Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
CLINICAL RESEARCH
Machine learning prediction of early hypothermia in sepsis patients
1
Hangzhou Normal University Affiliated Hospital Zhejiang University School of Medicine Second Affiliated Hospital, China
2
Hangzhou Normal University Affiliated Hospital, China
3
The Third People’s Hospital of Deqing, China
Submission date: 2025-06-03
Final revision date: 2025-08-06
Acceptance date: 2025-08-17
Online publication date: 2025-10-29
KEYWORDS
TOPICS
ABSTRACT
Introduction:
Sepsis is a systemic inflammatory response syndrome caused by infection and remains a leading cause of mortality worldwide. Abnormal body temperature, especially hypothermia (body temperature < 36°C), is a key clinical feature in sepsis patients and is closely associated with disease severity, impaired immune function, and poor prognosis. Early prediction of hypothermia is crucial for timely intervention and improving prognosis.
Material and methods:
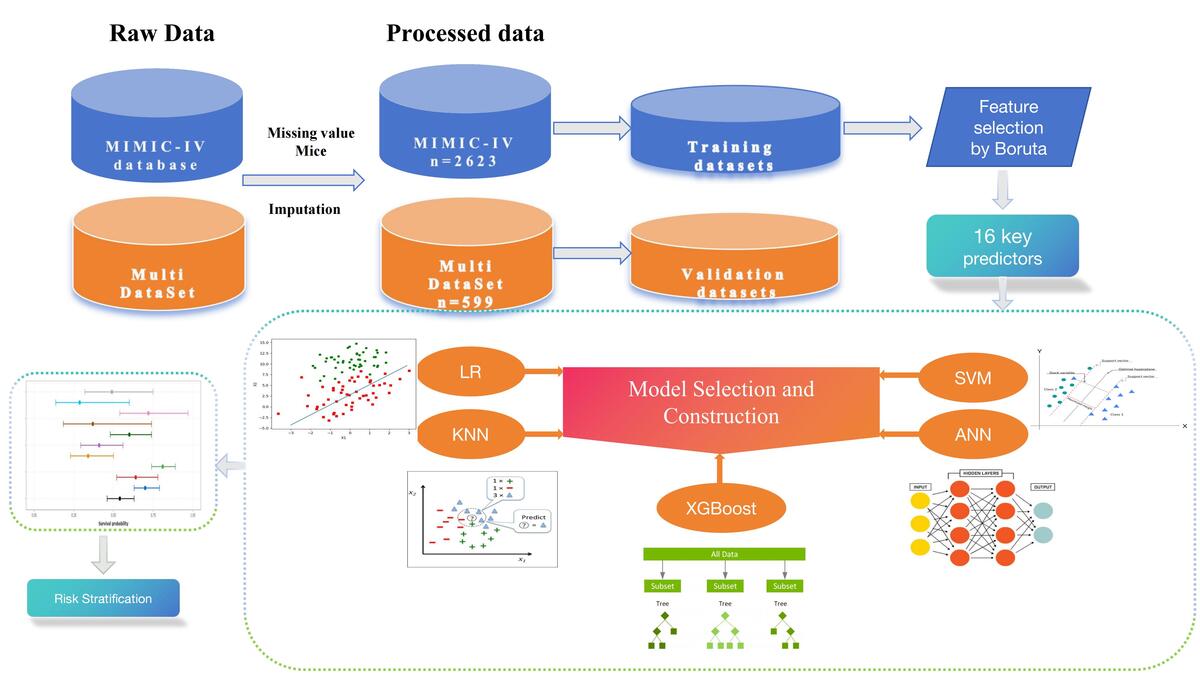
This study used machine learning algorithms to train and validate a prediction model for early temperature changes in critically ill sepsis patients. Data were extracted from the MIMIC-IV database and five models were established: XGBoost, LR, SVM, KNN, and ANN.
Results:
The XGBoost model demonstrated the best predictive performance with AUC values of 0.92 in the training cohort and 0.98 in the validation cohort.
Conclusions:
This model can assist clinicians in identifying sepsis patients at high risk for early hypothermia and implementing early intervention to reduce mortality.
