Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
ONCOLOGY / RESEARCH PAPER
HER2-Low Status in Breast Cancer: Clinicopathological Factors and Prognostic Value.
1
Maria Sklodowska-Curie National Research Institute of Oncology, Gliwice Branch, Poland
Submission date: 2024-11-22
Final revision date: 2025-02-27
Acceptance date: 2025-03-09
Online publication date: 2025-04-27
Corresponding author
Joanna Huszno
Maria Sklodowska-Curie National Research Institute of Oncology, Gliwice Branch, ul Wybrzeże Armii Krajowej 15, 44-101, GLIWICE, Poland
Maria Sklodowska-Curie National Research Institute of Oncology, Gliwice Branch, ul Wybrzeże Armii Krajowej 15, 44-101, GLIWICE, Poland
KEYWORDS
TOPICS
ABSTRACT
Introduction:
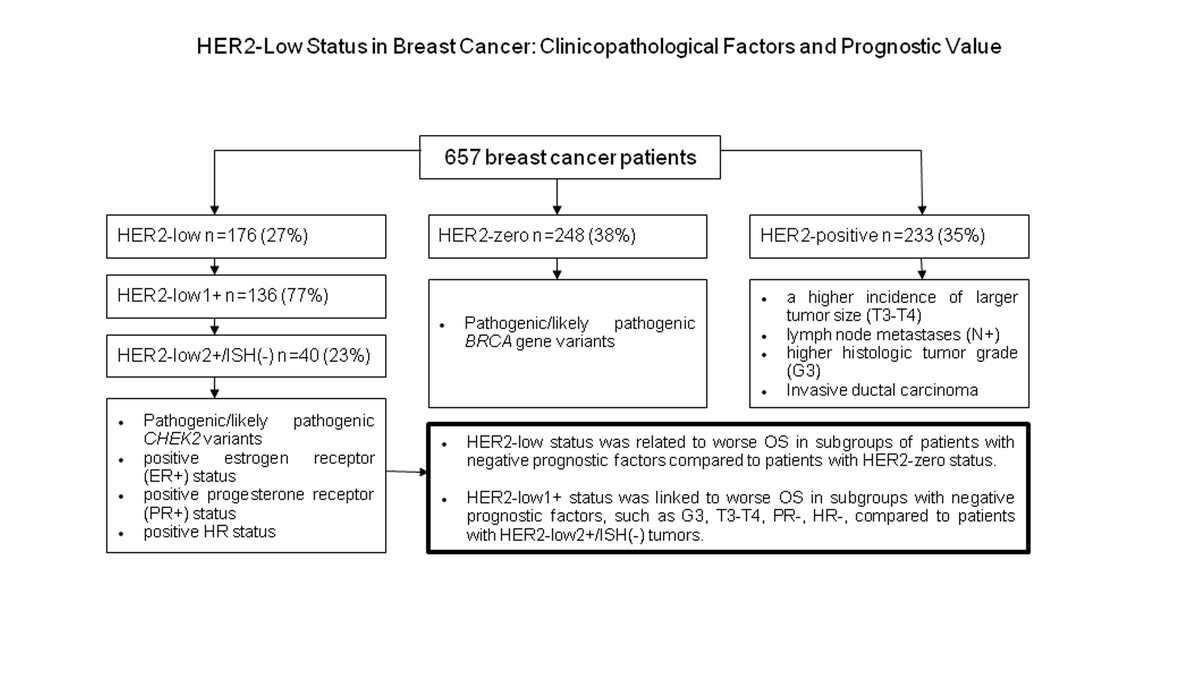
This study aimed to assess the prognostic importance of HER2-low status in breast cancer (BC). Additionally, we compared the HER2-low subgroup (defined as HER2-low1+; HER2-low2+/ISH(-)) with HER2-zero and HER2-positive subgroups according to clinical, histopathological and molecular features.
Material and methods:
The study analyzed the medical records of BC patients treated at the National Institute of Oncology in Gliwice, Poland, between 2002-2018. HER2 overexpression was assessed in postoperative specimens or samples obtained via core needle biopsy.
Results:
Of the 657 tumors, 176 (27%) tumors were classified as HER2-low BC, 248 (38%) as HER2-zero and 233 (35%) as HER2-positive tumors. BC patients with HER2-low tumors were more likely to have hormone receptor-positive (HR+) status compared to those with HER2-zero tumors (82.4% vs. 62.1%, P < 0.001). Specifically, patients with HER2-low1+ tumors had a higher frequency of HR+ status versus both HER2-zero and HER2-positive tumors. Similarly, patients with HER2-low2+/ISH(-) tumors were more frequently characterized as HR+ compared to HER2-zero and HER2-positive patients. In the subgroup of patients with estrogen receptor negative tumors, OS was slightly worse than for those with HER2-low status compared to HER2-zero patients (5-year OS 72.6% vs. 86.7%, P = 0.074). A tendency toward poorer OS was noted in HER2-low1+ patients with negative prognostic factors, including HR-, progesterone receptor-negative, grade 3, and larger tumors.
Conclusions:
HER2-low status appears to be associated with worse OS in breast cancer patients with certain negative prognostic factors versus HER2-zero status. Also, HER2-low1+ and HER2-low2+/ISH(-) subgroups were characterized by HR+ status.
This study aimed to assess the prognostic importance of HER2-low status in breast cancer (BC). Additionally, we compared the HER2-low subgroup (defined as HER2-low1+; HER2-low2+/ISH(-)) with HER2-zero and HER2-positive subgroups according to clinical, histopathological and molecular features.
Material and methods:
The study analyzed the medical records of BC patients treated at the National Institute of Oncology in Gliwice, Poland, between 2002-2018. HER2 overexpression was assessed in postoperative specimens or samples obtained via core needle biopsy.
Results:
Of the 657 tumors, 176 (27%) tumors were classified as HER2-low BC, 248 (38%) as HER2-zero and 233 (35%) as HER2-positive tumors. BC patients with HER2-low tumors were more likely to have hormone receptor-positive (HR+) status compared to those with HER2-zero tumors (82.4% vs. 62.1%, P < 0.001). Specifically, patients with HER2-low1+ tumors had a higher frequency of HR+ status versus both HER2-zero and HER2-positive tumors. Similarly, patients with HER2-low2+/ISH(-) tumors were more frequently characterized as HR+ compared to HER2-zero and HER2-positive patients. In the subgroup of patients with estrogen receptor negative tumors, OS was slightly worse than for those with HER2-low status compared to HER2-zero patients (5-year OS 72.6% vs. 86.7%, P = 0.074). A tendency toward poorer OS was noted in HER2-low1+ patients with negative prognostic factors, including HR-, progesterone receptor-negative, grade 3, and larger tumors.
Conclusions:
HER2-low status appears to be associated with worse OS in breast cancer patients with certain negative prognostic factors versus HER2-zero status. Also, HER2-low1+ and HER2-low2+/ISH(-) subgroups were characterized by HR+ status.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.