, gender, race or heart rate [7]. Especially in patients with atrial fibrillation (AF), the ABI may be potentially more difficult because of high beat-to-beat variability of heart rate and stroke volume [8]. Our previous study showed that AF does not significantly affect ABI measured by the Doppler method [9]. However, there is still a lack of data indicating whether the automatic oscillometric method, often used for ABI measurements, is also accurate in AF patients. A meta-analysis of 24 studies assessing the usefulness of automated oscillometric devices for ABI estimation, when compared with the Doppler method, showed that the oscillometric method may be a useful alternative to the Doppler method in patients without atrial fibrillation [10]. Atrial fibrillation does not significantly affect the accuracy of oscillometric blood pressure measurements when three repeated measurements are performed [11]. However, these findings were questioned because of specific validation criteria [12]. Hence, the answer as to how AF affects the oscillometric blood pressure and ABI measurements remains not fully known.
Therefore, the purpose of this study was to investigate whether atrial fibrillation influences results of ABI measurements performed with an automatic oscillometric device.
Material and methods
Study design
In this study, we included data from one hundred and fifteen consecutive patients with atrial fibrillation admitted for electrical cardioversion (EC). The current study is the extension of the research published by Dabrowski et al. [9], where detailed patients’ characteristics were presented. Ninety-nine patients (mean age: 66.6 ±11) years, M/F − 63/36) underwent the complete study protocol and were analyzed (Figure 1).
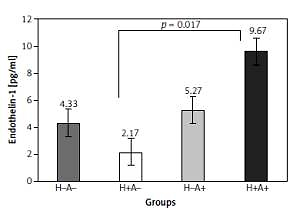
Figure 1
STARD (Standards for Reporting of Diagnostic Accuracy) flowchart representing the selection of the study patients
The inclusion criteria for participation in the study were age 18−70 years and clinical decision of patients’ eligibility for electrical cardioversion (EC) of atrial fibrillation. The exclusion criteria were circulatory instability, use of vasoconstrictive agents, limb trauma or upper limb artery stenosis.
The local bioethical committee accepted the study and informed consent was obtained from all participants. This trial is registered at ClinicalTrials.gov (NCT02986282).
ABI was performed in two study sessions, before and after EC. The first session was scheduled before routine anesthesia for EC (with intravenous propofol 1%). The second session started approximately 1 h after EC, in the same intensive care unit, with the patient fully conscious. All study-related procedures were finished within 2 h after EC. No adverse events were observed during the study-related procedures in the intensive care unit.
ABI measurements
All the measurements were taken in the intensive care unit at an ambient room temperature of about 21°C, after patients gave their written informed consent to participate in the study. All patients were awake, fasting and in the supine position. The ankle-brachial index was measured according to the guidelines issued by AHA [7]. Firstly, Doppler ABI measurements were performed. Systolic blood pressure (SBP) was measured using a Doppler device (Echo Sounder ES-101EX, Hadeco, Kawasaki, Japan) and a validated and calibrated aneroid sphygmomanometer (Minimus II, Riester, Jungingen, Germany). For each measurement, the appropriate cuff size was used, with the cuff width measuring at least 40% of the limb circumference. The higher value of SBP measured on the arm and the higher value of SBP measured on the posterior tibial or dorsalis pedis artery were used to calculate the ABI. During both study sessions throughout the study, the ABI measurements were repeated 3 times in an alternating clockwise sequence. The clockwise sequence was as follows: right arm, right posterior tibial, right dorsalis pedis, left posterior tibial, left dorsalis pedis, left arm, right arm. The counterclockwise sequence started with the left arm, with each successive set of measurements taken in the reverse order. The same sequence of limb pressure measurements was used during the whole study. The measurements were repeated three times, and the mean of the results was used for calculations. After Doppler measurements, the WatchBP Office ABI system (MicroLife WatchBP AG, Windau, Switzerland) was used for three measurements on both lower extremities. The mean of three ABI measurements was used for further calculations. The ABI system included two sizes of arm cuffs and ankle cuff. All automated oscillometric recordings and Doppler measurements were performed using appropriately sized cuffs. One investigator (M.D.), trained in vascular procedures, performed all ABI measurements.
Endpoints
The primary endpoint of this study was the difference between ABI measures before and after electrical cardioversion using the oscillometric method, and additionally the difference between measurements performed with the Doppler method and the oscillometric method.