Sepsis is a systemic inflammatory response syndrome caused by infection and remains a leading cause of mortality worldwide. Abnormal body temperature, especially hypothermia (body temperature < 36°C), is a key clinical feature in sepsis patients and is closely associated with disease severity, impaired immune function, and poor prognosis. Early prediction of hypothermia is crucial for timely intervention and improving prognosis.
Material and methods:
This study used machine learning algorithms to train and validate a prediction model for early temperature changes in critically ill sepsis patients. Data were extracted from the MIMIC-IV database and five models were established: XGBoost, LR, SVM, KNN, and ANN.
Results:
The XGBoost model demonstrated the best predictive performance with AUC values of 0.92 in the training cohort and 0.98 in the validation cohort.
Conclusions:
This model can assist clinicians in identifying sepsis patients at high risk for early hypothermia and implementing early intervention to reduce mortality.
REFERENCES (39)
1.
Singer M, Deutschman CS, Seymour CW, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016; 315: 801-10.
2.
Hotchkiss RS, Moldawer LL, Opal SM, et al. Sepsis and septic shock. Nat Rev Dis Primers 2016; 2: 16045.
3.
Machado FR, Cavalcanti AB, Bozza FA, et al. The epidemiology of sepsis in Brazilian intensive care units (the Sepsis PREvalence Assessment Database, SPREAD): an observational study. Lancet Infect Dis 2017; 17: 1180-9.
4.
Annane D. Body temperature in sepsis: a hot topic. Lancet Respir Med 2018; 6: 162-3.
5.
Kushimoto S, Gando S, Daizoh Saitoh D, et al. The impact of body temperature abnormalities on the disease severity and outcome in patients with severe sepsis: an analysis from a multicenter, prospective survey of severe sepsis. Crit Care 2013; 17: R271.
6.
Liu D, Huang SY, Sun JH, et al. Sepsis-induced immunosuppression: mechanisms, diagnosis and current treatment options. Mil Med Res 2022; 9: 56.
7.
Ito Y, Kudo D, Kushimoto S. Association between low body temperature on admission and in-hospital mortality according to body mass index categories of patients with sepsis. Medicine 2022; 101: e31657.
8.
Vincent J, de Mendonca A, Cantraine F, et al. Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Crit Care Med 1998; 26: 1793-800.
9.
Thakur R, Naga Rohith V, Arora JK. Mean SOFA score in comparison with APACHE II score in predicting mortality in surgical patients with sepsis. Cureus J Med Sci 2023; 15: e36653.
10.
Huang Y, JIang S, Li W, et al. Establishment and effectiveness evaluation of a scoring system-RAAS (RDW, AGE, APACHE II, SOFA) for sepsis by a retrospective analysis. J Inflamm Res 2022; 15: 465-74.
11.
Sonna LA, Hawkins L, Lissauer ME, et al. Core temperature correlates with expression of selected stress and immunomodulatory genes in febrile patients with sepsis and noninfectious SIRS. Cell Stress Chaperones 2010; 15: 55-66.
12.
Handelman GS, Kok HK, Chandra RV, et al. eDoctor: machine learning and the future of medicine. J Intern Med 2018; 284: 603-19.
14.
Toh TS, Dondelinger F, Wang D. Looking beyond the hype: applied AI and machine learning in translational medicine. Ebiomedicine 2019; 47: 607-15.
15.
Johnson AEW, Bulgarelli L, Shen L, et al. MIMIC-IV, a freely accessible electronic health record dataset. Sci Data 2023; 10: 1.
16.
Speiser JL, Miller ME, Tooze J, Ip E. A comparison of random forest variable selection methods for classification prediction modeling. Expert Syst Appl 2019; 134: 93-101.
17.
Lee BH, Inui D, Suh GY, et al. Association of body temperature and antipyretic treatments with mortality of critically ill patients with and without sepsis: multi-centered prospective observational study. Crit Care 2012; 16: R33.
18.
Peres Bota D, Lopes Ferreira F, Lot CM, Vincent JL. Body temperature alterations in the critically ill. Intens Care Med 2004; 30: 811-6.
