Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
NEPHROLOGY / RESEARCH PAPER
Exploring causality between peripheral blood B cell subtypes and membranous nephropathy: A two-sample Mendelian randomization study
1
Department of Nephrology, The Sixth Medical Center of PLA General Hospital, China
These authors had equal contribution to this work
Submission date: 2025-01-03
Final revision date: 2025-04-23
Acceptance date: 2025-05-14
Online publication date: 2025-06-24
Corresponding author
Zhiyong Zhang
Department of nephrology, The sixth Medical Center of PLA General Hospital, Beijing, China
Department of nephrology, The sixth Medical Center of PLA General Hospital, Beijing, China
KEYWORDS
TOPICS
ABSTRACT
Introduction:
Membranous nephropathy (MN) is a glomerular autoimmune disease associated with nephrotic syndrome. This study explored the influence of peripheral blood B cell subtypes on MN using Mendelian randomization (MR).
Material and methods:
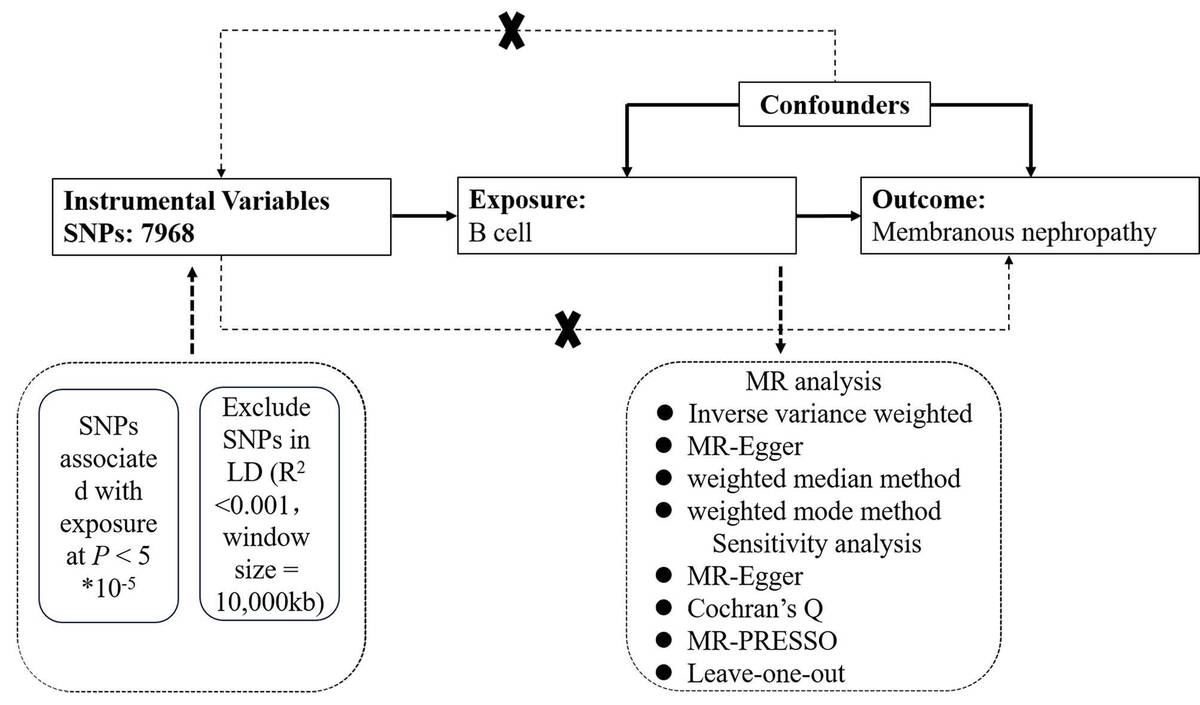
Data on single-nucleotide polymorphisms (SNPs) associated with peripheral blood B cells and MN were obtained from a genome-wide association study (GWAS). Analytical methods included instrumental variable weighted (IVW), weighted median, weighted mode methods, and MR-Egger regression. Sensitivity analyses were conducted using MR-Egger, Mendelian Randomization Pleiotropy RESidual Sum and Outlier (MR-PRESSO) for outlier detection, Cochran’s Q test for heterogeneity, and leave-one-out analysis to assess the robustness of the findings.
Results:
Higher levels of IgD+ CD24-B cell absolute count (OR 0.8285, 95% CI 0.7317-0.9381, P=0.003), B-cell activating factor receptor (BAFF-R) on IgD+ CD24-B cells (OR 0.9045, 95% CI 0.8275-0.9886, P=0.0269), BAFF-R on IgD+ CD38dim B cells (OR 0.9057, 95% CI 0.8277-0.991, P=0.0311), BAFF-R on IgD- CD27-B cells (OR 0.9134, 95% CI 0.8404-0.9928, P=0.0332), CD19 on IgD-CD24-B cells (OR 0.884, 95% CI 0.7906-0.9886, P=0.0306), CD24 on switched memory B cells (OR 0.8927, 95% CI 0.8133-0.9798, P=0.0169), and CD25 on switched memory B cells (OR 0.8768, 95% CI 0.7745-0.9927, P=0.0379) were strongly associated with an decreased risk of membranous nephropathy. Sensitivity analyses were conducted to confirm the stability of the findings.
Conclusions:
This MR study supports the possibility of a genetic causal association between peripheral blood B cell subtypes and MN. The results enhance the comprehension of the immunological basis of MN and may play a role in personalized medicine.
Membranous nephropathy (MN) is a glomerular autoimmune disease associated with nephrotic syndrome. This study explored the influence of peripheral blood B cell subtypes on MN using Mendelian randomization (MR).
Material and methods:
Data on single-nucleotide polymorphisms (SNPs) associated with peripheral blood B cells and MN were obtained from a genome-wide association study (GWAS). Analytical methods included instrumental variable weighted (IVW), weighted median, weighted mode methods, and MR-Egger regression. Sensitivity analyses were conducted using MR-Egger, Mendelian Randomization Pleiotropy RESidual Sum and Outlier (MR-PRESSO) for outlier detection, Cochran’s Q test for heterogeneity, and leave-one-out analysis to assess the robustness of the findings.
Results:
Higher levels of IgD+ CD24-B cell absolute count (OR 0.8285, 95% CI 0.7317-0.9381, P=0.003), B-cell activating factor receptor (BAFF-R) on IgD+ CD24-B cells (OR 0.9045, 95% CI 0.8275-0.9886, P=0.0269), BAFF-R on IgD+ CD38dim B cells (OR 0.9057, 95% CI 0.8277-0.991, P=0.0311), BAFF-R on IgD- CD27-B cells (OR 0.9134, 95% CI 0.8404-0.9928, P=0.0332), CD19 on IgD-CD24-B cells (OR 0.884, 95% CI 0.7906-0.9886, P=0.0306), CD24 on switched memory B cells (OR 0.8927, 95% CI 0.8133-0.9798, P=0.0169), and CD25 on switched memory B cells (OR 0.8768, 95% CI 0.7745-0.9927, P=0.0379) were strongly associated with an decreased risk of membranous nephropathy. Sensitivity analyses were conducted to confirm the stability of the findings.
Conclusions:
This MR study supports the possibility of a genetic causal association between peripheral blood B cell subtypes and MN. The results enhance the comprehension of the immunological basis of MN and may play a role in personalized medicine.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.