Statistical analysis
A sample size calculation was made for the initial study and presented in our previous publication [9]. Each lower extremity measurement was considered as a separate test; therefore, 198 measurements were repeated 3 times using both the Doppler and the oscillometric method. The data were processed with the Shapiro-Wilk normality test. The ABI measurements were compared using the Wilcoxon signed rank test. The comparison was calculated for patients with sinus rhythm and during atrial fibrillation, as well as for measures with the two studied methods. For normal data distributions, the paired two-tailed t test was used. The Bland-Altman plot was used to analyze the agreement between ABI measurements performed in sinus rhythm with an oscillometric device (considered the method tested in standard conditions) and ABI measurements performed during atrial fibrillation (method tested in experimental conditions). The Bland and Altman plot was also used to analyze the agreement between the ABI measured by the reference Doppler method and the ABI measured by the oscillometric device in experimental conditions. Correlations between ABI measurements in sinus rhythm and after EC using the oscillometric method were performed. Also, the correlation between both methods of ABI and the Spearman’s rho coefficient were estimated. Statistical significance was established at p < 0.05. All data were calculated using statistical software R 3.1.3 and were expressed as median (IQR) and mean (SD) as appropriate.
Results
Using the reference Doppler method we investigated in total 198 lower extremities in 99 patients referred for EC. The diagnosis of PAD, as defined by ABI ≤ 0.9, was established in 3 patients (ABI ≤ 0.9 was detected on 4 lower extremities). The automated oscillometric method detected 2 patients with PAD (two lower extremities with ABI ≤ 0.9; Figure 1) in sinus rhythm and 1 during atrial fibrillation (one lower extremity). Eight borderline PAD (ABI in the range of 0.91−1.0) were identified by the Doppler method and 10 using the oscillometric method.
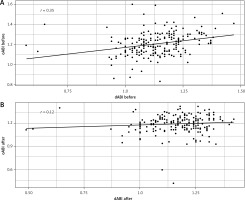
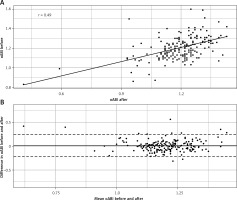
The median ABI measurement with the oscillometric method, performed on both lower limbs before EC, did not differ from ABI after restoration to sinus rhythm (1.21 (1.13−1.27) before EC vs. 1.22 (1.14−1.26) after EC, p = 0.664, respectively) (Figure 2). A correlation was found between measurements performed with the oscillometric method before and after EC on both lower limbs (r = 0.49, p < 0.001) (Figure 3). The Bland-Altman plot was performed, using the measurement after EC as the reference. The average bias was low 0.009 (95% limits of agreement – 0.22 and 0.24); however, more than 5% of differences were beyond the limits of agreement, suggesting poor agreement between measurements performed with the oscillometric method before and after cardioversion (Figure 3).
Figure 2
Plot showing differences in median ankle-brachial index (ABI) before and after EC assessed using Doppler and oscillometric method respectively – dABI before, dABI after, oABI before and oABI after, # p < 0.001. The dots indicate outliers that are more than 3/2 of the upper quartile, and the whiskers indicate maximum and minimum excluding outliers, the box margins show upper (75%) and lower quartile (25%), and the central line represents the median
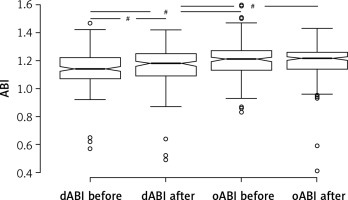
Figure 3
Correlation between ankle-brachial index (ABI) oscillometric method results obtained before and after EC (oABI before vs. oABI after, r = 0.49, p < 0.001) (A) and Bland-Altman plot between ABI measurements performed before and after EC using oscillometric method (B)
When compared with the Doppler measurements, the oscillometric measurements were significantly higher both during AF (1.21 (1.13−1.27) vs. 1.14 (1.07−1.22), p < 0.001 respectively) and in sinus rhythm (1.22 (1.14−1.26) vs. 1.18 (1.09−1.13), p < 0.001 respectively; Figure 2). Upper 95% CI margins for the median of difference in ABI between methods were 0.08 and 0.06 for the results obtained before and after cardioversion. The difference was higher during AF than during sinus rhythm. That may be significant from a clinical perspective (0.07 vs. 0.04, p = 0.002).
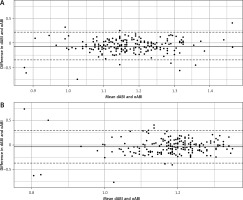
The two methods showed a weak correlation before EC (r = 0.35, p < 0.001), but after EC there was no correlation between the methods (r = 0.12, p = 0.07; Figure 4). The Bland-Altman plot showed no significant agreement between measurements performed using the oscillometric method and the Doppler method in sinus rhythm and during AF (Figure 5). The average bias before EC was 0.068 (95% limits of agreement −0.21 and 0.35) and after EC was 0.035 (95% limits of agreement −0.30 and 0.37).
Discussion
Guidelines for PAD recommends the ABI as a strong, class 1 recommendation, of moderate-quality evidence as a diagnostic test in patients with history or physical examination findings suggestive of PAD [1, 2]. This test is also important for follow-up and periodic evaluation in patients with PAD who have undergone lower extremity revascularization. A change in ABI of 0.15 is considered clinically significant [1, 13].