19.
Wiewel MA, Harmon MB, van Vught LA, et al. Risk factors, host response and outcome of hypothermic sepsis. Crit Care 2016; 20: 328.
20.
Laupland KB, Zahar JR, Adrie C, et al. Determinants of temperature abnormalities and influence on outcome of critical illness. Crit Care Med 2012; 40: 145-51.
21.
Young PJ, Bellomo R. Fever in sepsis: is it cool to be hot? Crit Care 2014; 18: 109.
22.
Carrara M, Ferrario M, Bollen Pinto B, Herpain A. The autonomic nervous system in septic shock and its role as a future therapeutic target: a narrative review. Ann Intensive Care 2021; 11: 80.
23.
Leibovici L, Gafter-Gvili A, Paul M, et al. Relative tachycardia in patients with sepsis: an independent risk factor for mortality. QJM-Int J Med 2007; 100: 629-34.
24.
Ning Y, Li WJ, Lu X, et al. Association between heart rate and mortality in patients with septic shock: an analysis revealed by time series data. BMC Infect Dis 2024; 24: 1088.
25.
Broccard A. Prone position, high-frequency oscillatory ventilation, and Hippocrates in acute respiratory distress syndrome. Crit Care Med 2005; 33: 2407-8.
26.
Ahmad S, Beckett M. Recovery from pH 6.38: lactic acidosis complicated by hypothermia. Emerg Med J 2002; 19: 169-71.
27.
Sibbald WJ, Doig G, Inman KJ. Sepsis, SIRS and infection. Intens Care Med 1995; 21: 299-301.
28.
Yaguchi A, Yuzawa J, Klein DJ, Takeda M, Harada T. Combining intermediate levels of the Endotoxin Activity Assay (EAA) with other biomarkers in the assessment of patients with sepsis: results of an observational study. Crit Care 2012; 16: R88.
29.
Zhang G, Wang T, An L, et al. U-shaped correlation of lymphocyte count with all-cause hospital mortality in sepsis and septic shock patients: a MIMIC-IV and eICU-CRD database study. Int J Emerg Med 2024; 17: 101.
30.
Yang J, Ma B, Tong H. Lymphocyte count trajectories are associated with the prognosis of sepsis patients. Crit Care 2024; 28: 399.
31.
Sheng S, Li A, Zhang C, et al. Association between hemoglobin and in-hospital mortality in critically ill patients with sepsis: evidence from two large databases. BMC Infect Dis 2024; 24: 1450.
32.
Peng H, Su Y, Luo J, Ding N. Association between admission hemoglobin level and prognosis in sepsis patients based on a critical care database. Sci Rep 2024; 14: 5212.
33.
Booke M, Sielenkämper A. Massivtransfusion mit dem Rapid Infusion System. Der Anaesthesist 2001; 50: 926-9.
34.
Challener D, Frank R, Kashani K, O’Horo J. Body temperature trends of critically Ill patients on continuous renal replacement therapy: a single-center retrospective study. Am J Med Sci 2022; 364: 404-8.
35.
Morsch CMF, Haas JS, Plotnick R, et al. Hypothermia related to continuous renal replacement therapy: incidence and associated factors. Crit Care Sci 2021; 33: 111-8.
36.
Warmerdam M, Stolwijk S, Boogert A, et al. Initial disease severity and quality of care of emergency department sepsis patients who are older or younger than 70 years of age. PLoS One 2017; 12: e185214.
37.
Michels EHA, Butler J, Reijnders TDY, et al. Association between age and the host response in critically ill patients with sepsis. Crit Care 2022; https://doi.org/10.21203/rs.3.....
38.
Martin GS, Mannino DM, Moss M. The effect of age on the development and outcome of adult sepsis. Crit Care Med 2006; 34: 15-21.
39.
Innocenti F, Tozzi C, Donnini C, et al. SOFA score in septic patients: incremental prognostic value over age, comorbidities, and parameters of sepsis severity. Intern Emerg Med 2017; 13: 405-12.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.