Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
DIET / RESEARCH PAPER
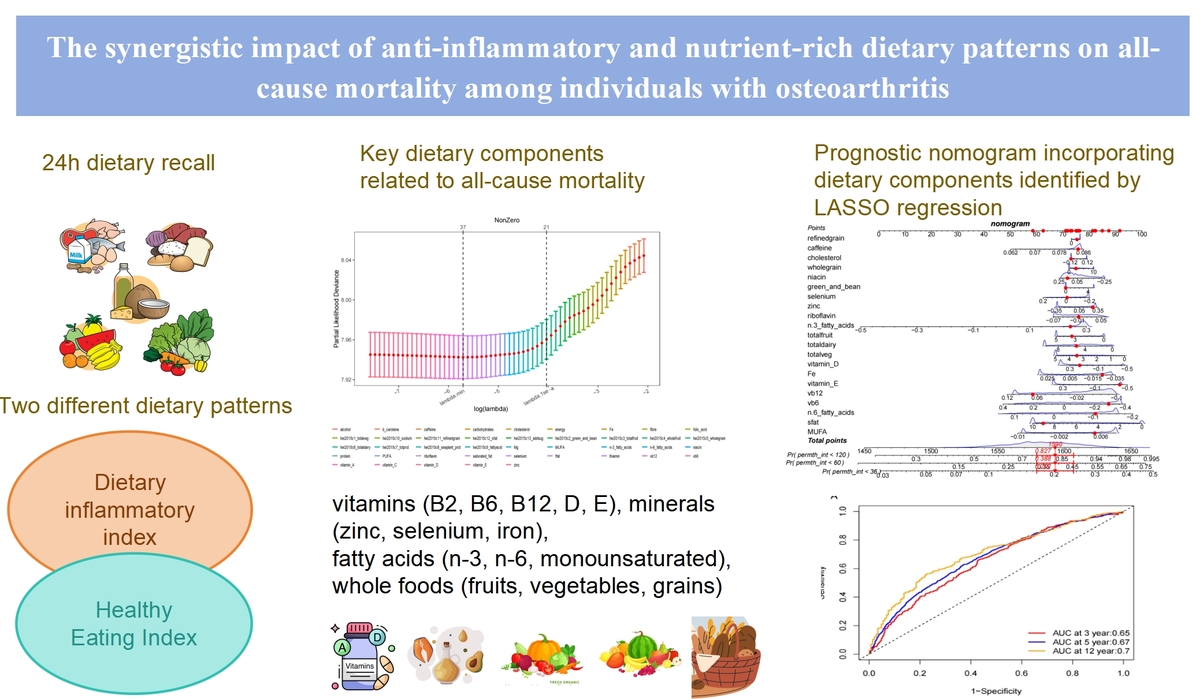
The synergistic impact of anti-inflammatory and nutrient-rich dietary patterns on long term prognosis among individuals with osteoarthritis
1
Chengdu Fifth People's Hospital, China
2
Chengdu Medical College, China
3
Deyang People’s Hospital, China
These authors had equal contribution to this work
Submission date: 2025-07-27
Final revision date: 2025-08-17
Acceptance date: 2025-09-08
Online publication date: 2026-02-08
KEYWORDS
TOPICS
ABSTRACT
Introduction:
To investigate the associations between healthy and anti-inflammatory dietary patterns and mortality risk in osteoarthritis (OA) patients, and to identify key dietary factors influencing long-term outcomes.
Material and methods:
We analyzed data from 3,012 OA patients participating in the National Health and Nutrition Examination Survey (NHANES) between 2007 and 2018. Dietary patterns were assessed using two validated indices: the Healthy Eating Index-2015 (HEI-2015) for overall diet quality and the Dietary Inflammatory Index (DII) for inflammatory potential, both derived from 24-hour dietary recall data. Mortality outcomes were ascertained through linkage with the National Death Index. Weighted Cox proportional hazards regression models were employed to evaluate associations between dietary patterns and all-cause mortality, with adjustments for demographic, lifestyle, and clinical confounders. To identify key dietary predictors, we applied Least Absolute Shrinkage and Selection Operator (LASSO) regression. A prognostic nomogram was developed to assess predictive performance.
Results:
A healthy, anti-inflammatory diet (high HEI-2015, low DII) was associated with a 14% lower mortality risk (HR: 0.86, 95% CI: 0.75–1.00, p-trend = 0.045) compared to an unhealthy, pro-inflammatory diet. LASSO regression highlighted 21 key dietary factors, including vitamins (B2, B6, B12, D, E), minerals (zinc, selenium, iron), fatty acids (n-3, n-6, monounsaturated), and whole foods (fruits, vegetables, grains). The nomogram showed reliable predictive accuracy (AUC: 0.65 at 3 years, 0.70 at 12 years). Subgroup analyses indicated stronger effects in non-smokers (HR: 0.79, 95% CI: 0.65–0.97).
Conclusions:
Adopting a healthy, anti-inflammatory dietary pattern can reduce mortality rates in individuals with arthritis, with specific micronutrients and food groups playing a critical role.
To investigate the associations between healthy and anti-inflammatory dietary patterns and mortality risk in osteoarthritis (OA) patients, and to identify key dietary factors influencing long-term outcomes.
Material and methods:
We analyzed data from 3,012 OA patients participating in the National Health and Nutrition Examination Survey (NHANES) between 2007 and 2018. Dietary patterns were assessed using two validated indices: the Healthy Eating Index-2015 (HEI-2015) for overall diet quality and the Dietary Inflammatory Index (DII) for inflammatory potential, both derived from 24-hour dietary recall data. Mortality outcomes were ascertained through linkage with the National Death Index. Weighted Cox proportional hazards regression models were employed to evaluate associations between dietary patterns and all-cause mortality, with adjustments for demographic, lifestyle, and clinical confounders. To identify key dietary predictors, we applied Least Absolute Shrinkage and Selection Operator (LASSO) regression. A prognostic nomogram was developed to assess predictive performance.
Results:
A healthy, anti-inflammatory diet (high HEI-2015, low DII) was associated with a 14% lower mortality risk (HR: 0.86, 95% CI: 0.75–1.00, p-trend = 0.045) compared to an unhealthy, pro-inflammatory diet. LASSO regression highlighted 21 key dietary factors, including vitamins (B2, B6, B12, D, E), minerals (zinc, selenium, iron), fatty acids (n-3, n-6, monounsaturated), and whole foods (fruits, vegetables, grains). The nomogram showed reliable predictive accuracy (AUC: 0.65 at 3 years, 0.70 at 12 years). Subgroup analyses indicated stronger effects in non-smokers (HR: 0.79, 95% CI: 0.65–0.97).
Conclusions:
Adopting a healthy, anti-inflammatory dietary pattern can reduce mortality rates in individuals with arthritis, with specific micronutrients and food groups playing a critical role.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.