Arrhythmias, especially atrial fibrillation, are common in the aging population [14]. Unfortunately, atrial fibrillation is often undiagnosed. Atrial fibrillation may substantially influence blood pressure measurements. Previously, we found that the results of ABI measured using the Doppler method during atrial fibrillation corresponded with the results obtained in sinus rhythm [9].
The main finding of the present study is that ABI results obtained using the automated oscillometric method did not differ when measured in sinus rhythm and during atrial fibrillation. The lack of difference between results obtained using the oscillometric method before and after EC does not mean however that the use of the oscillometric method should be preferred for ABI determination in all groups of patients. Previously it was suggested that PAD screening with the oscillometric device may not be suitable in patients with atrial fibrillation [10].
The second important finding of the study is that results of measurements performed using oscillometric and Doppler methods differed from each other. The difference was greater during atrial fibrillation than in sinus rhythm. This is an important observation from the clinical perspective, because it may impact the potential usefulness of automatic oscillometric ABI determination in patients with atrial fibrillation. We observed a weak correlation between the two methods during arrhythmia and no correlation in sinus rhythm, which is in contrast with some other reports [10]. However, the Bland-Altman analysis also showed low agreement of both methods (Figure 5), both during atrial fibrillation and in sinus rhythm, when the Doppler method was considered as the reference. In addition to bias higher than reported by other authors [15], we observed wide limits of agreement, and almost 5% differences passing the 95% limit of agreement.
Analyzing the ABI results obtained using the oscillometric method, it is important to realize that the automated method does not measure systolic and diastolic blood pressure directly. The values of systolic and diastolic blood pressure are calculated from the mean blood pressure by the oscillometric device, according to its algorithm. This may cause significant bias, especially during arrhythmia. Because of beat-by-beat changes in pulse pressure and mean pressure, there may be a distortion in the relation between cuff pressure and oscillometric wave amplitude. Considering that ABI is the ratio between blood pressures, the difference between different measurements may be amplified.
In the medical literature, there is a paucity of information about the ABI measurements in patients with AF. MacDougall et al. showed that the oscillometric method of PAD detection was feasible and operator-independent, even though it did not detect low ABI as efficiently as the Doppler method, especially in subjects with non-palpable peripheral pulses [16]. Hsu et al. found that in patients with AF values of ABI were lower than in subjects with sinus rhythm. After adjustment for heart rate this relation disappeared, which suggests that heart rate can significantly influence the relationship between AF and ABI. In the current study, we performed an analysis, dividing studied group into the patients with heart rate (HR) over 100 beats/minute and patients with HR below 100 beats/minute. This approach did not affect differences between results obtained before and after EC and the differences between methods.
In contrast to our study, another work by Pagonas et al. [11] found that the biases of systolic and diastolic blood pressure did not significantly differ in the presence or absence of atrial fibrillation, when the Bland-Altman analysis was used for analysis. However, the difference in the results between these two studies may stem from the fact that the authors measured blood pressure, but they did not measure ABI, and that difference impacts the results and any comparisons between these studies. Furthermore, our study analyzed exactly the same patients – before and after EC. That was not the case in the study of Pagonas et al. [11], who analyzed two different populations of patients – with and without atrial fibrillation.
In the current study values of oscillometric measurements were higher than Doppler measurement results. As summarized by Veckber et al., other studies also found higher oscillometric ABI values than the Doppler ABI values. Though from the pathophysiological point of view such a difference should not be present or be opposite, it is probably related to the intrinsic characteristics of each method. Other authors postulated that higher (close to 1) cutoff values for PAD detection should be used using the oscillometric method [17, 18].
Automated devices, especially with the AF detection mode, due to easy use are handy tools for PAD and possible AF screening. Because of the impact on AF detection automated oscillometric devices may strengthen the appropriate use of the reference Doppler method in case of AF recognition.
The main limitation of the study is that a possible effect of conditions related to the procedure of electrical cardioversion, including effects of anesthesia, cannot be excluded. However, the ABI measurements were performed at the time when propofol should not have direct hemodynamic effects. Furthermore, we designed this research to study in detail the impact of AF on ABI. Therefore, we excluded the hemodynamic effects of the medications that are often prescribed after EC, especially the antiarrhythmic and the heart rate slowing drugs.
The current study identified only a few patients with PAD according to the ABI results < 0.9, detected by both investigated methods. The oscillometric method is considered as relatively observer-independent, and this study included consecutive patients admitted for EC without prescreening. If the threshold of ABI < 1.0 to diagnose PAD was used, as suggested by other authors evaluating the oscillometric method [17, 18], number of PAD detected would be considerably larger. It worth noting that using the threshold of ABI < 1.0, numbers of PAD cases detected in the study would be identical using both methods.
In conclusion, postulate that the automated oscillometric method should not replace the reference Doppler method in patients with atrial fibrillation. However, more research related to the oscillometric measurements is needed in subjects with PAD and AF.